Abstract
This paper reports the clinical outcome of the arthroscopic reduction and pull-out suture technique in acute and chronic displaced tibial spine anterior cruciate ligament (ACL) avulsion fractures. Between April 1997 and December 2000, 14 patients received an arthroscopic reduction and pull-out suturing of displaced tibial spine fractures (ACL avulsion fractures of tibia). Of 14 cases, ten were acute fractures and four were chronic nonunion fractures, in which all patients showed extension limitation. The mean follow-up period was 51 months (ranging from 30 to 80 months). At final follow-up, review of range of motion, Lachman test, anterior drawer test, KT-2000 arthrometer, Lysholm knee score, and Hospital for Special Surgery (HSS) score were evaluated. Compared to conventional pull-out suturing, several key modifications to surgical techniques were used. In all 14 patients, radiological bony union was detected at mean 12.3 weeks (range, 8–16 weeks) after surgery. All patients were able to return to their preinjury activity and sports level. At final follow-up, full range of motion was achieved in all patients. Anterior draw test, Lachman test, and KT-2000 (less than 3 mm side-to-side) were all negative in 13 patients. One female patient, who was 6 years old at the time of surgery, complained of no subjective instability, but showed Lachman grade I, and 5 mm side-to-side difference in KT-2000. She also revealed 10°̇ difference of genu recurvatum deformity. Two children (including the previously-mentioned 6-year-old female patient) showed leg-length discrepancy of 1 cm—the affected legs being longer—at final follow-up. The mean Lysholm knee scores were 95.6 (range, 92–100) and HSS knee scores were 96.4 (range, 91–100). Arthroscopic reduction with modified pull-out suturing technique in displaced tibial spine ACL avulsion fractures showed excellent union rate for both acute and chronic cases, without instability or extension limitations at minimum two-year follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Not infrequently, arthroscopic treatments of displaced tibial spine anterior cruciate ligament (ACL) avulsion fractures are reported with suboptimal clinical results; either with some limitation to knee extension or slight knee instability or both [1, 21]. The main causes of these unfavorable results seemed to be related with improper reduction and mild reduction loss, causing weakening of the ACL tension. Although several fixation methods, such as percutaneous K-wire fixation, screw fixation, and pull-out suturing are available, no single treatment can be apply to all types of fractures.
Meyers and McKeever [18] classified tibial spine fractures into three types. In addition, completely displaced type III was subdivided into types IIIA and IIIB, the former being merely displaced and the latter being displaced and rotated. Zaricznyj [23] added type IV in which the fragment was comminuted. Types III and IV are generally considered for surgical treatment.
The purpose of this study is to report the clinical outcome of the arthroscopic reduction and pull-out suture technique in acute and chronic displaced tibial spine ACL avulsion fractures.
Methods
Between April 1997 and December 2000, 14 patients underwent arthroscopic reduction and fixation of the displaced acute or chronic (nonunion) tibial spine ACL avulsion fracture, performed by one senior author (JHA). All patients received arthroscopic reduction and modified suturing method. There were six females and eight males. Among nonunion patients there were three females and one male. The mean age was 26 (range, 6–47); five patients were under 18 and nine patients were over 18 (Table 1).
Surgical indications were patients with fracture types III and IV [18] and any chronic displaced tibial spine showing nonunion. All patients either had acute displaced tibial spine fractures (ten) or chronic nonunion tibial spine fractures with instability and range of motion limitation (four). The mean postoperative final follow-up was 51 months (range from 30 to 80 months). According to fracture type classification [18] for acute fractures, four were type IIIA, three were type IIIB, and three were type IV. All four nonunion fractures were widely displaced, and were initially treated conservatively at other hospitals. The mean duration from injury to surgery for these nonunion was 21 months (range, 8–43 months).
The causes of injury were eight skiing accidents, two motor vehicle accidents, two bicycle accidents, and two falls. All of the acute fractures showed limitation in range of motion, hemarthrosis, and positive Lachman test. In nonunion cases, all patients showed knee extension limitations (approximately 10°) and grade II or more instability. oF 14 patients, three patients had combined injury; of these one had a medial meniscus radial tear and two had medial collateral ligament injuries (grade II). For the medial meniscus tear, partial menisectomy was performed and for the two patients with MCL injury, conservative therapy was applied after pull-out suturing.
All patients were followed at postoperative 2 weeks and every 4 weeks until union was observed. At the final follow-up, all patients were evaluated with the range of knee motion, knee instability test including Lachman test and anterior drawer test, KT-2000 arthrometer, Lysholm knee scores, and Hospital for Special Surgery (HSS) scores.
Surgical technique
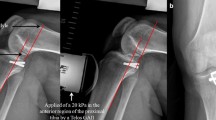
Standard knee arthroscopy was performed with anterolateral and anteromedial portals using a 30° 4.0 mm arthroscope (Linvatec, Largo, FL, USA). In all patients, we used an additional portal, the lateral mid-patellar portal for wider and better view of the intercondylar tibial eminence (Fig. 1). We removed hematomas, fibrin clots, ligamentum mucosum, and part of the infrapatella fat pad to improve the visual field. Small fracture fragments, and the transverse intermeniscal ligament which interfered with fragment reduction were also removed. In four nonunion cases, severe scarring and synovial hypertrophy was observed between the fracture fragment and tibial crater (crater made by avulsion of tibial spine). Only after removing these tissues and the transverse intermeniscal ligament with a shaver were we able to anatomically reduce the fragment. In six knees out of ten acute fractures, the avulsion fragment had attachment to the intact anterior horn of lateral meniscus. It is very important to anchor this attached meniscus to the tibia during fragment fixation. This can be achieved by creating a lateral hole piercing the anterior horn of lateral meniscus and by anchoring the meniscus together with the fragment (Fig. 2). We presumed this procedure might enhance blood supply to the fragment and also provide more stability to the reduced fragment. Furthermore, it eliminates any possibility of being an obstacle to the fracture reduction. First viewing from the lateral mid-patellar portal, a crescent suture hook (Linvatec, Largo, FL, USA) loaded with No. 0 PDS (Ethicon, Sommerville, NJ, USA) was introduced through the anteromedial portal. The suture hook pierces the ACL just above the superior border of the avulsion fragment, purchasing the whole thickness. The PDS is now advanced out through the hook, and, using the suture retriever (Linvatec, Largo, FL, USA) or other grasping material, the end is brought out to the anterolateral portal. Two ends are gathered with a hemostat for future identification. An additional two or more sutures are passed through the ACL fiber, making it parallel to the previous sutures. We recommend on average the placement of three or more sutures. After suture placement, a 2-cm longitudinal incision is made at approximately 3 cm distal to the joint line and midportion from the tibial tuberosity and medial edge of tibia (anteromedial aspect of proximal tibia). Two holes were drilled obliquely from proximal anteromedial tibia toward the crater of fracture site with the 2.7 mm ACL tibial guide. The position of the drilled hole is essential in making the reduced fragment stable. We carefully guided the hole to be placed in two important respects; first it is crucial to make this hole more anterior than the mid-transverse axis of the crater and second, unlike other reports where the hole is made within the crater, it is very important that the hole lies just outside the crater (Fig. 2). After making two anterior and outer positioned holes, an arthroscopic retriever (Arthrex, Germany) is introduced to each tunnel, retrieving each end of the suture, and is pulled out to the proximal and anteromedial aspect of tibia. After verifying good sliding of the suture materials, an SMC knot, preferably sliding [8], is made. A soft tissue is closed over the knot with firm skin suture. The reduced fragment is re-examined under scope vision with a probe testing its fixation during knee flexion and extension motion. A long leg splint was applied for 2 weeks and afterwards a limited motion brace was applied to control motion and gradually increase range of motion of the knee. Partial weight bearing was allowed until bone union, which was approximately 3 months.
Results
All 14 patients showed radiological bone union at mean 12.3 weeks (range, 8–16 weeks) postoperatively. For acute cases, the mean duration to union was 10.8 weeks (range, 8–12 weeks). For nonunion cases, the duration to union was 15 weeks (range, 12–16 weeks).
All 14 patients showed full range of knee motion, especially without any extension limitation at final follow-up. Thirteen patients showed negative Lachman test, anterior draw test and less than 3 mm side-to-side difference in KT-2000 arthrometer. The mean difference in KT-2000 arthrometer with contralateral control knee was 2 mm (range, 0–5 mm).
One female patient who was 6 years old at the time of surgery showed grade II Lachman and anterior draw test at final follow-up. At postoperative 52 months, she showed 5 mm side-to-side difference in KT-2000. She also showed more than 10° difference in genu recurvatum compared to the contralateral knee. Including the previously-mentioned child, the 6-year-old female and 11-year-old children showed aleg length difference of 1 cm, with the affected legs being 1 cm longer, at final follow-up.
The Lysholm knee score was on average 95.6 (range, 92–100), and the HSS score was on average 96.4 (range, 91–100) at final follow-up. Preoperative scoring was not available. All 14 patients were able to return to their preinjury activity level and participate in recreational sports activity.
Discussion
Although our study sample is relatively small in number, it shows an excellent union rate not only for the acute avulsion fractures but also for chronic nonunion avulsion fracture fragments (Fig. 3). Furthermore, all patients showed good clinical results with no instability at minimal two-year follow-up.
Eilert [5] first attempted arthroscopic reduction on tibial spine fracture with attached ACL in 1978. Since then, it has become a common practice to treat tibial spine fracture arthroscopically. Many fixation methods have been reported with promising results [2, 3, 7, 12–14, 16, 20, 22]. Although it is simple to use, K-wire fixation has difficulty in holding the fragment if the size is small. It is also more troublesome to maintain reduction during early postoperative rehabilitation using this method due to its weak holding power. Screw fixation, though it has strong purchasing power, due to its large size, can be applied only to a large fracture fragment [4]. Other disadvantages in screw fixation are possible breakage of fracture fragment during insertion, possible impingement of screw head during knee extension, and the requirement for a secondary procedure for screw removal [11, 12].
Both of these fixation methods cannot be applied to comminuted type IV fractures. Kogan et al. [10] recommended pull-out suturing in Meyers and McKeever type IV fractures where K-wire or screw fixation is not possible. In addition they insisted that pulling the inferior portion of ACL fiber by the suture helps to maintain the normal ACL tension [6]. The authors shared this theory and treated 14 consecutive patients with suturing technique. We were able to anatomically reduce and fixate the avulsion fragment using our modified suturing method. The anterior cruciate ligament regained its normal tension without any laxity. Baxter and Wiley [1] stressed 51% of anterior drawer test positive after operation and inevitable mild extension limitation. Kocher et al. [9]. also concluded that arthroscopic reduction and internal fixation of type III tibial spine fractures in skeletally immature patients results in persistent laxity but excellent functional outcome. However, in our study no patients showed any objective anterior instability, except in one child with Lachman test grade II where the patient did not have subjective instability. Additionally, all patients regained full range of knee motion without any extension limitation. This can be possibly explained by the additional tensioning effect of elongation ACL fiber during suturing using this fiber.
It seems that the good results are related to several modified techniques we used: (1) the lateral mid-patella portal secures good visualization of the operative field, (2) the 3 PDS#0 suture placement within the ACL fibers enhances firm fixation, and (3) the anterior and outer position of the drilled hole from the crater minimizes any anterior tilt or displacement. The main reason for anterior positioning is to reduce any tilting of the fragment after suture tightening. If the suture hole is placed in a more middle to posterior position, the anterior portion of the fracture fragment tends to tilt upwards, reducing the ACL tension. In addition, positioning of the hole just outside eliminates any possibility of suture blocking reduction and displacing the fragment.
As described before, it is important to make the hole pierce the anterior horn of the lateral meniscus when the fragment is attached. Hopefully it will somewhat enhance vascularity and stability. In this study, six of ten acute cases (more than 50%) showed attachment of lateral meniscus anterior horn (LMAH) to the avulsed fragment that was somewhat blocking the reduction. Matthews and Geissler [15] report one patient (out of six patients) who had LMAH blocking reduction of the fracture fragment. Several other articles in the literature [3, 19] report and recommend proper management of LMAH, which may act as an obstacle to the reduction. Our view is that this LMAH must be properly addressed during the surgery. Furthermore, whether it is blocking the reduction or not, it should be removed to the proper position and fixated along with the avulsion fragment.
Medial collateral ligament injury and lateral meniscus tear are prone to accompany ACL avulsion fracture [17]. It was true that in our study two patients (2/10) had combined MCL injury for acute tibial spine fracture. However, after fixating the ACL avulsion fragment, the instability on valgus stress markedly decreased, making it possible for us to treat MCL with conservative measurements (Fig. 4).
Two cases of growth disturbance were seen, the affected limb being 1 cm longer, in patients who were 6 and 11 years old at the time of surgery. The same 6-year-old patient had genu recurvatum deformity. We did not have preoperative leg-length measurement to compare with postoperative measurements. Hence we cannot make any conclusive statement that transepiphyseal tibial guide-pin tunneling had caused this growth disturbance. However, to avoid any possibility of growth disturbance it might be recommended that different fixation methods are used [19]. Otherwise, we think using the smallest-possible guide pin, possibly K-wire, for tunnel placement and suture passage would minimize the damage to growth plate. In addition, avoiding anterior epiphysis as much as possible might prevent genu recurvatum deformity.
Some authors [3, 15] comment on taking care not to harm the intermeniscal ligament during crater preparation before reduction. However, we had removed the transverse intermeniscal ligament during crater preparation in all cases, which in turn might aid good reduction and healing. We agree that the intermeniscal ligament has some role in stabilizing the anterior horn of both menisci; however, during fracture reduction this ligament tend to obstruct reduction, especially when the fragment is attached to LMAH.
We experienced good results in all cases regardless of age (young or adult), fracture type (large or comminuted), and fracture duration (acute or chronic). This led us to presume that this suturing method can be applied in a broad spectrum of patients. Although we need to add more cases and a longer period of follow-up, the results seem promising with regard to treatment of displaced tibial spine fractures arthroscopically.
Arthroscopic reduction with pull-out suturing technique in displaced tibial spine ACL avulsion fractures showed excellent union rate for both acute and chronic cases without instability or extension limitations at minimal 2-year follow-up.
References
Baxter MP, Wiley JJ (1988) Fractures of the tibial spine in children. An evaluation of knee stability. J Bone Joint Surg Br 70:228–230
Berg EE (1995) Pediatric tibial eminence fractures: arthroscopic cannulated screw fixation. Arthroscopy 11:328–331
Binnet MS, Gurkan I, Yilmaz C, Karakas A, Cetin C (2001) Arthroscopic fixation of intercondylar eminence fractures using a 4-portal technique. Arthroscopy 17:450–460
Davies EM, McLaren MI (2001) Type III tibial spine avulsions treated with arthroscopic Acutrak screw reattachment. Clin Orthop 388:205–208
Eilert RE (1978) Arthroscopy and arthrography in children and adolescent. In: AAOS symposium on arthroscopy and arthrography of the knee. Mosby, St Louis, p 12
Janarv PM, Hirsch G (2001) Growth influences knee laxity after anterior tibial spine fracture: a study on rabbits. Acta Orthop Scand 72:173–180
Jung YB, Yum JK, Koo BH (1999) A new method for arthroscopic treatment of tibial eminence fractures with eyed Steinmann pins. Arthroscopy 15:672–675
Kim SH, Ha KI (2000) The SMC knot—a new slip knot with locking mechanism. Arthroscopy 16:563–565
Kocher MS, Foreman ES, Micheli LJ (2003) Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy 19:1085–1090
Kogan MG, Marks P, Amendola A (1997) Technique for arthroscopic suture fixation of displaced tibial intercondylar eminence fractures. Arthroscopy 13:301–306
van Loon T, Marti RK (1991) A fracture of the intercondylar eminence of the tibia treated by arthroscopic fixation. Arthroscopy 7:385–388
Lubowitz JH, Grauer JD (1993) Arthroscopic treatment of anterior cruciate ligament avulsion. Clin Orthop 294:242–246
Mah JY, Otsuka NY, McLean J (1996) An arthroscopic technique for the reduction and fixation of tibial-eminence fractures. J Pediatr Orthop 16:119–121
Mah JY, Adili A, Otsuka NY, Ogilvie R (1998) Follow-up study of arthroscopic reduction and fixation of type III tibial-eminence fractures. J Pediatr Orthop 18:475–477
Matthews DE, Geissler WB (1994) Arthroscopic suture fixation of displaced tibial eminence fractures. Arthroscopy 10:418–423
McLennan JG (1982) The role of arthroscopic surgery in the treatment of fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Br 64:477–480
McLennan JG (1995) Lessons learned after second-look arthroscopy in type III fractures of the tibial spine. J Pediatr Orthop 15:59–62
Meyers MH, McKeever FM (1970) Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 52:1677–1684
Mylle J, Reynders P, Broos P (1993) Transepiphysial fixation of anterior cruciate avulsion in a child. Report of a complication and review of the literature. Arch Orthop Trauma Surg 112:101–103
Osti L, Merlo F, Bocchi L (1997) Our experience in the arthroscopic treatment of fracture-avulsion of the tibial spine. Chir Organi Mov 82:295–299
Panni AS, Milano G, Tartarone M, Fabbriciani C (1998) Arthroscopic treatment of malunited and nonunited avulsion fractures of the anterior tibial spine. Arthroscopy 14:233–240
Prince AR, Moyer RA (1995) Arthroscopic treatment of an avulsion fracture of the intercondylar eminence of the tibia. Case report. Am J Knee Surg 8:114–116
Zaricznyj B (1977) Avulsion fracture of the tibial eminence: treatment by open reduction and pinning. J Bone Joint Surg Am 59:1111–1114
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahn, J.H., Yoo, J.C. Clinical outcome of arthroscopic reduction and suture for displaced acute and chronic tibial spine fractures. Knee Surg Sports Traumatol Arthrosc 13, 116–121 (2005). https://doi.org/10.1007/s00167-004-0540-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-004-0540-6