Abstract
The purpose of the present study was to determine the effect of biological in-growth and pre-tensioning on the load transmission function of meniscal transplants. The ability of meniscal transplants to transfer load to the tibial plateau was measured in an animal model. Thirty-six sheep were divided into six groups: group A was the sham group, in group B a medial meniscectomy was performed, and in groups C–F a medial meniscal transplantation with an autograft was carried out. In groups C–F, different levels of pre-tensioning force were applied via bone tunnel sutures (C=0, D=20, E=40, and F=60 N, respectively). The animals were killed after 6 months. The excised knees were mounted in a materials testing machine at 30, 60, and 90° of flexion, and loaded through the femoral axis to 500 N. A thin film pressure measuring transducer (K-scan, Tekscan®) was positioned underneath the meniscus in the medial compartment in order to determine contact area and pressure. The mean contact pressure (MCP) of the sham group (A) and the groups with the transplanted meniscus (C–F) was significantly lower in relation to the meniscectomized knees (B). Significant increases in contact area and reductions in peak contact pressure were also observed. Only the meniscal transplantation group with 40 N (E) pre-tension consistently showed a significant or strong trend toward increased contact area, compared to the meniscectomized knees (B) at all flexion angles tested. All meniscal transplanted groups with the exception of the 0 N group (C) showed a significant reduction in peak contact pressure in comparison to the meniscectomized group (B). The results indicate that meniscal transplantation reduces the MCP on the tibial plateau independent of the level of intraoperative pre-tensioning. Furthermore, the menisci pre-tensioned to 40 N showed significantly increased contact area and reduced peak contact pressure in comparison to the meniscectomized knees at all flexion angles tested, and revealed results similar to those reported in the literature for meniscal allografts fixated with bone plugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The menisci play an important role in the complex biomechanics of the knee joint. Loss of meniscal cartilage leads to degenerative arthritis [4, 21, 32, 33, 61]. To avoid degenerative changes due to loss of meniscal tissue, it is important to save the meniscus whenever possible. Meniscus repair has become a standard procedure. With the help of modern techniques the healing of the meniscus can be enhanced even in less vascularized areas of the meniscus, and the indications for meniscus repair could be extended [7, 20, 29, 35, 44, 45, 47, 49]. Partial resection of an injured meniscus should be as tissue-sparing as possible; nonetheless, not all damaged menisci can be treated by partial resection or by repair. The concept of meniscal replacement has thus been suggested, and the practice has become more common in recent years [42].
Different types of meniscus substitutes such as allografts, autografts (tendons, perichondral tissue), and biodegradable scaffolds [6, 17, 18, 25, 26, 36, 51, 56, 58, 59, 64, 67] have been experimentally and clinically used as meniscal replacement materials, and fresh frozen allografts as well as the cryopreserved allografts seem to provide the best prior conditions to prevent degenerative arthritis [48, 52].
Another factor affecting the ability of a meniscal transplant to restore normal contact mechanics at the time of implantation is the method of fixation to the surrounding tissues [2, 3, 19, 28, 46], and the problem of meniscal fixation is a frequently discussed subject in the field of meniscus transplantation [41]. Biomechanical investigations have shown that meniscal transplants require firm bony fixation in order to function well in load transmission, and that meniscal transplants fixed only with sutures were inferior with results similar to meniscectomized knees [2, 3, 19, 28, 46]. As a consequence of these studies, fixation with bone plugs has been favored by these investigators. Nonetheless, several important aspects were not considered in these studies: first, all experiments were done on cadaver knees—so that the influence of the biological in-growth could not be investigated; second, no information was provided regarding pre-tensioning of the meniscal transplant; and third, clinical studies using soft tissue fixation have reported better results than would be expected based on the results of biomechanical investigations alone [6, 63]. Furthermore, it is known that the natural meniscus needs a certain amount of movement to allow the equalization of the joint congruency between extension and flexion [62]. To our knowledge, no previous study has investigated the influence of pre-tensioning of meniscal transplants in an in vivo model, which have been allowed to bear weight for 6 months.
The purpose of the study was thus to investigate the effect of pre-tensioning and biological in-growth of meniscal transplants on the ability of the implant to transfer load to the tibial plateau in an animal experiment.
Materials and methods
Experimental design
Thirty-six sheep (Ovies aries) with an average mass of 68 kg (range 41–106 kg) were used in this animal study. The study was approved by the local animal use ethics committee according to federal German guidelines. The animals were between 2 and 4 years old at the time of surgery. The animals were randomly divided into six groups: group A was the sham group in which only the surgical approach to the knee joint with detachment of the medial collateral ligament was performed; in group B, a medial meniscectomy was performed; in groups C–F, a medial meniscal transplantation with an autograft was carried out. In groups C–F, different levels of pre-tensioning were applied to the meniscal transplant via bone tunnel sutures (C=0, D=20, E=40, and F=60 N, respectively). The animals were killed after 6 months, using an overdose of pentobarbital (150 mg/kg body weight). The right hind leg was disarticulated at the hip, the stability of the knee was evaluated by manual testing, and radiographs were taken. Afterwards, the legs were frozen at −20°C for later biomechanical analysis.
Surgical technique
The surgical procedure was performed under general anesthesia (Propofol 1.5–2.5 mg/kg intravenously and isoflurane/oxygen). The right hind leg was cleaned and draped in sterile fields in a sterile operating theater. Antibiotic prophylaxis with a penicillin–streptomycin combination (5–7.5 ml) was administered.
A medial parapatellar incision was used for arthrotomy. The patella was gently displaced laterally and the medial collateral ligament was explored. The medial collateral ligament was detached from its femoral insertion by means of a 1-cm2 bone block allowing full access to the medial compartment of the knee and the meniscus. In group A (sham group), the medial collateral ligament was reattached and the bone block was fixed using a washer and a 6.5-mm cancellous AO-screw (Synthes®, Switzerland) of 25 mm length. The joint capsule, retinaculum, and subcutaneous tissue were closed with absorbable sutures (Vicryl® 0 and 2, Ethicon, Norderstedt, Germany) and the skin with single stitches of non-resorbable suture (Ethilon® 2-0, Ethicon, Norderstedt, Germany). This same surgical approach was used in all animal groups investigated.
In addition, in the meniscectomy group, the meniscus was detached from its insertion ligament at the anterior and posterior horns and from the joint capsule with a scalpel. Before removing the meniscus, the exact insertion positions of the meniscus were marked with a sterile pen.
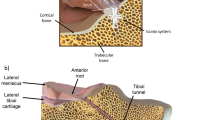
In the groups treated with autologous meniscal transplantation (groups C–F), the entire medial meniscus was removed and both ends of the meniscus were tagged with non-absorbable threads (Ethibond® 2, Ethicon, Norderstedt, Germany). The surgical approach was then distally extended to a length of about 5 cm and the proximal origin of the musculus tibialis cranialis was laterally separated from the proximal tibia. Two-millimeter diameter bone tunnels were drilled from the lateral surface of the tibia to the anterior and posterior insertions of the meniscal attachments with the help of an ACL drilling guide (Acufex®, Smith & Nephew, Andover, USA). The exact locations of the meniscus insertions were marked as described in the previous paragraph. The tag sutures were passed through the bone tunnels and the meniscus was pulled into the medial joint space. After passing the tag sutures through the tunnels, they were knotted tightly together and attached to a two-hole washer specially designed for this study. This washer had one hole for the suture and one hole for a 4.5-mm cortical AO-screw (Synthes®, Switzerland) to fix it to the proximal tibia (Fig. 1). Pre-tension was applied to the anchoring sutures by means of a tensiometer (Tension Isometer®, MEDmetric Corp., San Diego, CA, USA) according to the study protocol (groups C=0, D=20, E=40, and F=60 N) (Figs. 2, 3). The position of the drill hole for fixation of the washer was more distal or more proximal on the tibia depending on the amount of applied load. The meniscus was sutured to the capsule with six absorbable sutures (Vicryl® 2, Ethicon, Norderstedt, Germany). Finally, the medial collateral ligament was reattached and wound closure followed as described earlier.
Washer plate was specially designed for this study. The tag sutures of the meniscal transplant were knotted through the smaller hole. The bigger hole was used for fixation with a 4.5-mm AO cortical screw after tensioning the tag sutures. The spikes were pushed into the tibial periosteum to ensure proper plate fixation
The animals were allowed immediate free movement and weight bearing post-operatively and were not restricted in any way. The animals were kept in cages with four animals per cage for the first 2 weeks after which the skin sutures were removed and the animals were allowed to roam freely in a herd with sufficient space for running. Wound healing and gait were examined daily, and prophylactic antibiotics (5–7.5 ml penicillin–streptomycin combination) were given for 2 days post-operatively. All animal care was undertaken in accordance with the guidelines of the animal laboratory and under supervision of a veterinarian team.
Evaluation of the specimen
The specimens were thawed gradually at room temperature. The patella and all muscle were removed with careful attention to ensure that the collateral and cruciate ligaments were left intact. The femur was transected 10 cm and the tibia 15 cm below the joint line potted in aluminum cylinders with a cold-curing methylmethacrylate resin (Technovit 4004, Heraeus Kulzer GmbH, Wehrheim, Germany). A uniaxial materials testing machine (Zwick GmbH Co., Ulm, Germany) was used to apply compressive loads on the knees. A hinge joint on the femoral side of the mounting fixture allowed reproducible selection of various flexion angles (Fig. 4), of which 30, 60, and 90° were investigated. The tibial cylinder rested on a linear motion x–y table allowing translation motion in the plane perpendicular to the axis of loading. After mechanical alignment of the knee, using a functional axis approach, the tibia was firmly fixed in position and loading applied (Fig. 4). The specimens were kept moist throughout the test with isotonic NaCl solution.
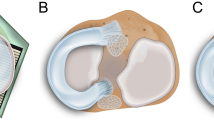
Contact pressure and area were measured with an electronic resistive pressure-measuring sensor (K-scan #4000, Tekscan, Boston, MA, USA). The sensor used has a size of 28×33 mm2 and thickness of 0.1 mm. One sensor contains 26 rows and 22 columns of sensor elements providing 572 sensing locations referred as “sensels”. The K-scan sensors were pre-conditioned and calibrated according to the manufacturer’s guidelines. To protect the film during repeated measurements, a thin Teflon film of 0.1 mm thickness was applied [60]. The sensors were trimmed according to the widths of the slits to allow insertion and further encased in a thin layer of self-adhesive cellophane film to prevent moisture from entering. For inserting the film beneath the meniscus, slits were made through the capsular attachments of the medial meniscus anteriorly and posteriorly from the meniscal horns to the medial collateral ligament [16]. This technique of inserting the sensors beneath the meniscus was previously described by Baratz et al. [10] as minimally disruptive of the joint capsule and supporting ligaments and was reported to produce no measurable change in the loading characteristics of the knee [40]. By using this insertion technique, the medial tibial plateau was completely covered by the pressure-sensitive film. This allowed the calculation of the contact area by summing up the areas of the sensels (sensor elements) recording contact under a given loading condition.
To ensure reproducible loading during testing, the specimens were first subjected to five cycles of 500 N pre-conditioning loading before joint pressure was measured. For the testing itself, a constant load of 500 N was applied for 10 s. The contact area, peak contact, and mean contact pressure (MCP) on the tibial plateau were recorded at 30, 60, and 90° of knee flexion. Statistical analysis was performed using the Mann–Whitney test for non-parametric unpaired groups at a significance level of P≤0.05.
The biomechanical testing was one of several tests to which the knees were subjected. The other tests included gross inspection and histological evaluation of the cartilage.
Results
There were no intra- or early post-operative complications. It was possible to biomechanically evaluate five of the six operated knees in each group. Reasons for exclusions were as follows: intra-articular infection which had completely destroyed the articular cartilage in three specimens; instability problems caused by an incompletely healed medial collateral ligament in two cases; and one patella dislocation which also caused degenerative changes.
Mean contact pressure
The MCP of the sham group (A) and the groups with the transplanted medial meniscus (C–F) was significantly lower in comparison to the meniscectomized knees (B), independent of the applied pre-tension on the meniscal transplant and the position of the knee (Table 1, Fig. 5). Significant differences between the single transplantation groups and/or the sham group were not observed.
Contact area
In the intact knee (A), mean total contact area of the medial compartment was 260.9, 254.1, and 241.3 mm2 at 30, 60, and 90° of knee flexion, respectively (Table 2). After total meniscectomy (B) the contact area significantly decreased by 53.2% at 30°, 56.9% at 60°, and 53.5% at 90°. Contact area was observed to be lower in all meniscal transplantation groups (C–F) with values relative to the sham control ranging from 14.2 to 29.9% at 30°, 18.5 to 31.8% at 60°, and 18.2 to 32.5% at 90° flexion. Thus, with the exception of the 40 N (30°; 60°) and the 0 N (60°) pre-tension groups, all groups demonstrated a significant (or tended to) decrease in comparison to the sham control group.
The differences in comparison to the meniscectomy group, as the worst possible case, were dependent on the degree of knee flexion. Thus, at 30° of flexion almost all groups (C–F) showed a significant increase of the contact area in comparison to the meniscectomy group (B). For the transplanted groups with 20 N (D) and 60 N (F) pre-tension, a strong trend for an increase was found (Figs. 6, 7). At greater flexion angles, only the meniscal transplantation group with the 40 N constantly showed a significant increase of the contact area (P=0.028 at 90°) and/or a very strong trend (P=0.076 at 60°) in relation to the meniscectomized knees. While no significant increase in contact area was observed in the 0 N intraoperative pre-tension (C) group at 60 and 90° of flexion, strong tendencies (P<0.1) toward increased contact areas were observed in the 20 and 60 N pre-tension groups at 90° of flexion.
Peak contact pressure
Peak contact pressure in the intact knees (A) (Table 3, Fig. 8) was 2.71, 2.74, and 3.32 MPa at 30, 60, and 90° of knee flexion. In the meniscectomized knees, an average increase of contact pressure of 260.4% was observed. All meniscal transplanted groups with the exception of the 0 N pre-tension group (C) showed persistently in all flexion positions a significant reduction in comparison with the meniscectomized group (B), and none of the transplanted groups showed significant increases in relation to the sham group (A).
Discussion
The purpose of the study was to investigate the effect of biological in-growth and implant pre-tensioning on the load transmission function of meniscal transplants. The ability of meniscal transplants implanted with suture fixation and without bone plugs to distribute load on the tibial plateau was measured in a sheep animal model. By using an autograft instead of an allograft, the effects of fixation were isolated from other confounding factors such as immunological reactions, differences in meniscus size, shape, and mechanical properties between donor and original menisci. Variability in positioning was minimized by marking the original insertion points before the meniscus was resected and drilling the bone tunnels at the anterior and posterior horns at these points. Flexion angles of 30, 60, and 90° were tested. The 0° position was not tested because the 30° flexion position was the maximal extension that could be achieved with the sheep specimen.
Several issues were considered in the selection of a compressive load for this study. Ideally, the applied compressive load should have been between 1,800 and 2,000 N (2.5 times body weight) to approximate the load across the knee during walking [2, 43]. In previous studies the authors found that the compressive load transmitted from femur to tibia attained five to six times body weight [39]. As early as 1891, Braune and Fischer demonstrated that the femorotibial contact area is much larger in a loaded than in an unloaded knee [13, 39]. In addition, a recent biomechanical study in human cadaveric knees demonstrated that the level of compressive load affects conclusions from statistical analysis whether a lateral meniscal autograft can restore normal tibial contact pressure. The differences between 400 and 1,200 N were significant [30].
In the majority of biomechanical studies dealing with load distribution on the tibial plateau, human cadaveric knees were used [1, 5, 8, 9, 11, 14, 15, 23, 31, 34, 37–40, 46, 53–55, 57, 65, 66]. But what about tetrapods? Only two biomechanical studies on knee joint contact pressure utilizing an animal experiment with goats or sheep were found [12, 16]. In the study of Bylski-Austrow et al. [16], biomechanical testing of the knee was performed at loads of twice the body weight (1,240±190 N). The reason for this choice of compressive load was not discussed in detail; perhaps it was used to enable a comparison with the human knee joint. Bellenger and Pickles [12] used compressive loads between 57 and 495 N in their sheep model. Because of this and the smaller size of the tibial head and the femoral condyles in comparison to the human knee, we decided to use 500 N as a compressive load for the present study.
We used the Tekscan system for pressure measurement. A comparative study between the Tekscan and the FUJI® system that was used in most of the biomechanical studies [2, 40, 46] reveals several advantages of the electronic sensor. The Tekscan system was suitable for dynamic measurement in the femorotibial joint, the reproducibility of the data was significantly higher, and it proved to be more reliable [27, 60, 68]. The capability for dynamic measurement presents the advantage that the sensors needed not be changed for measuring the different flexion positions of the knee joint as was done in the present study. The risk of damaging the articular cartilage and otherwise damaging the specimen by repeatedly inserting a pressure sensor film was thus reduced.
According to the literature, the decrease in contact area from intact knee joints to meniscectomized knee joints ranges from 30 to 80% [1, 2, 10, 14, 23, 34, 37–39, 46, 54, 65, 66]. The data of the present study fall within this range, with reductions of 53.2, 56.9, and 53.5% in contact area of the meniscectomized knee observed relative to the sham control at 30, 60, and 90° of flexion, respectively. Comparisons of the magnitude of the contact area itself are generally not possible since in most human cases human cadaveric specimens were used.
After meniscal allograft transplantation with bone plugs, a decrease of 17–23% in contact area was reported in the study of Paletta et al. [46]. With detachment of the anterior and posterior horns of the meniscus, a decrease of 45–48% was observed. Comparing the results of Paletta et al. [46] with the present study, we found a comparable reduction in contact area in relation to the intact meniscus for the 40 N meniscal transplantation group (E) (16.2–21.2%). However, all meniscal transplantation groups (C–F), independent of the level of pre-tension, showed better results with regard to the contact area in comparison to the meniscal allograft with the detached anterior and posterior horns in that study [46]. These results support the hypothesis that the biological in-growth improves the biomechanical function of the meniscus. In the study of Alhaki et al. [2], all three fixation methods (meniscal transplants with bone plugs, meniscal transplants with bone plugs and suture, and meniscal transplants with sutures only) restored the mean contact area to normal, but there was large variability in the data. In a cadaver study, Chen et al. [19] demonstrated that the total contact area of the meniscal transplantation with bone bridge or with both horns secured showed no significant difference to the intact knee joint. However, investigations of contact area and pressure should take the healing and in-growth process into consideration. In the present study, the biomechanical analysis was performed 6 months post-operatively. During this time, biological processes such as remodeling, healing, and inflammation of the bone and soft tissue takes place, which can alter the contact area observed immediately post-operatively and may lead to conclusions different from the purely in vitro cadaver studies. Bylski-Austrow et al. [16] demonstrated this effect in their biomechanical study by measuring the knee joint contact pressure after chronic meniscectomy relative to acutely meniscectomized joints in an animal model at 4 and 8 months post-meniscectomy. It was observed that the peak contact pressure is consistently high in chronic meniscectomized knees, which suggests that this parameter is important.
Previous studies of human cadaver knees found increases in contact pressure ranging from 117 to 400% of normal for the meniscectomized knee joint. These results depended on the applied compressive load ranging from 310 to 2,500 N [1–3, 10, 19, 23, 37, 38, 46, 50, 54, 55]. Our results for the peak contact pressure with an average increase of 260.4% for the meniscectomized knee compared to the intact knee fit well into this admittedly very large range.
With regard to meniscal transplantation groups, Paletta et al. [46] found a significant increase in peak contact pressure of 36 and 80% for the allografts with bone plugs in comparison to the intact knee joint. With release of the anterior and posterior horns, there was a further increase in peak contact pressure to 220–360% in comparison to the intact joint. In the study of Chen et al. [19], the meniscal transplanted knee with both horns secured or bone bridge had 8–12% more peak contact pressure in comparison to the intact joint. Peak contact pressure in the meniscal transplanted groups with neither or only one horn secured was 39–53% more. Alhaki et al. [2] also found significant increases in maximum pressure with suture fixation alone. In the present study, contact pressure increases ranging from 7 to 53% were observed for the pre-tension groups (D–F, 20–60 N), which is equal to or even better than the results observed for bone plug fixation by Paletta et al. [46]. This further supports the hypothesis that the biological in-growth and pre-tensioning improve the biomechanical load-transferring function of the meniscal transplant.
With regard to the different meniscal transplantation groups (C–F), only the 40 N pre-tension meniscal transplanted group consistently showed improvement relative to the meniscectomized knees throughout all flexion angles for contact area and the peak contact pressure. We speculate that 40 N pre-tension is enough to provide for load transmission function of the meniscus while still allowing the equalization of the congruency between the femoral condyles and the tibial plateau during extension and flexion. The fixation of a meniscal transplant with a pre-tension of 0 and 20 N seems too low and may lead the meniscus being extruded out of the joint space at higher flexion angles. This effect could possibly be compared with the medial placement of the posterior horn in the study of Sekaran et al. [55]. The medial mal-position of that study caused the meniscal transplant to displace toward the periphery of the joint, with the consequence that the meniscus became slack circumferentially. Inasmuch as the circumferential tensile modulus has been shown to be an important determinant of meniscal load sharing [22], introducing slackness circumferentially with mal-positioning or low tension caused decreased load-sharing on the part of the meniscus [55]. Gao et al. [24] supported this hypothesis by demonstrating in rabbits that after transection and refixation of the anterior attachment, the meniscus healed in a prolonged position, which reached not more than 20% of the failure load compared to the normal attachment at tensile testing. This is partly in accordance with the study of Haut [28] who investigated the stiffness of meniscal attachments and meniscal material properties affecting tibiofemoral contact pressure using a validated finite element model of the human knee joint. The contact pressure was sensitive to the circumferential modulus and horn stiffness, but once again the influence of pre-tensioning and biological in-growth was not considered. On the other hand, the results of the present study suggest that pre-tensioning with 60 N appears to be too high, and that the meniscal transplant may be so firmly pulled against the tibia such that it can no longer equalize the incongruence between the femoral condyle and the tibial plateau. In this connection it should be mentioned that it is not clear how long the intraoperative tension applied on the sutures is maintained post-operatively as healing progresses. Unfortunately, we could not find any method to measure the relaxation effect directly in the animals. Furthermore, no clear conclusions about the state of the sutures at harvest could be made; since suture was observed in a variety of states at harvest (intact, partially ruptured, ruptured) we could not draw any clear conclusion from this.
Conclusion
In summary, we conclude that biological in-growth and the intraoperative pre-tensioning of meniscal transplants has an influence on the biomechanical load-transferring function of meniscal transplants. In this animal model, and with the compressive load of 500 N, meniscal transplantation reduces the MCPs independent of the level of pre-tensioning. Furthermore, contact area and peak contact pressure in the 40 N pre-tensioned meniscal transplantation group showed significantly better results in comparison to the meniscectomized knees over all flexion angles tested. Compared to the results reported in the literature, the 40 N pre-tensioning group performed similarly to meniscal allografts fixated with bone plugs. Nonetheless, the clinical implications of the results of this experimental animal study should not be overestimated. When interpreting the results of this study, it should be remembered that the study was performed with an autograft as an ideal meniscal transplant. Several additional problems not present in our idealized graft model are associated with the allografts contemporarily finding clinical use. While the results of this animal study suggest that suture fixation with pre-tensioning may improve clinical results in human patients, further carefully designed studies will be necessary to verify this hypothesis and prove whether or not the technique can indeed prevent or reduce degenerative changes in completely meniscectomized knees.
References
Ahmed A, Burke DL (1983) In-vitro measurement of static pressure distribution in synovial joints. Part I: Tibial surface of the knee. J Biomech Eng 105:216–217
Alhaki M, Howell S, Hull ML (1999) How three methods for fixing a medial meniscus autograft affect tibial contact mechanics. Am J Sports Med 27:320–328
Alhaki M, Hull ML, Howell S (2000) Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft. Am J Sports Med 28:370–376
Allen P, Denham R, Swan A (1984) Late degenerative changes after meniscectomy. J Bone Joint Surg (Br) 66B:666–671
Andrish J, Kambic H, Valdevit A, Kuroda R, Parker R, Aronowitz E, Elster T (2001) Selected knee osteotomies and meniscal replacement: effects on dynamic intra-joint loading. J Bone Joint Surg (Am) 83-A:142–150
Arkel van E, Boer de H (2002) Survival analysis of human meniscal transplantations. J Bone Joint Surg (Br) 84B:227–231
Arnoczky S, Warren S, Spivak J (1988) Meniscal repair using and exogenous fibrin clot. J Bone Joint Surg (Am) 70A:1209–1217
Atheshian G, Soslowsky L, Mow V (1991) Quantitation of articular surface topography and cartilage thickness in knee joints using stereophotogrammetry. J Biomech 24:761–776
Bach J, Hull M (1995) A new load application system for in vitro study of ligamentous injuries to the human knee joint. J Biomech Eng 117:373–382
Baratz M, Fu F, Mengato R (1986) Meniscal tears: the effect of meniscectomy and of repair on the intraarticular contact areas and stress in the human knee. Am J Sports Med 14:270–275
Baratz M, Rehak DC, Fu F, Rudert MJ (1988) Peripheral tears of the meniscus. Am J Sports Med 16:1–6
Bellenger C, Pickles D (1993) Load-bearing in the ovine medial tibial condyle: effect of meniscectomy. Vet Comp Orthop Traumatol 6:100–104
Braune W, Fischer O (1891) Die Bewegungen des Kniegelenkes nach einer neuen Methode an lebenden Menschen gemessen. Abh Math Phys Classe Königl Sächsischen Ges Wiss 17:75–150
Brown T, Shaw D (1984) In vitro contact stress distribution on the femoral condyles. J Orthop Res 2:190–199
Bylski-Austrow D, Ciarelli M, Kayner D, Matthews L, Goldstein S (1994) Displacements of the menisci under joint load: an in vitro study in human knees. J Biomech 27:421–431
Bylski-Austrow D, Malumed J, Meade T, Grood E (1993) Knee joint contact pressure decreases after chronic meniscectomy relative to the acutely meniscectomized joint: a mechanical study in goat. J Orthop Res 11:796–804
Cameron J, Saha S (1997) Meniscus allograft transplantation for unicompartimental arthritis of the knee. Clin Orthop 337:164–171
Carter T (1999) Meniscal allograft transplantation. Sports Med Arthrosc Rev 7:51–62
Chen M, Branch T, Hutton W (1996) Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 12:174–181
Cook J, Tomlinson J, Arnoczky S, Fox D, Cook C, Kreeger J (2001) Kinetic study of the replacement of porcine small intestinal submucosa grafts and the regeneration of meniscal-like tissue in large avascular meniscal defects in dogs. Tissue Eng 7:321–334
Fairbank T (1948) Knee joint changes after meniscectomy. J Bone Joint Surg (Br) 30B:664
Fithian D, Kelly M, Mow V (1990) Material properties and structure–function relationship in the menisci. Clin Orthop 252:19–31
Fukubayashi T, Kurosawa H (1980) The contact area and pressure distribution pattern of the knee. Acta Orthop Scand 51:871–879
Gao J, Wei X, Messner K (1998) Healing of the anterior attachment of the rabbit meniscus to bone. Clin Orthop 348:246–258
Garrett J (1993) Meniscal transplantation: a review of 43 cases with 2- to 7-year follow-up. Sports Med Arthrosc Rev 1:164–167
Groff Y, Urquart M, Irrgang J, Fu F, Harner C (2001) Lateral meniscus transplantation: the University of Pittburgh experience. Pittburgh Orthop J 12:134–140
Harris M, Morberg P, Bruce W, Walsh W (1999) An improved method for measuring tibiofemoral contact areas in total knee arthroplasty: a comparison between K-scan sensors and Fuji film. J Biomech 32:951–958
Haut T, Hull M, Rashid M, Jacobs C (2003) How the stiffness of meniscal attachments and meniscal material properties affect tibiofemoral contact pressure computed using a validated finite element model of the human knee joint. J Biomech 36:19–34
Henning C, Lynch M, Yearout K, Vequist S, Stallbaumer R, Decker K (1990) Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop 252:64–72
Huang A, Hull M, Howell S (2003) The level of compressive load affects conclusions from statistical analysis to determine whether lateral meniscal autograft restores tibial contact pressure to normal: a study in human cadaveric knees. J Orthop Res 21:459–464
Huang A, Hull M, Howell S, Donahue T (2002) Identification of cross-sectional parameters of lateral meniscal allografts that predict tibial contact pressure in human cadaveric knees. J Biomech Eng 124:481–489
Johnson R, Kettelkamp D, Clark W, Leaverton P (1974) Factors affecting late results after meniscectomy. J Bone Joint Surg (Am) 56A:719–729
Kenny C (1997) Radial displacement of the medial meniscus and Fairbank’s signs. Clin Orthop 339:163–173
Kettelkamp D, Jacobs A (1972) Tibiofemoral contact area—determination and implications. J Bone Joint Surg (Am) 54A:349–356
Kobuna Y, Shirakura K, Niijima M (1995) Meniscal repair using a flap of synovium. Am J Knee Surg 8:52–55
Kohn D (1993) Autograft meniscus replacement: experimental and clinical results. Knee Surg Sports Traumatol Arthrosc 1:123–125
Krause W, Pope M, Johnson R (1976) Mechanical changes in the knee after meniscectomy. J Bone Joint Surg (Am) 58A:599–604
Kurosawa H, Fukubayashi T (1980) Load-bearing mode of the knee joint. Clin Orthop 149:283–290
Maquet P, Van de Berg A, Simonet J (1975) Femorotibial weight-bearing areas. J Bone Joint Surg (Am) 57A:766–771
Martens T, Hull M, Howell S (1997) An in vitro osteotomy method to expose the medial compartment of the human knee. J Biomech Eng 119:379–385
Messner K, Verdonk R (1999) Is it necessary to anchor the meniscal transplants with bone plugs? Scand J Med Sci Sports 9:186–187
Milachowski K, Weismeier K, Wirth C (1989) Homologous meniscus transplantation. Int Orthop 13:1–11
Morrison J (1969) Function of the knee joint in various activities. Biomed Eng 4:573–580
Ochi M, Mochizuki Y, Deie M, Ikuta Y (1996) Augmented meniscal healing with free synovial autografts: an organ culture model. Arch Orthop Trauma Surg 115:123–126
Okuda K, Ochi M, Shu N, Uchio Y (1999) Meniscal rasping for repair of the meniscal tear in the avascular zone. Arthroscopy 15:281–286
Paletta G, Manning T, Snell E, Parker R, Bergfeld J (1997) The effect of allograft meniscal replacement on the intra-articular contact area and pressures in the human knee. Am J Sports Med 25:692–698
Peretti G, Caruso E, Randolph M, Zaleske D (2001) Meniscal repair using engineered tissue. J Orthop Res 19:278–285
Peters G, Wirth C (2003) The current state of meniscal allograft transplantation and replacement. Knee 10:19–31
Port J, Jackson D, Lee T, Simon T (1996) Meniscal repair supplemented with exogenous fibrin clot and autogenous cultered marrow cells in the goat model. Am J Sports Med 24:547–555
Radin E, De Lamotte F, Maquet P (1984) Role of the menisci in the distribution of stress in the knee. Clin Orthop 185:290–294
Rath E, Richmond J, Yassier W, Albright J, Gundogan F (2001) Meniscal allograft transplantation. Two- to eight year results. Am J Sports Med 29:410–414
Rodeo S (2001) Meniscal allografts—where do we stand? Am J Sports Med 29:246–261
Schreppers G, Sauren A, Huson A (1991) A model of force transmission in the tibio-femoral contact incorporating fluid and mixtures. Proc Inst Mech Eng 205:233–241
Seedhom B (1979) Transmission of the load in the knee joint with special reference to the role of the menisci. Eng Med 8:207–228
Sekaran S, Hull M, Howell S (2002) Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects pressure distribution on the tibial plateau. Am J Sports Med 30:74–82
Sekiya J, Giffin J, Irrgang J, Fu F, Harner C (2003) Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med 31:896–906
Shrive N (1978) Load-bearing in the knee joint. Clin Orthop 131:279–287
Stollsteimer G, Shelton W, Dukes A, Bomboy A (2000) Meniscal allograft transplantation: a 1- to 5-year follow-up of 22 patients. Arthroscopy 16:343–347
Stone K, Steadman J, Rodkey W, Li S (2002) Regeneration of meniscal cartilage with the use of a collagen scaffold. J Bone Joint Surg (Am) 79A:1770–1777
Stukenborg-Colsman C, Ostermeier S, Hurschler C, Wirth C (2002) Tibiofemoral contact stresses after total knee arthroplasty. Acta Orthop Scand 73:638–646
Tapper E, Hoover N (1969) Late results after meniscectomy. J Bone Joint Surg (Am) 51A:517–526
Thompson W, Thaete F, Fu F, Dye S (1991) Tibial meniscal dynamics using three dimensional reconstruction of magnetic resonance images. Am J Sports Med 19:210–216
Verdonk R (1997) Alternative treatments for meniscal injuries. J Bone Joint Surg (Br) 79B:873
Verdonk R (2002) Meniscal transplantation. Acta Orthop Belg 68:118–127
Walker P, Erkman M (1975) The role of the menisci in force transmission across the knee. Clin Orthop 109:184–192
Walker P, Hajek J (1972) The load-bearing area in the knee joint. J Biomech 5:581–589
Wirth C, Peters G, Milachowski K, Weismeier K, Kohn D (2002) Long-term results of meniscal allograft transplantation. Am J Sports Med 30:174–181
Wirz D, Becker R, Li S, Friedrich N, Muller W (2002) Validation of the Tekscan system for static and dynamic pressure measurements of the human femoraltibial joint. Biomed Technol 47:195–201
Acknowledgements
This study was supported by the “Hochschulinterne Leistungsförderung” of the Hannover Medical School, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
von Lewinski, G., Hurschler, C., Allmann, C. et al. The influence of pre-tensioning of meniscal transplants on the tibiofemoral contact area. Knee Surg Sports Traumatol Arthrosc 14, 425–436 (2006). https://doi.org/10.1007/s00167-005-0704-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-005-0704-z