Abstract
Open kinetic chain (OKC) knee extensor resistance training has lost favour in ACLR rehabilitation due to concerns that this exercise is harmful to the graft and will be less effective in improving function. In this randomized, single-blind clinical trial OKC and closed kinetic chain (CKC) knee extensor training were compared for their effects on knee laxity and function in the middle period of ACLR rehabilitation. The study subjects were 49 patients recovering from ACLR surgery (37 M, 12 F; mean age=33 years). Tests were carried out at 8 and 14 weeks after ACLR with knee laxity measured using a ligament arthrometer and function with the Hughston Clinic knee self-assessment questionnaire and single leg, maximal effort jump testing (post-test only). Between tests, subjects trained using either OKC or CKC resistance of their knee and hip extensors as part of formal physical therapy sessions three times per week. No statistically significant (one-way ANOVA, p>0.05) differences were found between the treatment groups in knee laxity or leg function. OKC and CKC knee extensor training in the middle period of rehabilitation after ACLR surgery do not differ in their effects on knee laxity or leg function. Exercise dosages are described in this study and further research is required to assess whether the findings in this study are dosage specific.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1993, Yack et al. [33] drew the attention of orthopaedic surgeons and physical therapists to the fact that greater anterior tibial displacement (ATD) occurs during open than during closed kinetic chain resistance exercise of the knee extensors. Along with other work [2, 13], this study resulted in an increased research effort to compare these two forms of exercise. More importantly, the Yack et al. study [33] and related work led to a shift in clinical practice away from the use of knee extensor open kinetic chain (OKC) training towards closed kinetic chain (CKC) training in patients with injury or surgery of the anterior cruciate ligament (ACL).
This shift to CKC exercise was partly based on the assumption that the greater ATD believed to occur during OKC exercise might lead to more pronounced permanent increases in knee laxity after a course of OKC training. This assumption can only be tested in clinical trials comparing the two regimens, which had not been done at the time. To further weaken the case for this assumption, Beynnon and Fleming [4] have since shed doubt on whether the exercises actually differ in their strain on the ACL.
There were two other reasons for the changing bias towards CKC training. Firstly, because CKC exercises appear to better replicate functional tasks, they were thought to enhance functional performance to a greater extent than OKC exercises [24, 25, 28, 29, 31]. Secondly, it was believed that CKC exercise would be less harmful to the patellofemoral joint [31]. Again, however, these beliefs had not been tested in clinical trials.
In 1995, the first clinical trial comparing OKC and CKC exercise of the knee extensors in ACL-injured subjects was published [8]. Subjects in this study were recovering from ACL reconstruction surgery and the subjects in the OKC group began to receive dynamic OKC training of the knee extensors at 6 weeks after surgery, whilst those in the CKC group started CKC exercises immediately after surgery. ATD was measured 19 months after the onset of rehabilitation with the KT1000 ligament arthrometer. The groups had statistically significant differences in ATD in the maximum manual test, the OKC group having a side-to-side difference of 3.3 compared to 1.6 mm for the CKC group. At a lower KT1000 force of 20 lb the groups did not differ. However, it is difficult to conclude that the differences were due to training as no baseline knee laxity testing was performed. The study also compared the effects of OKC and CKC exercise on subjective function, as measured by patients’ responses on questionnaires. Members of the CKC group reported that they returned to work earlier and tended to report greater satisfaction with their surgical outcome. However, there was a lack of any objective data on functional improvement.
In a more recent study of ACL reconstruction rehabilitation, Mikkelsen et al. [20] compared ATD and time to return to sports between a CKC group and a combined OKC/CKC group. The CKC group underwent a 6-month CKC exercise regime commencing immediately after ACLR surgery, whilst the combined group underwent a 6-month CKC regime also commencing immediately after surgery, with the addition of an OKC regime 6 weeks later. The groups did not differ in terms of ATD changes from before surgery to 6 months after surgery. Although baseline ATD measurements were performed prior to reconstruction, no post-reconstruction measurements were taken before the onset of the exercise programme. Pre-reconstruction knee laxity may bear little relation to post-reconstruction laxity and is therefore an unsuitable baseline from which to judge the extent of any changes in graft laxity due to exercise after surgery. The combined group was found to return to pre-injury sports level significantly sooner, which possibly indicates the usefulness of including OKC training in ACLR rehabilitation. However, the greater training dosage in the combined training group may explain this result more than any fundamental difference between the two regimens.
Most recently, our research team compared the effects of OKC and CKC exercise programmes on laxity and function in ACLR patients after a 4-week training period commencing 2 weeks after surgery [14, 22]. No significant differences were found between the groups in terms of ATD increases or functional changes. This study included ATD measurements immediately before and after the 4-week training period and subjective (questionnaire) and objective (gait in walking and stair climbing) measures of function. In common with the studies by Bynum et al. [8] and Mikkelson et al. [20], this study lacked data on training dosage, making it difficult to draw useful conclusions about training effect.
In the ACLR knee, there are two post-operative periods when the graft is believed to be most susceptible to loosening and stretching. Firstly, the graft fixation site is weakest immediately after surgery [17, 18, 27]. Secondly, as the fixation site becomes stronger, the soft tissue component of the graft tissue becomes gradually weaker until it reaches its weakest point, which is believed to occur at approximately 12 weeks after surgery when strength recovery begins to occur [15, 27]. We have already found that the two regimes do not differ in their effects on laxity and function in the first period of graft vulnerability [14, 22]. However, no study has yet prospectively investigated the effects of these regimes on laxity and function during the second period of graft susceptibility. Hence, the purpose of this study was to compare the effects of the two regimens on knee laxity and function in the 8- to 14-week period after ACL reconstruction. The null hypotheses to be tested are that the groups will not differ in terms of injured knee laxity or self-assessed and objective knee function.
Methods
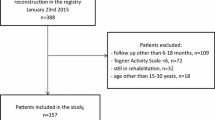
Subjects
Potential subjects were identified for this study from in-patients recovering from ACL reconstruction at 11 National Health Service and private hospitals in the London area. Subjects were deemed suitable for inclusion in the study if they had no prior history of pathology requiring medical attention in the contralateral lower extremity within the previous 6 months, they did not have a posterior cruciate ligament injury in the operated knee, they were aged 18–60 and their surgeon had given consent for them to be approached. Forty-nine patients successfully completed the study (i.e. attended the pre- and post-test).
Surgical procedures
Twelve orthopaedic surgeons participated in the study. Surgeon A performed ACL reconstruction using the technique described by Kennedy et al. [16]. This technique consists of combining the ligament augmentation device (3M, Minneapolis, MN, USA) with a small film of the patellar tendon to act as the graft. The tendon graft remains anchored at the tip of the tibial tuberosity. It is threaded through a tibial bone tunnel and then passed through the joint with an over-the-top technique and fixed with a lateral screw. Surgeons B, C and D performed arthroscopically assisted ACL reconstruction after harvesting a bone-patellar tendon-bone graft from the central third of the extensor mechanism via an anterior midline incision. The free graft is then inserted through tunnels in the tibia and femur with fixation using interference screws or staples. Surgeons E, F and G performed an open (non-arthroscopic) version of the above. Surgeons H, I, J, K and L performed arthroscopically assisted ACL reconstruction using a graft harvested from the semitendinosus and/or gracilis muscles. Surgeon B also used this technique for five of his patients.
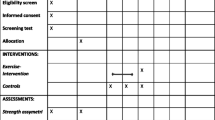
Testing
Within the first 8 weeks following surgery, subjects were approached and given a written and verbal explanation of the study and invited to volunteer for participation in the study. The target date for test initiation was 8 weeks after reconstruction surgery.
After reading and signing an informed consent form that had prior approval from the relevant local ethics committees, participants were asked to fill in a general questionnaire detailing their personal particulars, their injury and surgery dates, activity difficulties and present sporting activities. This was done with the assistance of the physical therapist examiner.
The Hughston Clinic questionnaire was used to evaluate the patient’s self-assessment of their knee condition [10]. This questionnaire consists of 28 questions in which the patient is asked to respond by marking 10-cm visual analogue scales (VAS). Where the horizontal line separating the two descriptors was bisected by the patient’s mark, the distance to the nearest 0.5 cm was measured from the left end of the scale. When values were between X.0 and X.5, values were always rounded up to X.5. Similarly, when values were between and X.5 and Y.0 (where Y=X+1) the values were also always rounded up. The rounding was done in this fashion to ensure consistency amongst examiners. For questions in which the subject responded by ticking the box for ‘not attempted because of my knee injury‘, a value of 10 was given. For questions in which the subject responded by ticking the box for ‘not attempted because of other reasons besides my knee injury’, the question was deleted from the analysis. The final score was calculated by aggregating the scores of the 28 questions and converting to a percentage of maximum possible score. A perfect knee would score 0% and the worst possible score was 100%.
Body height and weight were measured with the patient barefoot for both tests. Body height was measured first.
Limits of active knee motion were measured with the subject lying supine and using a manual goniometer as used in the clinic. The knee was actively flexed by the subject as far as the joint would allow or according to the patient’s tolerance of pain. The arms of the goniometer were aligned with the greater trochanter and lateral malleolus whilst the axis of the goniometer was placed over the knee joint line just below the lateral femoral epicondyle. The knee angle was then recorded. Active knee extension was measured in a supine position with a block placed under the subject’s heel to allow for hyperextension, or used to support the thigh if extension was limited. Goniometer alignment was the same as for the flexion test. Both knees were measured in this way and the uninjured knee was measured first. Active ROM testing was included as a baseline characteristic for comparing the control and intervention groups prior to intervention.
Knee circumference was also measured with the patient in the supine position. The subject’s heel was placed on a block in full passive extension to standardize the knee angle. For patients unable to achieve full passive extension, the knee angle was recorded and the post-test knee circumference repeated in the same position as in the pre-test. Measurements of knee girth were taken at the mid-point of the patella and the superior border of the patella using a cloth tape. Both knees were measured in this way with the uninjured knee measured first.
One of three physical therapists, at all times blinded to subject group assignment, performed knee laxity testing. One examiner (M.P.) tested 43 of the 49 subjects, another examiner (R.V.) tested five subjects and the third examiner (I.M.) tested one subject. The same examiner was used for pre- and post-testing of each patient in order to avoid error due to inter-observer variability. In reliability testing, we have found that our examiners’ least significant difference values in test–retests of ten uninjured subjects ranged from 3.8 to 4.8 mm, which compares favourably to published data [26].
Passive laxity of both knees was tested on the Knee Signature System (Orthopedic Systems, Inc., Union City, CA, USA). Arthrometric testing has been found to be valid relative to simultaneous radiography [30]. Prior to testing of each subject, the Knee Signature System (KSS) was calibrated using the ‘zero values function’. The patient, wearing shorts, was positioned sitting on the edge of the KSS seat. The uninjured knee was tested first. After application of the equipment to the leg using the manufacturer’s recommendations, testing was performed with the knee in approximately 25° of flexion (Lachman test) and neutral rotation. The knee flexion angle was determined with a standard goniometer and the tibial rotation by observation. With the knee in this position, ATD was tested using 178 N of force. Prior to each anterior displacement, a small posterior displacement force was applied to the shin to ensure that the shin was not already anteriorly displaced. Five test repetitions were performed on each leg. Each repetition was deemed successful if displacement was recorded at 178 N and the curve describing force–displacement passed through the origin of these axes.
Finally, each participant was given a diary, in which they were instructed to record details of all physical activities undertaken during the 6-week training period, apart from the supervised training itself. A page from this diary is included in Appendix 1. The participants were verbally encouraged to continue with activities as normal, but to refrain from any weight training on either leg outside the training sessions.
In the second testing session, at the end of the 6-week intervention period (i.e. approximately 14 weeks after the ACLR surgery), the same tests were repeated. In addition, three jumping tests were also performed: the single leg horizontal jump, the single leg vertical jump and the single leg triple crossover jump (in this order). For all jump tests, the uninjured side was tested first and subjects repeated maximum effort jumps until there were two consecutive reductions in distance/height jumped. This method was used in order to ensure that maximum performance was exhibited and is based on the belief that no further gains would be made through practice and further reductions would occur due to pain or fatigue. For the horizontal and triple crossover tests, individual trials were considered successful if the subject landed on the test leg without losing balance. The trial with the maximum distance was used in later analysis.
The single leg horizontal hop has been shown to be a reliable [6, 7] test of knee function and is in common use [11]. Subjects performed the single leg horizontal jump test in bare feet. The subject stood stationary on the test leg, with the heel of the test leg aligned level with a start line. The subject was then encouraged to jump as far forwards as possible, with landing on the test leg on a sponge mat. The distance jumped was measured from the start line to the position of the heel on landing.
The vertical jump test was performed next. The single leg vertical jump has also been described as a reliable [7] test of knee function. Subjects stood in bare feet on a sponge mat in a marked rectangle to standardize starting position. The subjects stood with the frontal plane of the body at a right angle to the wall reaching as high as they could with their feet flat on the floor marking the wall with the tip of their chalked middle finger using the wall-side arm. This represented the baseline height. The subject then jumped as high as they could, re-marking the wall at the highest point of the jump. The distance between the baseline and the highest chalk mark was considered to be the maximum height jumped.
Following ACL injury, the triple crossover jump for distance is considered to be a potentially more sensitive test of knee dysfunction than other common jump tests since it imposes both frontal and rotational plane forces on the knee in addition to the predominantly sagittal plane forces that occur in linear functional performance tests [1, 9]. The triple crossover jump test consisted of an 8 m×15 cm course which required subjects to perform three consecutive jumps, without pausing between jumps, obliquely crossing the entire width of the course with each jump, to achieve the maximum possible linear displacement along the length of the course [23]. Comfortable shoes (e.g. running shoes) were worn for this test.
At the end of the post-test, patients were asked to fill in an anonymous questionnaire (Appendix 2) which asked at which site the patient had training and whether the patient had received any explicit or implicit information whilst at that site that might have biased the patient towards viewing one training regime (CKC or OKC) as superior to the other. This was done in order to detect any tendency for clinical staff at a site to impose any of their pre-existing opinions about the safety and efficacy of either regime on the patients and thus possibly influence the patients’ attitude to their training and recovery. We believed this was important given the common belief among clinicians that CKC training is superior.
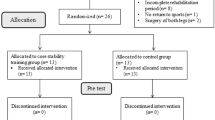
Training
After initial testing, subjects were assigned to one of two treatment groups (OKC training or CKC training) using block randomization and asked to attend physical therapy sessions three times per week for the 6-week training period of the study, starting as soon as possible after the pre-test. Because block randomization (four per block) was initiated prior to the inclusion of both hamstring and patella tendon surgery graft types, randomization was not separated for the two surgery types. Sessions occurred in the outpatient physiotherapy departments at one of four National Health Service hospitals in the London area [Mile End Hospital (MEH), St Thomas’s Hospital (STH), The Whittington Hospital (TWH) or Whipps Cross University Hospital (WCUH)]. All of the training sites had identical equipment for the key knee extensor training and other equipments were standardized.
The two treatment groups, groups CKC and OKC, differed in the type of isotonic resistance training used for their hip and knee extensors. Group CKC subjects performed unilateral CKC resistance training of the hip and knee extensors on a leg press machine (Horizontal Leg Press, Technogym UK, Bracknell, UK) with all these subjects using the same device for this exercise regardless of treatment site. The leg press machine was set so that the patient was supine with the hip and knee in approximately 90° of flexion for the start of each lift and the trunk slightly inclined from a parallel-to-floor position. From this position the leg was extended until the knee reached end-of-range extension.
Group OKC subjects performed unilateral OKC knee extensor resistance training using ankle weights or a knee extension/ham curl machine (Health and Leisure leg curl/extension machine, Walthamstow, UK). For the machine training, the subject sat with the knee and hip flexed to 90°, the axis of the knee joint level with the axis of the machine arm and with the shin bar resting just above the ankle joint. The weight was lifted to the end-of-range knee extension and then lowered gently. Ankle weight exercise was performed in the same way, with the weight strapped just above the ankle. The attending therapist used ankle weights if the subject was unable to lift the unloaded machine bar. The therapists were urged to use the machine as early as possible in the subjects’ training in order to allow greater standardization of the resistance loads. In addition, the hip extensors were also trained to achieve parity with the CKC group (for whom hip extensor exercise would have occurred concurrently during the leg press exercise). Ankle weights only were used for this exercise. The patient leaned on the edge of the plinth in a semi-prone position with ankle weights strapped around the distal tibia. The leg was lifted into extension with the knee semi-flexed, movement occurring from 90° hip flexion to full hip extension.
For the hip and knee extensor muscle resistance exercises, regardless of kinetic chain training type, three sets of 20 repetition maximum (RM) were used in each session until the beginning of week 4 of the 6-week intervention period, whereupon a switch to three sets of six RM was instituted. For all resistance exercise, a progressive resistance (i.e. load) programme was used with the load used dependent on knee pain and capacity of the target muscle group to move the load. Load was increased when the pain level was less than 5 (on a 0–10 scale reported verbally with 10 being the worst pain ever experienced and 0 being no pain) and the muscle group could successfully lift the load through the available range of motion for the target number or repetitions.
No other resistance training exercise was allowed for the knee extensors either in or out of the training sessions, apart from the relatively low-load step up and bicycle ergometer exercises, which will be described. Attempts were made to equalize the training velocity between the training groups for the hip and knee extensors. To control velocity, subjects used metronomes set to a target speed. The target speed setting used was 2 s for the concentric phase and 2 s for the eccentric phase of a training repetition with a 1 s interval between phases. These represent average angular velocities of 45°/s for the concentric and eccentric phases.
Both groups also followed a common core of other exercises and treatments, which had been chosen and agreed before the commencement of the study by the collaborating clinicians overseeing the training at each site. These were as follows:
-
1.
Ten minutes of cycling at 70 rotations per minute on a stationary ergometer (Tunturi F300, Tunturi Oy Ltd, Turku, Finland). The resistance level was chosen to provide the subject with a maximal challenge.
-
2.
Static stretching of the hamstrings, quadriceps, iliotibial band and calf muscles, using two holds of 15 s (30 s holds for the iliotibial band).
-
3.
Three sets of ten lunges. The patient stood in the long stride position, with the injured leg forwards and the toes of the rear foot aligned with the forward foot. The forward knee was bent slowly to 90° and then straightened.
-
4.
Patello-femoral and tibiofemoral Maitland mobilizations if appropriate [19].
-
5.
Soft-tissue mobilization if appropriate.
-
6.
Single leg proprioception exercises on a mini-trampette. The patient was progressed, using three repetitions of 30-s exercises, from unsupported balance on the trampette for 30 s on the injured leg, to hopping in place for 30 s with the eyes open, to hopping in place with the eyes closed for 30 s, to a hop with landing after a 180° turn with the eyes open. For the two middle stages, the subject also progressed from supported to unsupported hopping.
-
7.
Wobbleboard proprioception exercises for three sets of 30 s, progressing from unsupported standing on both legs to unsupported single leg standing whilst throwing and catching a ball.
-
8.
Lateral hops. Three sets of ten single leg hops side-to-side on either side of parallel lines (distance between lines equalling 30 cm increasing to 50 cm as the patient’s ability progressed).
-
9.
Figure Z hops. Three sets of ten repetitions of single leg hops in a figure Z outline between four points marked equidistant on the floor (40 cm apart).
-
10.
Isotonic resistance exercise of the hamstrings, using either a machine designed for this purpose, or ankle weights. The machine used was a knee extension/ham curl machine (Health and Leisure leg curl/extension machine, Walthamstow, UK) where ham curls are performed with the subject in a prone position. The knee was flexed from 0 to 90° knee flexion. The knee axis was aligned with the axis of the machine arm and the machine bar was placed just proximal to the ankle joint. Ankle weight exercises were performed in the same way, with the weights strapped just proximal to the ankle. Subjects were only allowed to use ankle weights if they did not have sufficient hamstring strength to use the machine. Hamstring exercises were performed at three sets of 20 RM progressing to three sets of 6 RM in week 4.
-
11.
Three sets of ten step ups on an 11.5-inch bench, leading up with the injured leg and leading down with the uninjured leg.
-
12.
Three sets of 20 calf raises.
-
13.
Interferential stimulation to decrease swelling if appropriate.
-
14.
Ice therapy to decrease swelling, used routinely for all patients in all sessions.
Details of all exercises or treatments were recorded on a sheet, which was returned to the examiners for data analysis at the end of the 6-week training period. By the end of the training period the therapy sessions routinely lasted approximately 1 h. No study restrictions were placed on the patient’s treatment before and after the study training period.
Data and statistical analyses
Non-nominal baseline and outcome data were tested for normal distributions using the Kolmogorov–Smirnov test. Baseline differences between groups were then analysed using an independent two sample t-test for normally distributed baseline measures, or the Mann–Whitney U test for non-parametric baseline measures. Nominal baseline data such as graft type, the existence of non-ACL pathology and surgery and the distribution of the groups across the four sites were analysed using chi-square tests. Baseline measures that were significantly different between groups were considered as potential confounding variables. Pre-test measures of the outcome variables were also automatically considered as confounding variables, as they were expected to influence the magnitude of the outcome measures. If a baseline measure was considered to have a potentially powerful effect on outcome, but was not significantly different between the groups, it was still considered as a possible confounding variable if there were large differences between the group means and, for categorical data, there were enough subjects in each category for meaningful analysis.
A univariate analysis of variance using SPSS version 10.1 (SPSS Inc., Chicago, USA) was used to analyse any difference in outcome variables (post-test values for the: injured leg laxity, Hughston Clinic score and the injured/uninjured ratio for distances jumped for the vertical, horizontal and triple crossover jumps) between the groups whilst considering all possible confounding variables. An independent t-test was used to analyse the differences between groups in terms of uninjured post-test laxity, as the uninjured leg was not thought to have been influenced by any of the confounding variables.
Results
Baseline and training data
Subjects were included in the data analysis if the number of days between surgery and pre-test were between 50 and 70 and if the number of days between pre- and post-test were between 35 and 55. Forty-nine patients successfully participated in the study (i.e. they fit these criteria and attended the pre- and post-test), with 25 in the CKC group and 24 in the OKC group. Their characteristics are summarized in Table 1. Whilst there were no significant differences (p>0.05) between the groups for these variables, it was deemed expedient to include the distribution of subjects across the four training sites as a possible confounding variable in the analysis of outcome as there were some large differences between the groups for these variables (e.g. the number of subjects training at MEH). Graft site was not included in the analysis of outcome because there were not enough subjects in each of the subcategories for meaningful analysis.
In addition to undergoing ACL reconstruction surgery, 36 subjects had one or more of the following when beginning the study: a history of meniscectomy (performed during the ACL-reconstruction or during a prior arthroscopy); a history of other surgical procedures performed at the same time as their reconstruction surgery; a history of prior ACL-reconstruction in the same or other knee; meniscal pathology not treated by surgery; medial or lateral collateral ligament pathology; and articular surface pathology. Any pathology was noted during the ACL reconstruction surgery, in any arthroscopic surgery that was performed prior to the ACLR surgery, or in a prior magnetic resonance imaging examination. Table 2 details the specific combinations of pathologies and additional surgeries received by subjects in both groups. A chi-square analysis was conducted on the differences between the groups in terms of numbers of those with co-existing pathology and/or a history of non-exploratory surgery and numbers of those with no such history. This analysis showed no significant differences (p>0.05) between groups. Despite this, we included the absence or presence of co-existing knee pathology and/or therapeutic surgery as a possible confounding variable in the outcome analysis for laxity and self-assessed knee function because of the large numerical differences between groups in some of the categories listed in Table 2 (e.g. the number of patients with no additional pathology or concurrent/prior therapeutic surgery). Co-existing knee pathology and/or therapeutic surgery was not included in the analysis of hop performance because there were not enough subjects in each of the subcategories for meaningful analysis.
Responses to the questionnaire (n=35) aimed at detecting bias towards one regime or another indicated that none of these patients had received any information that gave them any pre-conceived opinions about whether the group they were in was ‘better’ or ‘worse’ than the other. Hence patient bias relative to the training types was unlikely to be a factor contributing to any differences between the two treatment groups.
In terms of the equivalence of training across the two groups (Table 3), there were significant differences (p<0.05) in the total time spent on the bicycle ergometer. Cycling may have muscle training effects that could influence jump performance and subjective function, as well as direct effects on knee laxity [12]. Cycling duration was therefore considered a possible confounding variable in the outcome analysis. There were also significant differences (p<0.005) in the final session quadriceps load. The difference in final quadriceps load is expected given the additional contribution to force production provided by the hip extensors in the CKC exercise. As this difference can be considered an integral part of any difference between OKC and CKC training, it was not deemed necessary to consider final quadriceps load as a confounding variable in the outcome analysis.
Table 4 compares the two groups with reference to physical activities undertaken by participants outside the physiotherapy sessions (as noted in their diaries). There were no statistically significant differences (p>0.05) between the groups for these variables.
In summary, analysis of the baseline and intervention period data suggests that potential confounding variables to be considered in outcome analysis were: (1) time on the bicycle ergometer in physical therapy sessions; (2) training site; and (3) presence or absence of non-ACL pathology and therapeutic surgery (except for the hop test analysis where this variable was not considered). In addition, pre-test injured laxity and pre-test Hughston Clinic scores were also considered for significant confounding effects (though only for analyses involving their respective post-test outcome measure) as previously explained.
Outcome data
None of the patients in this study reported problems indicative of graft failure in the period between pre- and post-test. Table 5 illustrates the means and standard deviations of the outcome measures. No significant (p>0.05) differences were found between the groups for the outcome variables. For the analysis of the laxity data there was a significant interaction between post-test injured laxity and pre-test injured laxity (p<0.001) and the treatment groups were compared while accounting for this factor. There was a significant interaction between the pre- and post-test Hughston scores (p<0.001) and again the groups were compared using this factor as a confounding variable. The combination of training site and pathology/other surgery also showed a significant interaction with post-test Hughston scores (p=0.005) whereby patients without pathology/other surgery who trained at the Whittington Hospital had the highest Hughston scores.
Many subjects did not participate in the jump testing and this is detailed in Table 6. For the horizontal jump there was a significant interaction (p=0.033) due to site indicating that subjects who trained at WCH were more likely to perform poorly in this test (mean I/U ratio=68%, SD=15, n=11) while the subjects that trained at MEH and TWH exhibited the highest mean I/U ratio score of 83% (SD=12 and 16, respectively and n=5 and 9, respectively). Treatment group had no significant (p>0.696) effect on the horizontal hop injured/uninjured ratio. For the vertical jump there was a significant interaction (p=0.044) between group and site and Table 7 offers a more detailed description of the vertical jump findings classified by treatment group and training site. For the triple crossover jump there was no significant interactions (p>0.05) and the group effect was also not significant (p=0.851).
Discussion
Results from this study indicate that the OKC and CKC training programmes described do not differ significantly in their effects on knee laxity in the 8- to 14-week period after ACLR surgery. These results concur with those of Mikkelsen et al. [20] and our earlier findings [22]. However, Mikkelsen and colleagues’ study differed from ours in that it compared a CKC regime to a combined OKC/CKC regime. In addition, our earlier study looked at training during an earlier period after ACLR surgery than the present study. Hence, direct comparisons between the three studies are not possible.
In contrast, Bynum et al. [8] demonstrated significant differences in laxity between OKC and CKC groups during a similar post-surgical period to our study. One reason for the conflicting results could be that Bynum et al., like Mikkelsen et al., did not obtain an appropriate baseline ATD measurement and so we cannot be sure that the differences observed between groups were not partly due to baseline differences in laxity. Our finding of a significant interaction between laxity measured before and after the rehabilitation period underlines the importance of our decision to consider such baseline data in our analysis and has been supported by our previous work [21]. In addition, their different results can also be explained by the fact that their training regimes were conducted over a much longer period, with training commencing 6 weeks after surgery and final laxity testing occurring 19 months after surgery.
This study also demonstrated that the OKC and CKC regimes used do not differ in their effects on either subjective knee function (as measured by the Hughston Clinic Questionnaire) or objective knee function (as measured by jump performance) during the 8- to 14-week period post-ACLR. The subjective knee function findings agree with our previous work [14], although the earlier study concerned training in the 2- to 6-week period after ACLR. Bynum et al. [8], investigating the functional effects of OKC and CKC training in a similar period after surgery to the present study, also obtained similar results using the Lysholm questionnaire and the Tegner questionnaire. Bynum et al. [8] also used a questionnaire designed to measure satisfaction with surgical outcome, which again indicated no group differences, although for one question concerning speed of return to sport, subjects in the CKC group were significantly more satisfied. Mikkelsen et al. [20] used a similar questionnaire designed to assess subjects’ satisfaction with outcome and success in returning to sports 31 months after ACLR. In contrast to the findings of Bynum et al., Mikkelsen et al. found that although patients in each group were equally satisfied, patients in the combined group were significantly more likely to have returned to sport at the pre-injury level than their counterparts in the CKC group. It is possible, however, that these findings may merely reflect the greater training load experienced by the combined group rather than any effect specific to OKC exercise. Finally, caution is advised in interpreting outcome measures such as return to sport, as they are subject to many additional factors that are unrelated to knee function. Examples are level and type of sport and the subjective prognosis made by attending clinicians (who may be influenced by the patient’s training methods, such as the use of the more clinically accepted CKC training).
The objective knee function findings in the present study echo those of our earlier work [14], where objective function was evaluated during gait in the 2- to 6-week period post ACLR. In contrast, Witrouw et al. [32] compared the effects of 5-week programmes of CKC and OKC exercise on non-crossover triple jump performance in patients with patellofemoral pain and found that whilst the CKC group demonstrated significant improvements in performance from pre-test to post-test, the OKC group did not demonstrate any improvement. However, the OKC regime in that study largely consisted of isometric quadriceps training and end-of-range dynamic extension exercises, which prohibit meaningful comparison with our findings. Similarly, Augustsson et al. [3] compared 6-week regimes of OKC and CKC exercise in a study on uninjured subjects and demonstrated a significant improvement in vertical jump performance in the CKC group, but no such improvement in the OKC group. Augustsson and colleagues used a standing squat with free weights as their CKC exercise and isokinetic training as their OKC exercise, thus also preventing direct comparisons with the present study.
Significant associations were found in this study between some of the function indices and confounding factors. The finding that horizontal jump performance interacted significantly with the site is interesting in that it may, amongst other things, demonstrate varying levels of aggressiveness of therapy at different sites. Unfortunately, our data set is not large enough to allow meaningful comparisons of aggressiveness between the treatment sites in each treatment group. We are hopeful that future studies will consider the effects of different treatment sites on outcome measures and that possible causes for site differences will be investigated.
At first sight, the vertical jump (the outcome variable that was closest to showing statistically significant differences between groups) interaction with the training site and group combination appears to indicate that the VJ I/U ratio in the OKC group at STH was significantly different from some or all of the other seven site–group combinations. However, closer inspection of the VJ I/U ratios for the eight group–site combinations highlights a possible difference in the aggressiveness of therapy between OKC and CKC groups at certain training sites. CKC group VJ I/U ratios were 1.25 times higher than OKC group ratios at MEH and 1.44 times higher at STH. It is reasonable to assume that these results are not due to the intrinsic type of quadriceps training regime used, as similar results were not seen at the other two sites that used identical quadriceps training regime types. However, it is possible that the high VJ I/U ratios that selectively occurred at STH and MEH are due to the manner in which the quadriceps training regimes were applied. The most likely difference in application is more aggressive training in the closed group than the open group at STH and MEH, with a more equal level of aggression in both regimes at the other two sites. Before continuing, it should be pointed out that there is an alternative interpretation of these results: the lower OKC VJ I/U ratios at STH and MEH are due to real differences between the groups, but the similarity between OKC VJ I/U ratios at the other two sites is due to greater aggressiveness in the OKC groups masking the group effect. However, we feel this is a less likely explanation, as we would expect clinicians to tend towards less aggressiveness in the OKC group. Hence, if our assertion that more aggressive training occurred in the closed group than the open group at STH and MEH is true, then the overall OKC VJ I/U outcome may have been artificially lowered.
Therapy aggressiveness will influence the absolute quadriceps training load that is applied. We could not introduce absolute quadriceps training load (expressed as weight lifted) as a confounding factor in our analysis, as we were unable to meaningfully compare absolute training loads between groups because of the different muscles used in each type of exercise and the different mechanical advantages of the leg press and knee extension machines. Unfortunately, there are no papers in the literature that offer guidance for comparing the knee extensor loads in CKC and OKC exercise that are highly applicable to this study. Blackburn and Morrissey [5] measured maximum lifts (1 RM) for the leg press and the knee extension exercise on the Universal Multigym in 20 uninjured female subjects and found mean (SD) maximum lifts were 75 (29) kg for the leg press and 21 (5) kg for the knee extension, a maximum lift ratio of 3.6. We considered using such data to help us to ‘normalize’ the loads lifted in our present study. Such ‘normalization’ would involve multiplying the OKC absolute training load in the present study by the CKC:OKC maximum lift ratio noted above, thus yielding OKC values that could be usefully compared to CKC values. However, problems specific to ACL reconstruction, such as joint swelling or patellofemoral pain, would not be accounted for and machines identical to those used in our study would need to have been used to make valid use of the maximum lift ratio data as in the study by Blackburn and Morrissey. Similar data from ACLR patients would have been of greater use for such a ‘normalization’ procedure, but such data do not, to our knowledge, exist. Even if these data exist, they might be subject to the same confounding factors of clinician or patient attitudes that possibly occurred in this study (see below). Hence, in the absence of the ability to account for any lack of equivalence of training loads retrospectively, rigid prospective standardization of training loads is necessary.
We attempted to standardize the training load by using a repetition maximum prescription, with pain and muscle performance capacity acting as limiting factors to the load applied. Such a system may be vulnerable to bias arising from clinicians’ pre-conceived ideas about the safety or efficacy of the regimes. Results from a questionnaire indicated that patients were not being negatively influenced by any bias held by clinicians, although the ‘trustworthiness’ of the questionnaire was not evaluated. However, bias arising directly from the clinician was not formally assessed, either prospectively or retrospectively. An example of such direct bias could be a failure to stress the importance of using a heavy enough load to make the final few repetitions difficult, when instructing a patient using the supposedly less ‘safe’ exercise. Hence, we cannot evaluate whether or not our results were influenced by differences in the level of aggressiveness across groups. As previously argued, it is possible that results for the I/U vertical jump were skewed by such differences. It is also possible that other outcome variables may have been similarly affected.
We can conclude that with the training loads used in this study, CKC and OKC regimes do not differ in their effects on knee laxity or function, during the 8- to 14-week period after ACLR surgery. However, we cannot assume that greater training intensities would lead to the same results. Future studies should address this question, with attention to eliminating or recording any possible confounding clinician or patient attitudes towards OKC exercise. In the meantime, although OKC training using the training loads used in this study appears safe, we would reiterate our earlier conservative advice [22], which is to continue using only CKC training after ACLR surgery, as OKC training does not appear to offer any particular advantages over CKC training in patients who have had ACLR, and the evidence that exists about its harmfulness has not been fully refuted.
References
Anderson M, Foreman T (1996) Return to competition: functional rehabilitation. In: Zachazewski J, Magee D, Quillen W (eds) Athletic injuries and rehabilitation, chap 13. Saunders, Philadelphia, pp 229–261
Arms SW, Pope MH, Johnson RJ, Fischer RA, Arvidsson I, Eriksson E (1984) The biomechanics of anterior cruciate ligament rehabilitation and reconstruction. Am J Sports Med 12:8–18
Augustsson J, Esko A, Thomee R, and Svantesson U (1998) Weight training of the thigh muscles using closed vs. open kinetic chain exercises: a comparison of performance enhancement. JOSPT 27:3–8
Beynnon BD, Fleming BC (1998) Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech 31:519–525
Blackburn JR, Morrissey MC (1998) The relationship between open and closed kinetic chain strength of the lower limb extensors and jumping performance. JOSPT 27:430–435
Booher LD, Hench KM, Worrell TW, Stikeleather J (1993) Reliability of three single-leg hop tests. J Sports Rehabil 2:165–170
Brosky JAJ, Nitz AJ, Malone TR, Caborn DN, Rayens MK (1999) Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction. JOSPT 29:39–48
Bynum EB, Barrack RL, Alexander AH (1995) Open versus closed chain kinetic exercises after anterior cruciate ligament reconstruction—a prospective randomized study. Am J Sports Med 23:401–406
Clark NC, Gumbrell CJ, Rana S, Traole CM, Morrissey MC (2003) Intratester reliability and measurement error of the adapted cross-over hop for distance. Phys Ther Sport 3:143–151
Flandry F, Hunt JP, Terry GC, Hughston JC (1991) Analysis of subjective knee complaints using visual analogue scales. Am J Sports Med 19:112–118
Gaunt BW, Curd DT (2001) Anthropometric and demographic factors affecting distance hopped and limb symmetry index for the crossover hop-for-distance test in high school athletes. JOSPT 31:145–151
Grana WA, Muse G (1988) The effect of exercise on laxity in the anterior cruciate ligament deficient knee. Am J Sports Med 16:586–588
Henning CE, Lynch MA, Glick KR (1985) An in vivo strain-gauge study of elongation of the anterior cruciate ligament. Am J Sports Med 13:22–26
Hooper DM, Morrissey MC, Drechsler WI, Morrissey D, King JB (2001) Open and closed kinetic chain exercises in the early period after ACL reconstruction: improvements in level walking, stair ascent and descent. Am J Sports Med 29:167–174
Jaureguito JW, Paulos LE (1996) Why grafts fail. Clin Orthop Relat Res 325:25–41
Kennedy JC, Roth JH, Mendenhall HV, Sanford JB (1980) Presidential address. Intraarticular replacement in the anterior cruciate ligament-deficient knee. Am J Sports Med 8:1–8
Kohn D, Rose C (1994) Primary stability of interference screw fixation—influence of screw diameter and insertion torque. Am J Sports Med 22:334–338
Kurosaka M, Yoshiya S, Andrish JT (1987) A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 15:225–229
Maitland GD (1991) Peripheral manipulation, 3rd edn. Butterworth-Heinemann, Oxford
Mikkelsen C, Werner S, Eriksson E (2000) Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow up study. Knee Surg Sports Trauma Arthros 8:330–342
Morrissey MC, Hudson ZL, Drechsler WI, Coutts FJ, King JB, McAuliffe TB (2000) Correlates of knee laxity change in early rehabilitation after anterior cruciate ligament reconstruction. Int J Sports Med 7:529–535
Morrissey MC, Hudson ZL, Drechsler WI, Coutts FJ, Knight PR, King JB (2000) Effects of open versus closed kinetic chain training on knee laxity in the early period after anterior cruciate ligament reconstruction. Knee Surg Sports Trauma Arthrosc 8:343–348
Noyes FR, Mooar LA, Barber SD (1991) The assessment of work-related activities and limitations in knee disorders. Am J Sports Med 19:178–188
Palmitier RA, An K, Scott SG et al (1991) Kinetic chain exercise in knee rehabilitation. Sports Med 402–413
Prentice WE (1994) Closed-kinetic chain exercise. In: Prentice WE (ed) Rehabilitation techniques in sports medicine, 2nd edn. Mosby, London, pp 98–107
Queale WS, Snyder-Mackler L, Handling KA, Richards JG (1994) Instrumented examination of knee laxity in patients with anterior cruciate deficiency—a comparison of the KT-2000, Knee Signature System, and Genucom. JOSPT 19:345–351
Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF (1993) Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg 75A:1795–1803
Shelbourne KD, Klootwyk TE, DeCarlo MS (1992) Update on accelerated rehabilitation after anterior cruciate ligament reconstruction. JOSPT 15:303–308
Shelbourne KD, Nitz P (1992) Accelerated rehabilitation after anterior cruciate ligament reconstruction. JOSPT 15:256–264
Staubli HU, Jakob RP (1991) Anterior knee motion analysis—measurement and simultaneous radiography. Am J Sports Med 19:172–177
Steinkamp LA, Dillingham MF, Markel MD et al (1993) Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med 21:438–444
Witvrouw E, Lysens R, Bellemans J, Peers K, Vanderstraeten G (2000) Open versus closed kinetic chain exercises for patellofemoral pain—a prospective, randomized study. Am J Sports Med 28:687–694
Yack HJ, Collins CE, Whieldon TJ (1983) Comparison of closed and open kinetic chain exercise in the anterior cruciate ligament-deficient knee. Am J Sports Med 21:49–54
Acknowledgements
This study was supported by Action Medical Research, The Special Trustees of the Royal London Hospitals Trust and Technogym, UK. The authors would like to thank orthopaedic surgeons Messrs T. Bucknill, A. Davies, P. Earnshaw, M. El-Zebdeh, D. Goodier, M. Lamba, A. Lang-Stevenson, T.B. McAuliffe, D. Sweetnam and P. Thomas and physiotherapists M. Brown, W. Drechsler, J. Dredge, J. Jones, P. Knight, I. Man, B. Paton, R. Vauhnik and M. Yeboah for their support of this study.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Page from the diary for recording of activities undertaken outside therapy
Subject Number: —————
Date: ———
Please complete the following tables on a daily basis (you should have been given enough of these sheets so you have one for each day of the study period):
Appendix 2: Questionnaire for detecting patient bias resulting from communication with their clinician
Date: ———-
Please note that this questionnaire is anonymous. Any responses you make will be kept in the strictest confidence. Your clinician will not be told of your specific responses. The responses will help us better understand the results from this study. Please answer the following questions as accurately as possible.
-
1.
Please tick which one of these two exercises you performed during the study:
-
leg press (lying on back and pushing against plate)
-
knee extension (sitting on a bench and lifting a weight placed against your shin)
-
-
2.
During the study, were you ever given the impression that these two exercises differed in terms of how good they were?
-
Yes (please answer all the following questions)
-
No (please answer questions 5 and 6 only)
-
-
3.
Which of the two exercises was the so-called ‘better’ one?
-
leg press ((lying on back and pushing against plate)
-
knee extension (sitting on a bench and lifting a weight placed against your shin)
-
-
4.
Please describe who or what gave you the impression that one exercise was better than the other
-
5.
Please tick the hospital where you had physiotherapy:
-
Mile End The Whittington Whipps Cross St Thomas’s
-
-
6.
Please state the name(s) of the physiotherapist(s) who treated you during the study:——————————–
Thank you for taking the time to complete this questionnaire.
Rights and permissions
About this article
Cite this article
Perry, M.C., Morrissey, M.C., King, J.B. et al. Effects of closed versus open kinetic chain knee extensor resistance training on knee laxity and leg function in patients during the 8- to 14-week post-operative period after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 13, 357–369 (2005). https://doi.org/10.1007/s00167-004-0568-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-004-0568-7