Abstract
Several studies have been published on disc degeneration among young athletes in sports with great demands on the back, but few on competitive divers; however, there are no long-term follow-up studies. Twenty elite divers between 10 and 21 years of age, with the highest possible national ranking, were selected at random without knowledge of previous or present back injuries or symptoms for an MRI study of the thoraco-lumbar spine in a 5-year longitudinal study. The occurrence of MRI abnormalities and their correlation with back pain were evaluated. Eighty-nine percent of the divers had a history of back pain and the median age at the first episode of back pain was 15 years. Sixty-five percent of the divers had MRI abnormalities in the thoraco-lumbar spine already at baseline. Only one diver without abnormalities at baseline had developed abnormalities at follow-up. Deterioration of any type of abnormality was found in 9 of 17 (53%) divers. Including all disc levels in all divers, the total number of abnormalities increased by 29% at follow-up, as compared to baseline. The most common abnormalities were reduced disc signal, Schmorl’s nodes, and disc height reduction. Since almost all divers had previous or present back pain, a differentiated analysis of the relationship between pain and MRI findings was not possible. However, the high frequency of both back pain and MRI changes suggests a causal relationship. In conclusion, elite divers had high frequency of back pain at young ages and they run a high risk of developing degenerative abnormalities of the thoraco-lumbar spine, probably due to injuries to the spine during the growth spurt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In order to reach elite level, many sports require training with high intensity and with high load from an early age. Regular training of pre-adolescents is therefore common [1, 21, 25]. Caine et al. [7] raised a warning flag for the early selection of one sport and the early start of rational training. Training with the aim of perfection often requires monotonous and repetitive strenuous physical exercises, with an increased risk of musculoskeletal morbidity and/or disturbed growth [1, 19]. The growing spine has been found to be highly vulnerable to trauma, especially during the adolescent growth spurt [2, 3, 5, 9].
Several studies have shown higher frequencies of intervertebral disc degeneration and abnormalities affecting the vertebral endplates and the vertebral ring apophyses among young athletes in sports with great demands on the back when compared to other athletes and non-athletes [3, 14, 17, 20, 26, 28, 38]. Injury rather than duration of athletic loading seems important in the aetiology of an early degenerative process in the thoraco-lumbar spine among athletes [20, 26, 28, 38]. There is, however, incomplete knowledge regarding the effects of intensive physical loading on the spine, at which ages abnormalities occur, and if they are due to injuries or overuse in adolescence.
It has also been reported that athletes with abnormalities of the vertebrae and disc degenerations have more back pain than other athletes and non-athletes [11, 16, 18, 23, 24, 26, 28, 39, 40, 43–45]. Lower back pain (LBP) among athletes may result from acute macrotrauma, repetitive microtrauma (stress), or from a combination of these two mechanisms [18, 22, 24, 35, 38]. There is limited knowledge of the effects of intensive physical loading and development of injuries in the spine during growth, and whether these injuries contribute to LBP and disc degeneration in adulthood.
Only few studies have reported the risk for injuries affecting the thoracic and lumbar spine and back pain of competitive divers. The prevalence of lumbar back injuries in competitive divers has been found to be up to 49%, based on collective data from two limited surveys conducted in 1980 and 1991 [4, 33]. However, there are no long-term follow-up studies on elite divers. Competitive diving puts high demands on the spinal column [13, 32]. The exposure of axial load on the spine of competitive divers is well described [4, 13, 32]. Flexion and extension bending occur in most diving manoeuvres and axial loading, shearing and torsional stresses act through multiple spinal segments, creating the potential for injuries [6]. The injury mechanism is related to the takeoff, flight, and the entry phases, and each phase can cause different spine injuries [6]. The average entry speed into the water is between 8.4 (1 m springboard) and 14.0 m/s (10 m platform). At impact, a speed reduction of more than 50% within a fraction of a second has been demonstrated, resulting in tremendous axial load on the spine creating significant potential for injuries [4, 13, 32]. Badman and Rechtine [6] suggest that young divers are at risk for disk degeneration at an earlier age than the general population due to annulus tears from torsional shear forces and repetitive axial compressive loads, promoting initiation of degeneration [6].
The aim of the present 5-year longitudinal MRI follow-up study is to examine the frequency and development of abnormalities in the thoraco-lumbar spine of elite divers and the correlation to back pain. The hypothesis of the study is that high loads on the spine of divers during the growth spurt are correlated to an increase of abnormalities and to back pain.
Materials and methods
Individuals
Twenty Swedish elite divers (1–3 m springboard and/or 5–10 m platform) aged ≥10 years with the highest possible ranking were selected without knowledge of previous or present back injuries or symptoms. All divers (14 girls and 6 boys) between 10 and 21 years of age accepted to participate in an MRI study of the thoraco-lumbar spine in 1992. In 1997, all the participants in the first examination were invited to take part in a clinical and MRI follow-up study. One diver had died in 1994 and two others did not want to be re-examined with MRI; these two were therefore excluded from the MRI evaluation. One of these individuals did not take part in the questionnaire evaluation and clinical examination. The results in the follow-up study are based on 18 divers regarding the back pain questionnaire and clinical examination, and 17 in the MRI evaluations.
The study was approved by the Ethics Committee at the Sahlgrenska Academy at Göteborg University, Göteborg, Sweden.
MRI examination
The MRI examinations at baseline were performed on a superconductive equipment (Siemens Magnetom) operating at a field strength of 0.5 T. Double-echo, multislice, spin-echo techniques were used with a repetition time (TR) of 1,500 ms and echo times (TE) of 30 and 90 ms. The number of acquisitions (Ac) was two for all sequences and the acquisition matrix was 256×256. Sagittal slices with a thickness of 5 mm and an interslice gap of 2.5 mm were recorded.
The MRI examinations at follow-up were performed on a 1.0 T Signa Advantage system (GE Medical System, Milwaukee, WI, USA). Sagittal T1 images (spin echo: TR, 460 ms; TE, 10 ms) and T2 images (fast spin echo: TR 3,220 ms; TE 115 ms) with a field of view of 24×12 cm as well as axial T1 (spin echo: TR, 440 ms; TE, 30 ms) and T2 images (fast spin echo: TR, 3,000 ms; TE, 104.1 ms) with a field of view of 16×8 cm were obtained. A matrix of 512×384 and a slice thickness of 3 mm with a 0.5 mm gap were used in all sequences.
On both occasions a spine coil was used in all examinations. The patients were placed in a supine position with T9 at the centre of the coil at the first sequence and L3 at the centre of the surface coil for the second sequence. The T2-weighted images were the most sensitive to changes in the disc signal intensities, while morphology was usually best evaluated on the T1-weighted images. In all athletes we were able to evaluate the discs T6–7 through L5–S1.
The images from the first examination and the second examination were evaluated together, side by side, for comparison by two experienced radiologists. The films were evaluated according to a standardised protocol, including an assessment of interval changes in MRI findings between the baseline and the follow-up examinations. All abnormalities were graded from 0 to 3.
MRI: diagnostic criteria and definitions
Disc signal reduction or degeneration was evaluated on T2-weighted images. Disc signal was graded as follows: 0=normal, 1=slight reduction as compared to normal appearing adjacent discs, 2=moderate reduction, or 3=severe reduction (complete or near complete lack of signal) [31, 38].
Disc height reduction was defined as reduction of an intervertebral disc height as compared with normal appearing discs above and below. Disc height was graded as follows: 0=normal, 1=slight, height reduction less than 50%, 2=moderate, height reduction 50–90%, and 3=severe, height reduction more than 90% [20]. At follow-up, any change in disc height reduction was considered when comparing with the initial examinations [31, 38].
Disc bulging was defined as a convex extension of the disc beyond the cortex of the vertebrae, and was graded as: 0=normal, 1=slight, 2=moderate, or 3=severe [38].
Apophyseal abnormalities: These abnormalities were considered as Schmorl’s nodes or sequels from such nodes and were defined as separation of an apophyseal bony fragment from the vertebral body or deformation of the apophyseal region. These abnormalities were recorded separately, graded as: 0=normal, 1=slight, 2=moderate, or 3=severe [38].
Schmorl’s node (intraspongious disc herniation): a clearly defined non-marginal defect in the vertebral endplate, with similar signal intensity as the rest of the disc. Abnormalities affecting the region of the ring apophysis, such as separation of an apophyseal bony fragment from the vertebral body or deformation of the apophyseal region, were considered as Schmorl’s nodes or sequels of such nodes [34]. When nuclear material herniates anteriorly, posteriorly, or laterally, it can undermine the ring apophysis, separate it from the body of the vertebra, and lead to the so-called limbus vertebra [36]. Smooth, shallow bulges in the endplate or minimal endplate irregularities were excluded. Schmorl’s nodes were graded as: 0=normal, 1=slight, 2=moderate, or 3=severe.
Abnormal configurations of the vertebral bodies: flattening of the vertebral body, anterior wedging greater than 5°, or increased antero-posterior diameter of the vertebral bodies. It was graded as: 0=normal, 1=wedging, 2=flattening, and 3=increased AP diameter [38].
Back pain: questionnaire
At follow-up, 18 divers answered a self-assessed two part questionnaire concerning back pain according to Swärd et al. [37, 38] and the Oswestry Disability Questionnaire [12], respectively. The questionnaires were sent home to the divers with instructions.
In the first part of the questionnaire, back pain was defined as previous or present pain located in the thoraco-lumbar spine. The divers were asked if they had any radiating pain, if the pain was influenced by training or competition, and if any movements aggravated the pain. They were also asked at what age it appeared. Back pain was self-assessed by the divers and was graded moderate or severe. It was graded as moderate if it did not affect daily living, work, or training and competition, and severe if it did affect daily living, work, or training and competition at any time. The athletes were asked if they still were active in their sport, how many hours per day and week they exercised, and if they still took part in competitions. If they were not active, they were asked at what age they finished their active career and if this was due to back pain. They were asked to draw a schematic figure of the location and type of their back pain [29, 30].
The second part, the Oswestry questionnaire, served to provide a subjective rating of performance of daily activities. It consists of ten questions. The question concerning sex life was excluded. Each question was scored on a 0–5 scale, where 5 represented the greatest disability. The score for all questions was added giving a maximal score of 45. The Oswestry Disability Index was expressed in percent by dividing the patient’s score with the maximal score 45. Minimal disability: 0–19%, moderate 20–39%, severe 40–59%, crippled 60–79%, and patients either bed-bound or exaggerating their symptoms 80–100%.
Clinical examination
The neurological examinations of the lower extremities and the spine of all divers were performed at the time of the MRI examination.
Statistical methods
The estimation of the probability of having at least one episode of back pain was estimated by the use of Kaplan–Meier’s method. Fisher’s permutation test [15] was applied to compare men and women and to compare divers who stopped vs those who continued diving in competition or practice with respect to MR findings and with respect to change of MR findings between baseline and follow-up. Fisher’s permutation test is a non-parametric test, which includes test for trend in contingency table as a special case when one of the dimensions of the table is 2.
Results
The median age at baseline was 17 years (range 10–21 years, mean 16.4±3.1 years) and it was 21 years (range 16–26 years, mean 21.2±3.0 years) at follow-up. At follow-up, nine of 18 divers were active in competitive diving and the others were still training diving. The median age for the nine divers who stopped competitive diving was 19.8 years (range 15–25). Three of them stated that they stopped competitive diving due to back pain. The median training days/week at follow-up was 3.5 (range 1–7, mean 4.0±1.6 h) and median training hours/week was 5 (range 2–11, mean 6.5±2.9 h). The divers who still were active in competitions, all of whom had frequent training (n=9), had a mean training duration of 8.8 h/week. Four of the divers trained >11 h/week. MRI abnormalities were found already at baseline in three and at follow-up in four of the seven divers, who were training more than 8 h/week at follow-up. In divers training less than 8 h/week, MRI abnormalities could be found in 8 of 11 divers.
Back pain
Sixteen of 18 divers (89%) had a previous or present history of back pain; therefore, no statistical calculations and correlation with MRI findings were made. The probability that back pain would appear within 1 year (if there was no back pain history earlier) was calculated (by use of the general relationship between hazard and survival function) and was about 45%, i.e. almost every other diver who had not had any back pain history would suffer from back pain within 1 year, assuming that one had reached 13 years of age.
The median age at the first episode of back pain was 15 years (range 10–17 years, mean 15±1.6 years) and 15 of the 16 individuals with a history of back pain had their first back pain episode at age 14–17 years. Eight of the subjects reported that diving was the cause of their back pain, two reported other trauma, four did not know, and two did not answer the question regarding the cause of their back pain. Ten of the 16 divers stated that their back pain did deteriorate with training and two stated an improvement with training.
When grading their back pain, seven divers reported moderate and seven reported severe back pain, while two did not answer this question. Of those with severe pain, two divers had discontinued training once, five divers two to ten times and two divers more than ten times due to back pain at any time up to the follow-up study. One diver had discontinued competition once and three divers two to ten times because of back pain. Using a schematic drawing of the body, one diver located the pain in the thoracic spine, four in the thoraco-lumbar spine, seven in the lumbar spine and four in the lumbo-sacral spine regions. None of the divers reported radiating back pain.
Oswestry Disability Questionnaire
Two of the 18 divers did not fill in the Oswestry questionnaire. Thirteen of 16 divers had minimal (0–19%) and one diver had moderate (20–39%) grade of disability. Seven divers stated difficulties with lifting heavy weights and eight stated difficulties with standing more than 1 h because of increased back pain.
Clinical examination
At physical examination, all divers had normal neurological findings in the lower extremities, including negative Lasègues’ test. One of the divers had a mild structural scoliosis in the thoracic spine. At palpation, eight divers had tenderness in the thoracic and five other divers in the lumbar spine. Five of the divers had both MRI abnormalities and tenderness in the thoracic/lumbar spine at palpation. Five divers had MRI abnormalities but no tenderness at palpation and five had tenderness but no MRI abnormalities. Three divers had neither MRI abnormalities nor tenderness. There was no statistical correlation between MRI abnormalities and tenderness at palpation (P>0.30).
MRI abnormalities
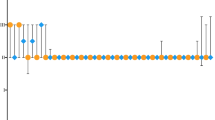
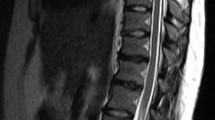
At baseline MRI examination, 12 of 18 (67%) divers and at follow-up 12 of 17 (71%) divers (Table 1) had abnormalities in the thoraco-lumbar spine (Fig. 1). One of the patients with MRI abnormalities at baseline was not re-examined at follow-up, and one patient without MRI abnormalities at baseline had developed MRI abnormalities at follow-up. The youngest individuals with MRI changes were 12 years old.
At baseline, a total of 69 MRI abnormalities were found in the examined levels T6–7 to L5–S1 in 12 of 18 divers. At follow-up, 89 abnormalities were found in 12 of 17 divers. Thus, 20 new abnormalities (29% increase) had occurred at follow-up, including all types of abnormalities (reduced disc signal, disc height reduction, disc bulging, injury to the ring apophyses, Schmorl’s nodes, and abnormal configuration of the vertebral body) including all anatomical levels and all individuals (Table 1 and Fig. 2). Deterioration (new abnormalities or increase of an abnormality score at a previously affected disc level) of any type of abnormality found at baseline was seen in nine (53%) of 17 divers at follow-up. One diver who did not have any abnormality at baseline had developed disc signal reduction at follow-up. Disc signal reduction was found at all anatomical levels of the thoraco-lumbar spine, while disc height reduction was predominantly seen at the lower thoracic and upper lumbar level. Schmorl’s nodes had a similar distribution, while the other abnormalities were too few to show any clear distribution pattern. None of the abnormalities seen at baseline had disappeared at follow-up.
Worst disc level at baseline vs follow-up
The abnormalities with the highest score (0–3, the worst disc level taken over all levels) at follow-up were reduced disc signal (12 of 17 cases), Schmorl’s nodes (7 of 17 cases), and disc height reduction (6 of 17 cases). The total number of abnormalities with a score similar to that of the worst abnormality score (including all individuals) was 26 at baseline and 31 at follow-up (Table 2).
MRI changes from baseline to follow-up
Only data from divers investigated on both occasions were used in this analysis (N=17). Fourteen divers had the same highest score of disc signal reduction on both occasions while three divers had deteriorated disc signal (the highest score increased from 0 to 2 in one diver and from 1 to 2 in two divers). Deterioration (reduced signal in a previously normal disc or increase of disc signal score in a previously affected disc, or increase of score at a new anatomical level) was found in nine (53%) divers and in 14 of 204 discs (Fig. 2). The hypothetical probability of achieving disc signal reduction was calculated under the assumption that disc signal was unaffected before the age of 12 years. At the age of 18 years, half of the population could be expected to have a reduced disc signal.
Fifteen divers had the same highest score of disc height reduction on both occasions. Eleven divers did not have disc height reduction at follow-up. Disc height reduction had progressed in two divers and three discs at follow-up (from grade 0 to 1).
Fifteen divers had the same highest score of disc bulging at both examinations. New disc bulging occurred in two individuals at follow-up: from grade 0 to 1 in one diver and from 0 to 2 in another diver.
One injury affecting the ring apophyses was identified at baseline and no new apophyseal injury was found at follow up.
There were six divers (35%) with Schmorl’s nodes at baseline. At follow-up there was one new case.
Abnormal configuration of the vertebral body was found in one diver at baseline and in two additional divers at follow-up.
Three of seven divers younger than 16 years at baseline had abnormalities. During the 5-year follow-up, there was a deterioration of the abnormalities in one of them. Eight of the ten divers that were ≥16 years had abnormalities at baseline and there was a deterioration of the abnormalities in eight of them at follow-up.
There were no significant differences regarding the frequency of MRI abnormalities between boys and girls, or between those who had discontinued and those who had continued competitive diving at follow-up.
Modic changes
At follow-up, a localised high-intensity area was noted in the posterior lower part of the L3 vertebral body, adjacent to the degenerated L3–L4 disc at T1-weighted MRI, in a 23 year old male diver. It was slightly hyperintense at T2-weighted images. At baseline MRI, it was not identifiable at T1, but faintly visible at T2-weighted images. The finding at follow-up was suggestive of a localised Modic type 2 change. No other divers had evidence of Modic-type abnormalities.
Discussion
The current study showed that 16 of the 18 divers (89%) had a history of back pain at the time of follow-up (median age 21 years, range 16–25 years). MRI abnormalities in the thoraco-lumbar spine were found in two out of three divers at baseline, and a similar frequency was noted 5 years later. New abnormalities or deterioration of an abnormality at a previously affected disc level was found in 53% of the divers, and the total number of abnormalities, including all disc levels in all divers, increased by 29% at follow-up.
The lifetime prevalence of back pain in the present study was 89%, which is significantly higher than in previous reports (up to 49%) regarding competitive divers [4, 33]. After reaching 13 years of age, the calculated probability of back pain occurring within 1 year was 45%. Nearly all divers (16 of 18) had back pain, which is remarkable for such a young population. In the self-assessed questionnaire, 8 of 14 responders attributed their back pain to diving, while four were uncertain, and two referred to other trauma. The results suggest a strong relationship between diving and back pain. The time of the first back pain episode coincided with the growth spurt period (14–17 years of age), supporting the notion that this is a very vulnerable period.
The high frequency of back pain in the current study is in line with results of studies on young athletes in other sports with high demands on the spine [10, 22, 27, 39]. Goldstein et al. [14] reported a strong correlation between the development of degenerative changes and back pain in gymnasts, and the frequency of back pain was suggested to correlate to the level of activity. In contradiction to these findings, Lundin et al. [28] found in a study of elite athletes representing wrestling, gymnastics, soccer, and tennis that the athletes did not report more back pain than non-athletes (all athletes 60%, non-athletes 61%, female gymnasts 67%), despite significantly more radiological changes. The difference between these two studies may be due to the fact that in the study by Goldstein et al. [14], the athletes were younger (mean age in female gymnasts 16.6 years) and still active in their sport, while in the study by Lundin et al. [28] the individuals were older (mean age in female gymnasts 30.6 years, all athletes 33.1 years) and they were mostly former, rather than active, elite athletes.
We found that 67% of the divers had MRI abnormalities in the thoraco-lumbar spine already at baseline. Only one patient without abnormalities at baseline had developed abnormalities at follow-up, although deterioration of existing abnormalities was noted in half of the population. At follow-up, there were no improvements of the abnormalities found at baseline. Disc signal reduction was found in all disc levels, whereas disc height reduction was found almost exclusively in the lower thoracic and in the upper lumbar segments. Disc signal reduction is probably preceding disc height reduction and is a notice for the future. Our MRI findings are in accordance with a 3-year longitudinal study by Kujala et al. [26] on young female athletes representing gymnastics and figure skating, in comparison to matched controls. Similar findings are reported in several studies in different groups of young athletes, mostly gymnasts [14, 26, 42]. In contrast to these findings, Tertti et al. [41] found that only 3 of 35 female gymnasts had MRI evidence of degenerated discs, possibly due to lower age of the athletes (mean 12±2.6 years, range 8–19 years), different MRI equipment (0.02 T), and differences in definitions of disc degeneration.
The degenerative changes found in adolescence in this study may be related to acute spine injuries occurring during the pubertal growth spurt early in the athletic career. In the current study, the abnormalities were found from the age of 12 years, and deterioration was found in only one of the divers under 16 years, but in 73% of those over 16 years. The results from the present and previous studies suggest that degenerative changes are common among young elite athletes and that trauma to the thoraco-lumbar spine during the growth spurt is harmful [2, 5, 14, 26]. Repeated acute injuries has been reported to be of aetiological importance for the early degenerative process in the lumbar spine of athletes rather than long-term heavy loading on the spine [10, 14, 17, 20, 26, 28, 38]. However, it is a clinical impression that deterioration of spinal injuries occurs also without significant new trauma, suggesting that continued heavy loading is of importance.
Goldstein et al. [14] found that 57% of the gymnasts who trained 15 h or more per week had degenerative changes on MRI, as compared to 13% in those who trained less, and they concluded that the amount of training is of importance for the development of spinal injuries. In the present study, we could not find any correlation between the level of activity and MRI abnormalities. Although the reports are on different sports, they have several biomechanical similarities. The lack of relationship between amounts of training and MRI changes in our study may be explained by the lack of data on training activity during the peak competitive period since we collected data only at follow-up, when less than half of the divers were in competitive training.
Limitations of the present study include the relatively small size of the study group and the relatively wide age range of divers, as well as the lack of an age and sex matched control group. Competitive diving is a small sport with a limited number of participants at elite level in our country. We managed to recruit all of the nationally top ranked divers for the baseline MRI study, and compliance at follow-up was complete except for one interval death, one individual who declined MRI and questionnaire, and one who declined only MRI. The age range at inclusion (10–21 years) prevented a comprehensive stratified analysis of the influence of age on the development of spinal injuries among the divers. Another limitation of our study was the retrospective analysis of first episode of back pain, leaving room for recall bias. However, the consistent reporting from the participants of first episode of back pain at 14–17 years of age suggests a relationship with the vulnerable growth spurt. An additional limitation of this study was that almost all divers (89%) had previous or present back pain, regardless of MRI findings, limiting a differentiated analysis of the relationship between pain and MRI findings. However, the high frequency of both back pain and MRI changes suggests a causal relationship.
Although our study clearly indicates that spinal injuries and back pain are common in young divers and that these injuries appear to occur at an early age, larger studies are needed to confirm our findings and to further analyse the influence of age, gender, training intensity, and diving technique on the development of back pain and spinal injuries.
From a clinical standpoint, increased awareness of these factors among coaches and health professionals seems warranted in order to find means of reducing the risks of spine injury and back pain in young divers [6, 8].
In conclusion, elite divers have a high frequency of back pain at young ages and they run a high risk of developing degenerative abnormalities of the thoraco-lumbar spine, probably due to injuries to the spine during the growth spurt.
References
Adirim TA, Cheng TL (2003) Overview of injuries in the young athlete. Sports Med 33:75–81
Alexander J (1976) Effect of growth rate on the strength of the growth plate-shaft function. Skeletal Radiol 1:67–76
Alexander J (1977) Scheuermann’s disease. A traumatic spondylodystrophy? Skeletal Radiol 1:209–221
Andersson SJ, Rubin BD (1994) Evaluation and treatment of injuries in competitive divers. In: Buschbacher B, Braddom RL (eds) Sports medicine and rehabilitation: a sport specific approach. Hanley and Belfus, Philadelphia, PA, pp 111–122
Arkin A, Katz J (1956) The effects of pressure on epifpyseal growth. J Bone Joint Surg Am 38:1056–1076
Badman BL, Rechtine GR (2004) Spinal injury considerations in the competitive diver: a case report and review of the literature. Spine J 4:584–590
Caine D, Lindner K (1985) Overuse injuries of growing bones: the young female gymnast at risk? Physician Sports Med 13:51–64
Dalton SE (1992) Overuse injuries in adolescent athletes. Sports Med 13:58–70
Ehrenhaft J (1943) Development of the vertebral column as related to certain congenital and pathological changes. Surg Gynecol Obstet 76:282–292
Epstein N, Epstein J (1991) Limbus lumbar vertebral fractures in 27 adolescents and adults. Spine 16:962–966
Eriksson K, Nemeth G, Eriksson E (1996) Low back pain in elite cross-country skiers. A retrospective epidemiological study. Scand J Med Sci Sports 6:31–35
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Gabriel JL (1990) US diving safety manual. US Diving Publications, Indianapolis
Goldstein JD, Berger PE, Windler GE, Jackson DW (1991) Spine injuries in gymnasts and swimmers. An epidemiologic investigation. Am J Sports Med 19:463–468
Good P (2000) Permutation tests. Springer, Berlin Heidelberg New York
Granhed H, Morelli B (1988) Low back pain among retired wrestlers and heavyweight lifters. Am J Sports Med 16:530–533
Halvorsen TM, Nilsson S, Nakstad PH (1996) Stress fractures. Spondylolysis and spondylolisthesis of the lumbar vertebrae among young athletes with back pain. Tidsskr Nor Laegeforen 116:1999–2001
Harvey J, Tanner S (1991) Low back pain in young athletes. A practical approach. Sports Med 12:394–406
Hawkins D, Metheny J (2001) Overuse injuries in youth sports: biomechanical considerations. Med Sci Sports Exerc 33:1701–1707
Hellström M, Jacobsson B, Swärd L, Peterson L (1990) Radiologic abnormalities of the thoraco-lumbar spine in athletes. Acta Radiol 31:127–132
Hogan KA, Gross RH (2003) Overuse injuries in pediatric athletes. Orthop Clin North Am 34:405–415
Jackson DW (1979) Low back pain in young athletes: evaluation of stress reaction and discogenic problems. Am J Sports Med 7:364–366
Jackson DW, Wiltse LL, Cirincoine RJ (1976) Spondylolysis in the female gymnast. Clin Orthop 117:68–73
Keene JS, Drummond DS (1985) Mechanical back pain in the athlete. Compr Ther 11:7–14
Kozar B, Lord R (1983) Overuse injury in the young athlete: reasons for concern. Physician Sports Med 11:116–122
Kujala UM, Taimela S, Erkintalo M, Salminen JJ, Kaprio J (1996) Low-back pain in adolescent athletes. Med Sci Sports Exerc 28:165–170
Kujala UM, Taimela S, Viljanen T (1999) Leisure physical activity and various pain symptoms among adolescents. Br J Sports Med 33:325–328
Lundin O, Hellström M, Nilsson I, Swärd L (2001) Back pain and radiological changes in the thoraco-lumbar spine of athletes. A long-term follow-up. Scand J Med Sci Sports 11:103–109
Mooney V, Cairns D, Robertson J (1976) A system for evaluating and treating chronic back disability. West J Med 124:370–376
Palmer H (1949) A description of a technique whereby functional pain may be diagnosed from organic pain. N Z Med J 48:187–213
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Rubin BD (1999) Aquatic sports injuries and rehabilitation; the basics of competitive diving and its injuries. Clin Sports Med 18:293–303
Rubin BD (1983) Orthopedic aspects of competitive diving injuries. US Diving, Indianapolis
Schmorl G, Junghanns H (1971) The human spine in health and disease, 2nd edn. Grune & Stratton, New York
Semon RL, Spengler D (1981) Significance of lumbar spondylolysis in college football players. Spine 6:172–174
Swischuk LE, John SD, Allbery S (1998) Disk degenerative disease in childhood: Scheuermann’s disease, Schmorl’s nodes, and the limbus vertebra: MRI findings in 12 patients. Pediatr Radiol 28:334–338
Swärd L, Hellström M, Jacobsson B, Nyman R, Peterson L (1990) Acute injury of the vertebral ring apophysis and intervertebral disc in adolescent gymnasts. Spine 15:144–148
Swärd L, Hellström M, Jacobsson B, Nyman R, Peterson L (1991) Disc degeneration and associated abnormalities of the spine in elite gymnasts. A magnetic resonance imaging study. Spine 16:437–443
Swärd L, Hellström M, Jacobsson B, Peterson L (1990) Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine 15:124–129
Szot Z, Boron Z, Galaj Z (1985) Overloading changes in the motor system occurring in elite gymnasts. Int J Sports Med 6:36–40
Tertti M, Paajanen H, Kujala UM, Alanen A, Salmi TT, Kormano M (1990) Disc degeneration in young gymnasts. A magnetic resonance imaging study. Am J Sports Med 18:206–208
Tertti MO, Salminen JJ, Paajanen HE, Terho PH, Kormano MJ (1991) Low-back pain and disk degeneration in children: a case–control MR imaging study. Radiology 180:503–507
Tsai L, Wredmark T (1993) Spinal posture, sagittal mobility, and subjective rating of back problems in former female elite gymnasts. Spine 18:872–875
Verni E, Prosperi L, Lucaccini C, Fedele L, Beluzzi R, Lubich T (1999) Lumbar pain and fin swimming. J Sports Med Phys Fitness 39:61–65
Videman T, Sarna S, Battie MC, Koskinen S, Gill K, Paananen H, Gibbons L (1995) The long-term effects of physical loading and exercise lifestyles on back-related symptoms, disability, and spinal pathology among men. Spine 20:699–709
Acknowledgements
The authors acknowledge the financial support of The Medical Society of Göteborg, Sweden, Trygg-Hansa Insurance Company, The Research Council of the Swedish Sports Confederation and Government grants under the LUA agreement. The authors acknowledge the support of Prof. Jon Karlsson, Sahlgrenska Academy at Göteborg University and the assistance of the statistical advisor Professor Anders Odén, PhD, Romelanda, Sweden. The authors thank radiology technician P-A Svensson, Department of Radiology at Queen Silvia’s Children’s Hospital, Sahlgrenska University Hospital, Göteborg. The study was approved by the Ethics Committee at the Sahlgrenska Academy at Göteborg University, Göteborg, Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baranto, A., Hellström, M., Nyman, R. et al. Back pain and degenerative abnormalities in the spine of young elite divers. Knee Surg Sports Traumatol Arthr 14, 907–914 (2006). https://doi.org/10.1007/s00167-005-0032-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-005-0032-3