Abstract
The existence of meniscal extrusion is well known in the natural history of the osteoarthritic knee. However, extruded menisci are also seen in non-pathologic knees. To ascertain the prevalence of meniscal extrusion in non-arthritic patients, the MRIs of 100 knees were prospectively studied. The data were correlated both with clinical and operative arthroscopic findings. The results showed 68.5% of the medial menisci to have some degree of extrusion, averaging at 28% of the meniscal size. While the lateral meniscus were extruded in 18.8% of cases at an average of 15% of the meniscal size. Furthermore, a relationship between the anterior insertion variant of the anterior medial meniscus and meniscal extrusion was found (P=0.001) in this series. The results suggest meniscal extrusion to be much more common in non-arthritic knees than previously estimated. The results also suggest that when the anterior horn of the medial meniscus inserts anteriorly in the tibial plateau, the meniscus tends to be extruded. It must be kept in mind that one of the limitations of this work is that the MRIs are taken in a non-weightbearing position.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal extrusion is defined as the situation in which the meniscus is partially or totally luxated from the tibial plateau [7]. It has been suggested that upon extruding the meniscus leaving the articular surface of the tibia uncovered, it would partially stop fulfilling its functions. Neither would it absorb the loads applied on the tibial cartilage. It would decrease the contact area and increase the degree of joint instability. Thereby, the aforementioned would simulate a condition of a total meniscectomy. This situation might favor progression toward osteoarthritis [6, 8].
Meniscal extrusion is a known fact in the natural history of the degeneration of the arthritic knee [1, 7]. However, there is little evidence with respect to the incidence of meniscal extrusion in the normal population. Furthermore, there is no agreement with respect to the amount of meniscal subluxation that can be considered as physiological. Some authors have accepted up to 3 mm of meniscal subluxation as normal [11].
It has also been suggested that some variations in meniscal insertions may contribute to the extrusion of the menisci especially in the medial compartment [3].
The aim of this work is to ascertain the prevalence of meniscal extrusion in non-arthritic patients who have undergone arthroscopic surgery as well as to define those factors related to it. Special attention was given to the fact of anatomic variations in the menisci attachments.
Methods
The files and knee MRI of 100 non-advanced arthritic consecutive patients that were operated on arthroscopically, in our institution, were prospectively studied.
Inclusion criteria
The study included those non-arthritic knees operated on for any disorder other than a meniscal pathology. This was done in order to avoid a known cause of extrusion as it has been demonstrated that a torn menisci does not resist hoop stress [8].
Seventy-two males and 28 females, average age of 36.6 years (range between 13 and 64), entered in the study. There were 43 right-knees and 57 left-knees. The average weight of the patients was 77 kg (range 44–135).
We recorded data such as prior surgeries, clinical symptoms, and degrees of arthritic changes according to the Ahlback score. Arthroscopic data relative to the operated knees was also recorded. That included data on the menisci anatomy, special attention paid to variations of the horn attachments, ligament status, and chondral lesions (outerbridge grade, size of the affected area, and localization).
Of the 100 medial and 100 lateral menisci initially considered for study, 46 medial and 17 lateral had to be excluded from it for having sustained injuries that were subsequently confirmed at surgery. Therefore, the final series was composed of 54 medial menisci and 83 lateral menisci ready for evaluation.
MRI evaluation
Each case underwent MRI of the affected knee. All studies were performed with a superconductive 1.9 T system (Prestige 2T, Elscint, Haifa, Israel) with a quadrature extremity coil. A positioning device for the ankle was used to ensure uniformity between patients. The standard knee protocol for each subject consists of a sagittal fat-saturated proton density-weighted sequence, a coronal T1-weighted sequence, a coronal Stir-weighted sequence, and an axial fat-saturated proton density-weighted sequence. Slice thicknesses of 3 mm with no intersection gap were used.
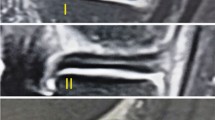
MRIs of the cases were evaluated by only one reader (MC), which was blinded to case status. Meniscal extrusion was measured on the coronal images using an MRI-generated scale on each image. According to Gale et al. [7] meniscal extrusion was defined as the greatest distance from the most peripheral aspect of the meniscus to the border of the tibia excluding any osteophyte. After looking at all of the coronal cuts of each knee, measures were taken in those images were extrusion was maximum. In order to standardize the results, each measure of extrusion was divided by the total width of the meniscus in the same MRI image (Fig. 1).
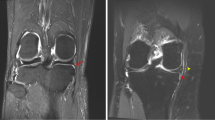
We also recorded the type of anterior horn insertion of the medial meniscus based on what was seen in the sagittal images. From an anatomical point of view, four types of anterior horn insertions can be identified according to Berlet and Fowler [3]. However, it was extremely difficult to identify more than two types in an MRI in the current study. Therefore, the anterior horn insertions were classified into anterior and posterior variants (Fig. 2). All these data were correlated with the MRI coronal images as well as with the arthroscopic findings (Fig. 3).
Statistical analysis
The statistical analysis was done with the SPSS computer program for Windows. In order to analyze the non-parametric variables, the Mann–Whitney test was used. The level of statistical significance was set at P≤0.05.
Results
The clinical and arthroscopic findings are shown in Tables 1, 2, and 3. With reference to conventional X-ray, 46 cases corresponded to Ahlback’s grade 0, 25 cases to grade I, and 2 cases to grade II.
In terms of the medial meniscus, 37 cases (68.5%) showed some degree of extrusion, averaging at 28% of the meniscal size (ranging from 10 to 60%). In the case of the lateral meniscus, extrusion averaged 15% (ranging from 10 to 40%) and was seen in 15 cases (18.8%).
In this series, the posterior insertion variant of the anterior medial meniscus was the most frequently found (69.5%). The remaining 31.5% presented an anterior type of insertion.
From the statistical point of view, medial meniscal extrusion was significatively correlated to the presence of a chondral lesion (P=0.008) and to an anterior variant of the medial meniscus insertion (P=0.001). No statistically significant relationship to the rest of the parameters studied was encountered. None of the parameters studied were related to lateral meniscus extrusion.
Discussion
In the current work, the data on meniscal extrusion was not presented as in absolute values but as a measure percentage of the menisci that pass the tibial plateau limit. This was done in order to standardize them to the different sized knees.
The results suggest that meniscal extrusion is frequent in non-arthritic knees. This fact has been seen with greater frequency in the medial (68%) rather than in the lateral meniscus (18.8%). The relationship between meniscal extrusion and the arthritic knee is well known and it might be produced by laxity in the meniscal support structures. Gale et al. [7] correlated, via MRI, the amount of meniscal subluxation with the narrowing of the joint line. Adams et al. [1] even suggested this joint narrowing was due to meniscal extrusion more than to cartilage wear in patients with incipient degenerative knee changes. More recently, Bennett and Buckland-Wright, using a system of macroradiography with double contrast, demonstrated that the initial narrowing is a combination of meniscal and cartilage wear [2]. Therefore, it seems clear that meniscal extrusion is a phenomenon that comes about during the natural history of knee joint degeneration whatever the cause or the consequence of the initial joint collapse.
However, there are situations in which menisci can subluxe independently of an arthritic condition. Breitenseher et al. [4] failed to encounter meniscal subluxation, defined as more than 3 mm, in any of the cases of an MRI study on ten asymptomatic volunteers. The average distance from the medial meniscus insertion rim to the tibial plateau was 0.07 mm and for the lateral meniscus it was 0 mm. There was evidence of subluxation in 8% of the patients with symptoms in the knee. Thus, they related this finding with the presence of joint effusion or arthritis [4]. On the contrary, Gale et al. [7] encountered meniscal extrusion of more than 3 mm in 64% of the patients in their study. The aforementioned group consisted of women of more than 50 years of age and men more than 40 years old [7]. Verdonk et al. [10] came upon an average of 0.8 mm of lateral meniscal extrusion in ten patients with normal knees in a comparative study of normal and transplanted menisci.
The relationship between meniscal extrusion and chondral lesions has already been shown in transplanted meniscal allografts [9]. Fourteen out of 29 transplants showed meniscal extrusion in this series. A chondral lesion of the affected compartment showed up in all these cases. In our series, medial meniscus subluxation only correlated with the presence of chondral lesions in the medial compartment and with anterior insertion types of the anterior horn of the medial meniscus.
Berlet and Fowler hypothesized that the loaded medial meniscus with an anterior type of insertion cannot resist peripheral extrusion. However, there was no proof of the relationship between meniscal extrusion and anatomical insertion variant anomalies [3]. In the current work, a simplification of the classification proposed by these authors for the medial meniscus insertion was used. The four groups of anterior horn insertions of the medial meniscus were simplified to only two in MRI sagittal images. There are two reasons for the simplification. On one hand, it was difficult for the authors to identify the four groups in MRI images previously founded in anatomical dissections. Furthermore, both of the anterior variants probably conditioned similar biomechanical behavior of the meniscus under physiological load as suggested by Berlet and Fowler [3]. According to the results obtained from the present series, their hypothesis seems to be confirmed.
One of the limitations of the present study is that both the MRIs and the arthroscopic surgery were done on symptomatic knees. Although we looked upon the MRIs of those patients without meniscal pathology as normal controls, one can consider those knees as having some degree of abnormality. However, the possible influence of these abnormalities on the final results were considered to be insignificant as they were not taken into account as a cause of extrusion, as far as we know.
A second limitation is that the MRI used to evaluate the degree of meniscal extrusion is a static image with the patient supine. During the movements of flexion and extension of the knee, the menisci are moved about an anterior–posterior axis. Therefore, the image of the meniscus in knee extension is only one of the possible locations of the meniscus. In a recent work, Boxheimer et al. [5] carried out MRI studies on 22 asymptomatic patients in various positions, including the weightbearing position. They demonstrated that extrusion of the medial meniscus depends on knee position, rotation, and load. In the supine position, extruded medial meniscus appeared in nine out of the 22 cases. The number of cases increased to 50% upon realizing the measurement in the loaded weightbearing position.
There are doubts as to whether MRI images of this partially luxated meniscus are a physiological fact. There are also doubts as to whether there are some predisposing anatomical morphologies associated with extrusion. There is a further doubt as to whether there is a true pathological condition that can affect the behavior of the knee joint surfaces. The results of the present work suggest meniscal extrusion to be much more common in normal knees than previously estimated. Extrusion might have been even more frequent if the study had been carried out under load conditions. The results also suggest that when the anterior horn of the medial meniscus inserts anteriorly in the tibial plateau, the meniscus tend to be extruded. However, it cannot be stated that this extrusion is or is not deleterious to the articular surfaces. Further studies are needed in order to answer this question.
References
Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S (1999) Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 54:502–506
Bennett LD, Buckland-Wright JC (2002) Meniscal and articular cartilage changes in knee osteoarthritis: a cross-sectional double-contrast macroradiographic study. Rheumatology 41:917–923
Berlet GC, Fowler PJ (1998) The anterior horn of the medial meniscus. An anatomic study of its insertion. Am J Sports Med 26:540–543
Breitenseher MJ, Trattnig S, Dobrocky I, Kukla C, Nehrer S, Steiner E, Imhof H (1997) MR imaging of meniscal subluxation in the knee. Acta Radiol 38(5):876–879
Boxheimer L, Lutz AM, Treiber K, Goepfert K, Crook DW, Marincek B, Weishaupt D (2004) MR Imaging of the knee: position related changes of the menisci in asymptomatic volunteers. Invest Radiol 39:254–263
Fukubayashi T, Kurosawa H (1980) The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthritic knee joints. Acta Orhop Scand 51:871–879
Gale DR, Chaisson CE, Totterman SMS, Schwartz RK, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage 7:526–532
Kurosawa H, Fukubayashi T, Nakajima H (1980) Load bearing mode of the knee joint: physical behaviour of the knee joint with and without menisci. Clin Orthop 149:383–390
Potter HG, Rodeo SA, Wickiewicz TL, Warren RF (1996) MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology 198:509–514
Verdonk P, Depaepe Y, Desmyter S, De Muynck M, Almqvist KF, Verstraete K, Verdonk R (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12(5):411–419
Yang A, Yang SS, Greif WL, Janick PA, Michael R (1993) Role of meniscal subluxation in degenerative arthritis of the knee. Demonstration with coronal MR imaging and the oreo cookie model. Radiol Suppl 189:380
Acknowledgements
We wish to thank Mr. Joan Vila, statistician at the Institut Municipal d’Investigació Mèdica (IMIM), for his help in the management of the data. The authors have not received anything of value from a commercial or other party related directly or indirectly to the subject of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puig, L., Monllau, J.C., Corrales, M. et al. Factors affecting meniscal extrusion: correlation with MRI, clinical, and arthroscopic findings. Knee Surg Sports Traumatol Arthrosc 14, 394–398 (2006). https://doi.org/10.1007/s00167-005-0688-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-005-0688-8