Abstract
We evaluated 13 reconstructions of the lateral collateral ligament (LCL) of the knee associated with a reconstruction of the ACL (n=6) and PCL (n=7). In all cases the LCL was reconstructed using a semitendinosus tendon graft through a tunnel in the fibular head and fixed in anatomical insertion of LCL at lateral femoral condyle. Patients were evaluated using the IKDC form. Lateral joint opening and posterior tibial translation were studied by radiographic stress views. The follow-up average was of 60 months (38–93). In the ACL group five patient were symptoms free while one reported moderate pain after strenuous activity. The lateral stress radiographs showed lateral joint opening of 0–2 mm in five knees, and 3–5 mm in one. In the PCL group four patients were symptom free while three complained mild to moderate pain or swelling. Lateral joint opening was 0–2 mm in six knees and 3–5 in one. External rotation at 30° of flexion was 10° in one and between 0–5° in the remainder. Eleven of 13 patients returned to their preinjury level and two returned to one level lower. These findings indicate that the LCL can be successfully reconstructed with a free ST graft at the time of ACL or PCL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterolateral ligament injuries rarely present as an isolated entity. They are frequently associated with an anterior (ACL) or posterior cruciate ligament (PCL) injury. Failure to recognize and treat a posterolateral lesion addressing only the cruciate injury is a cause of failure of the ACL [1, 23] or PCL reconstruction [2]. In a study on 66 ACL revision operations 24% of the failures were attributed to an unrecognized posterolateral laxity [22]. Biomechanical studies have shown that in presence of a posterolateral laxity increased stresses are experienced by the ACL [12, 16], by the PCL [9, 16, 30], or by the grafts used to reconstruct them.
The structures of the posterolateral corner of the knee include both dynamic and static stabilizers. The iliotibial band, biceps tendon, lateral head of the gastrocnemius, and popliteus muscle are dynamic stabilizers. The lateral collateral ligament (LCL), arcuate ligament, flabellofibular ligament, and popliteofibular ligament (PFL) represent the static stabilizers [15, 17, 24, 27, 28]. Biomechanical studies have shown that the static stabilizers cooperate to restrain posterior tibial displacement, varus and external tibial rotation [7, 8, 26, 29].
In acute injuries of the posterolateral structures repair within 2 weeks is widely recommended. In the chronic injuries of the posterolateral structures reconstructive procedures are usually necessary. Several operations have been described. These include a proximal advancement of the posterolateral structures [11], biceps tenodesis [5], reconstruction of the LCL [14, 19], PFL, or popliteotibial ligament [13, 28]. A variety of autografts or allografts have been employed for this purpose.
Since 1992 we have employed a semitendinosus graft to reconstruct the LCL in chronic injuries. The associated ACL or PCL injury was reconstructed at the same time. We present here the results in our first 13 patients, with a minimum follow-up of 3 years. The results were evaluated clinically and radiographically. Objective stability against varus rotation was measured by the Telos device.
Material and method
Between 1992 and 1997 we treated 16 by reconstruction of lateral compartment (11 men, 2 women; mean age 26.8 years, range 17–36). Three of the patients (3 knees) received a biceps tenodesis, and 13 (13 knees) underwent a LCL reconstruction using a free semitendinosus graft. Only patients who underwent LCL reconstruction using a free semitendinosus graft were reviewed. All the operations were performed in the First Orthopedic Clinic of the University of Florence by the senior author (P.A.). Six knees had a combined ACL and seven a PCL lesion. All the injuries were chronic, with a mean period between injury and surgery of 19 months (range 8–50). The right knee was involved in six patients and the left in seven.
This study was retrospective analysis of these LCL reconstructions. The patients were examined using the IKDC evaluation form preoperatively and at the University of Florence [10]. One patient was examined during the period before publication of IKDC score, and we converted the findings from our earlier subjective and objective preoperative chart to the IKDC form. The physical examination included a varus stress test with the knee at 5–10° of flexion, where an attempt was made to estimate the opening of the lateral joint line in millimeters. The maneuver is enhanced by placing a finger over the joint line. External tibial rotation was evaluated with the patient supine and the knee flexed at 30°. A manual maximum force was applied to the medial margin of the foot. An increase in external rotation of 10° or more in comparison to the opposite knee was considered significant.
Posterior tibial displacement and lateral joint line opening at follow-up was measured with the Telos device (Samo, Bologna, Italy). To measure posterior tibial displacement the patient was placed in the lateral position with knee flexed at 70°. A posterior force of 15 kg was applied at the level of the tibial tuberosity. Lateral radiography was performed using an image amplifier to achieve superimposition of the femoral condyles To evaluate the lateral joint line opening the patient was placed supine with the knee in 5–10° of flexion. A laterally directed force of 15 kg was applied to the medial side of the knee and image amplifier oriented anteroposterior radiography was performed.
The original injury occurred during a sport activity in each of the six patients with a combined ACL lesion. In five patients the mechanism of injury was a varus force with internal rotatory component while in one patient it was not identified. Before the injury four patients were participating regularly in level I activities (pivoting-contact sports) and two in level II activities (agility sports). Preoperatively all the patients in the ACL group complained of pain, swelling, and giving-way episodes. Three patients were limited to level III activities (running) and three to daily living activities (level IV). The preoperative range of motion was complete in all the knees. Previous surgery included two medial arthroscopic meniscectomies, one lateral meniscectomy, and an acute repair of the lateral structures.
Of the seven knees with a combined PCL tear the original injury was sustained during a motor vehicle accident in four through a direct force against anteromedial proximal tibia of the flexed knee. Other three knees sustained the injury during a sport activity with a rotary component force associated with a direct blow to proximal tibia. Before the original injury six patients were participating in level I activities and one in level III. Preoperatively all the patients complained of pain, swelling and giving-way episodes and were limited to level III (n=3) or level IV (n=4) activities. All the knees showed a full range of motion preoperatively. Previous surgery included repair of an acute lesion of the lateral compartment in one knee and of the medial compartment in one.
Surgical technique
The patients were placed in the supine position. A pneumatic tourniquet was applied routinely. Reconstruction of the ACL or PCL was performed first. The ACL was reconstructed using an autogenous bone–patellar tendon–bone graft with an endoscopic single incision technique [25]. The PCL was reconstructed with an autogenous quadriceps tendon graft implanted with an open technique and a direct posterior approach and fixation to the tibia [3]. An anterior skin incision was used to harvest the quadriceps tendon graft. The joint was entered by a subvastus approach, and the necessary meniscal surgery was performed. A bone tunnel was produced into the medial femoral condyle to exit at the insertion of the anterolateral fibers in a shallow position. The graft was introduced with the bone plug into the tunnel and fixed with an interference screw. After the LCL reconstruction the patient was turned in the prone position, and the posterior proximal tibia was exposed using a posterior approach [4]. The graft was recovered from the anterior compartment, pulled posteriorly, tensioned, and fixed to the back of the tibia with two barbed staples.
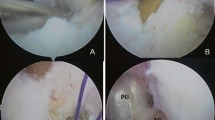
The semitendinosus tendon was harvested as a free graft through the anterior incision using a tendon stripper. The lateral aspect of the knee was exposed using a 15-cm longitudinal skin incision crossing over the Gerdy’s tubercle. The iliotibial band was incised longitudinally in its midline and the lateral femoral condyle was exposed. The head of the fibula was located and the peroneal nerve was isolated and protected. A 4.5-mm tunnel was drilled in the head of the fibula starting in front of the styloid and aiming 2 cm distally towards the neck. The semitendinosus graft was introduced into the tunnel and sutured to the soft tissues around the proximal tunnel exit. The iliotibial band was elevated from the underlying capsule and the graft was passed deep to it to reach the LCL insertion on the lateral femoral epicondyle. The tip of the lateral femoral epicondyle was located by finger palpation. This is enhanced by its sharp shape. The remnants of the LCL are also a useful guide to the correct insertion point. A 2.5-mm Kirschner wire was introduced into the lateral femoral epicondyle within the LCL insertional area. The semitendinosus graft was tensioned around the wire, and the knee was flexed from 0° to 120° with the tibia in the neutral position. In knees with a combined PCL injury care was taken to maintain the tibia reduced underneath the femur throughout the arc of motion. Changes in the distance between the ligament insertions were observed. We aimed at a 3–5 mm approximation of the graft insertion sites proceeding from extension to 110° of flexion. After identification of the correct femoral insertion point the Kirschner wire was overdrilled with a 6-mm cannulated drill bit. A bone tunnel was made in the distal femoral metaphysis, and the graft was introduced into the tunnel and fixed (Fig. 1).
In the knees with an associated ACL reconstruction the LCL was tensioned and fixed first with the knee in 20–30° of flexion, the tibia in neutral rotation and avoiding opening of the lateral joint line. Fixation was obtained with two barbed staples (Richards, Memphis, Tenn., USA) or with a screw and soft tissue washer. Then the ACL graft was tensioned and fixed with the knee in extension. In the knees with a combined PCL reconstruction the LCL was reconstructed, tensioned, and fixed with the knee at 30° of flexion. Afterwards the patient was turned in the prone position to perform a direct posterior approach to the tibia. The PCL graft was tensioned and fixed to the posterior intercondylar fovea of the tibia with two barbed staples.
Intra-articular pathology in the ACL group included: a total lesion of LCL in six knees, a longitudinal lesion of the medial meniscus in one (treated with partial meniscectomy), superficial fibrillation and fissuring of the cartilage of the medial femoral condyle in two and of the patella in two. Total lesion with partial scar tissue of ACL was seen in each. In the PCL group seven total lesions of LCL, one lesion of the medial meniscus, and three lesions of the lateral meniscus were seen These were treated with partial meniscectomy in two cases and with meniscal repair in two. Cartilage pathology included fissuring and fibrillation of the cartilage of the medial femoral condyle and patella in three knees No lesion of PFL or biceps complex in both group was recognized. The treatment of cartilage pathology was shaving of the lesions. No arthroscopic technique was performed in these cases.
Postoperatively a knee brace was applied, and motion was allowed in the range between 20° and 90° of flexion during the first month. If an ACL reconstruction had been performed, full extension was allowed twice a day, removing the brace. The range of motion was gradually increased during the second month but hyperextension was prevented. Weight-bearing was progressively allowed after the 6th postoperative week. Otherwise the rehabilitation followed the routine protocol after an ACL or PCL reconstruction. The patients were reviewed at an average follow-up of 60 months (range 38–93).
Results
In the six knees with a combined ACL injury the preoperative physical examination revealed (Table 1) a side to side difference in lateral joint line opening of 5–7 mm in four and of 8–10 mm in two. An increased external tibial rotation of 10° was present in three knees. Two knees had a 5° hyperextension compared to the opposite normal knee. The mean KT-1000 side to side difference in anterior tibial displacement at 30 lb was 10.6 mm (range 9–13). The pivot shift was 2+ in five knees and 3+ in one. Two patients showed a mild lateral thrust during walking.
At follow-up the side-to-side difference in lateral joint line opening evaluated with the Telos device was within 2 mm in 5 knees and 4 mm in one. There were no knees with an increased external tibial rotation over 5° at follow-up. A 3° hyperextension in comparison to the opposite normal knee was present in two. Five patients felt the knee subjectively normal and one nearly normal. Five patients were free from symptoms and one reported swelling after strenuous sport activities. Extension and flexion loss were absent in all the knees. The side to side difference in anterior tibial displacement measured with the KT-1000 arthrometer with a 30-Ib force was within 3 mm in all the knees. The pivot shift was negative in five cases and glide in one. Patellofemoral symptoms were present in one patient who complained of swelling after training with a mountain bike. At follow-up five patients participated regularly in level l and one in level II activities. The final result according to the IKDC form [10] was normal in five knees and nearly normal in one. The medial and lateral cartilage spaces were compared to the opposite normal knee in the anteroposterior weight bearing view. Preoperatively five knees showed a 1 mm narrowing of the medial cartilage space. At follow-up two knees had a 1–2 mm narrowing of the medial cartilage space.
The preoperative physical examination in the knees with an associated PCL injury (Table 1) showed that the side to side difference in lateral joint line opening was 6–8 mm in three knees and 9–10 mm in four. An increased external tibial rotation of 10–15° was present in three. Two knees had a recurvatum of 3–5° in comparison to the normal contralateral knee. The preoperative side to side difference in posterior tibial displacement was over 10 mm in all the knees. With the knee at 90° of flexion the tibial plateaus were flush with the femoral condyles in four knees and posterior to them in three. The reverse pivot-shift was negative in one knee, slight in two and marked in four. Three patients showed a subtle lateral thrust during the stance phase of the gait.
The physical examination at follow-up showed a side to side difference in lateral joint line opening within 2 mm in six knees and 4 mm in one. There was one knee with a 10° external tibial rotation at follow-up. Posterior tibial displacement evaluated with the Telos device was within 2 mm in two knees and 3–5 mm in five. There were no knees with an extension loss. Three knees showed a 6–15° flexion loss. A 5° hyperextension was present in two knees at follow-up. Four patients rated the knee subjectively normal and three nearly normal. Four patients were symptom free while three reported a mild to moderate pain and swelling after recreational activities. Patellofemoral crepitus with pain was present in one knee. At follow-up two patients participated in level I activities, four in level II and one in level III activities. The final result according to the IKDC form was normal in two knees and nearly normal in five knees. Preoperatively two knees showed a narrowing of 1 mm in the medial cartilage space. The radiographs at follow-up showed a narrowing of 1–2 mm in the medial cartilage space in three knees and of the patellofemoral space in one.
Discussion
Combined lesions involving the ACL and/or the PCL and the posterolateral structures, are severe injuries which cause significant functional limitations. Surgical treatment for these injuries is often required in both the acute and chronic phase. It is widely agreed that competent posterolateral structures are required to protect the ACL and PCL reconstructions [9, 12, 16, 30]. In the acute injuries repair of the lateral structures is usually sufficient to restore the stability of the knee. If this is not the case an augmentation procedure should be added. Reconstructive procedures for chronic injuries are a more challenging task. These operations are performed occasionally by most of the surgeons dealing with sports injuries. This fact contributes to the difficulty in standardizing the surgical techniques and collecting meaningful series to evaluate the results.
A tibial osteotomy is occasionally indicated in chronic posterolateral instabilities to correct a constitutional varus malalignment. These patients often show a major lateral thrust during the stance phase of the gait. In these knees soft tissue procedures are doomed to failure if the axis of the lower axis is not realigned. An additional indication to a valgus tibial osteotomy may be represented by those knees which have already progressed to an early medial osteoarthritis as a consequence of the lateral instability and medial overload. Patients with an indication to a tibial osteotomy were intentionally excluded from our study. The preoperative femorotibial anatomical angle was valgus in all the knees. There were no knees with an opening of the lateral joint line on the anteroposterior weight bearing view.
Several soft tissue procedures have been described to reconstruct chronic posterolateral rotatory instabilities. In 1985 Hughston and Jacobson [11] reported the results of 96 knees operated on with a detachment and advancement of the lateral epicondyle in an anterior and distal direction with the knee at 90° of flexion. A combined ACL rupture was present in 66 knees and was not reconstructed. At a follow-up of 2–13 years a satisfactory subjective, objective, and functional result was achieved in 78–85% of the cases. A modified advancement technique was proposed by Noyes and Barber-Westin [19]. The main differences to the series reported above [11] were that the associated ACL and/or PCL injuries were reconstructed, and that an attempt was made to minimize the displacement of the insertion of the posterolateral structures. A series of 21 knees was reviewed at an average follow-up of 42 months. A stringently functional rating for the posterolateral structures was developed. These structures were defined as functional if lateral joint line opening was less than 3 mm and external tibial rotation up to 5°. They were defined partially functional if the joint line opening was 3-5 mm and the external tibial rotation 6–10°. Using these criteria the posterolateral structures were functional in 64% of the cases and partially functional in 27%. The advancement technique is easier in comparison to the formal reconstructive procedures using auto- or allografts. The applicability of the advancement technique is limited to the cases in which the lateral structures have healed with interstitial elongation. If the lateral structures are detached distally or are definitely insufficient because of injury or previous surgery, the advancement cannot be performed. An additional criticism to this technique is that the anatomical insertion on the lateral epicondyle is altered, which may predispose to later stretching of the ligaments.
Tenodesis of the biceps tendon has been described by Clancy [5]. The operation involves preparation of the biceps tendon and its fixation into a bone trough centered in the upper one half of the lateral epicondyle. A screw and soft tissue washer are recommended. In a review of 49 knees operated on by this technique [5] there were 39 knees with chronic injuries and 10 acute. Of these injuries 43 were combined and 6 isolated. Eighty-two percent of the patients were satisfied at follow-up. Objective evaluation showed no reverse pivot-shift, symmetrical external tibial rotation and 0–2 mm of lateral joint line opening in 84–90% of the knees. Pain over the hardware was a frequent finding. Fanelli et al. [6] presented the minimum 2-year results of 21 knees operated on with an arthroscopically assisted PCL reconstruction using an Achilles tendon allograft and a biceps tenodesis as described by Clancy [5]. All the knees had preoperatively a posterolateral laxity as demonstrated by a positive reverse pivot shift, increased external tibial rotation at 30° and 90° and a positive posterolateral drawer test. This report does not mention the varus rotation test. Postoperatively the posterolateral instability was corrected in all the knees as shown by a negative reverse pivot shift and posterolateral drawer test. The external tibial rotation was decreased in relationship to the opposite knee in over one-half of the cases, suggesting an overcorrection.
Washer et al. [31] studied the in vitro effects of a biceps tenodesis after sectioning of the LCL and posterolateral structures. Using a femoral insertion point 1 cm anterior to the LCL they found that the procedure was effective in restoring external rotation and varus laxity. The operation actually overconstrained external rotation in all positions of flexion and varus angulation at 60° and 90°. This may affect the performance of the reconstruction in the long term. A fixation point 1 cm proximal to the LCL did not adequately control external rotation and varus laxity at 60° and 90° of flexion. The difference is due to the fact that an insertion point 1 cm anterior to the LCL insertion has an isometric behavior while the insertion point 1 cm proximal shows shortening of the distance between the ligament insertions proceeding toward flexion. It has been the experience of several authors as well as our own that it is not easy to have enough length in the biceps tendon to reach an insertion located anteriorly to the femoral epicondyle. The procedure cannot be performed in knees in which the biceps tendon had been detached distally by the previous injury. The need of postoperative splinting for 6 weeks to allow tendon healing limits the acceptability of the biceps tenodesis technique.
A further option is reconstruction of the fibular collateral ligament from the fibular head to the femoral epicondyle using autogenous or allograft tissue. Noyes and Barber-Westin [18] reported 20 LCL reconstructions performed with allograft tissue in knees in which local tissue was insufficient. The procedure involved production of two bony tunnels in the sagittal plane the first in the fibular head and the second across the lateral femoral epicondyle. Allograft tissue included the Achilles tendon (n=16), fascia lata (n=3), and bone–patellar tendon–bone (n=1). The posterolateral tissue was plicated over the fibular collateral ligament in a vest-over-pants fashion. Combined ACL/PCL injuries were also reconstructed with an average follow-up of 42 months a satisfactory lateral stability was achieved in 16 cases (76%). Three reconstructions showed a partial stretching and two failed. The authors emphasized the importance of connecting gait abnormalities and varus osseous alignment by means of tibial osteotomy.
Latimer et al. [14] reported ten patients with a combined ACL, PCL, ACL plus PCL, and posterolateral injury. The knees were treated by ACL or PCL reconstruction and an LCL reconstruction using a 9-mm patellar tendon allograft. The graft was fixed with interference screws into the fibular head and in the femoral epicondyle at a point 6 mm anterior to the fibular collateral ligament insertion. This point is believed to be the isometric. At a minimum 2-year follow-up six knees had no varus laxity, and four had up to 5 mm of increased lateral joint line opening compared to the opposite normal knee. Increased external tibial rotation at 30° of knee flexion was corrected in all the knees except one. The authors felt that a 9-mm patellar tendon allograft, which is much larger than the LCL, positioned at the isometric point on the lateral femoral condyle, may substitute adequately for the LCL as well as for the popliteofibular and arcuate ligaments. In a later comment to this article [20] it was observed that an increase of 3–5 mm in lateral joint line opening may not represent an excellent result, suggesting that reconstruction of the LCL and the posterolateral structures would afford a better stability.
Our results confirm those of Noyes and Barber-Westin [18] and Latimer et al. [14]. In a series of 13 knees with a posterolateral instability associated with an ACL or PCL injury the LCL reconstruction with the semitendinosus tendon was effective in correcting the lateral instability. The side-to-side difference in lateral joint line opening evaluated by the Telos device at follow-up was within 2 mm in 11 knees and 4 mm in two knees. Only one knee had a residual external tibial rotation of 10° at follow-up. According to the criteria expressed by Noyes and Barber-Westin [19] the lateral structures were functional in ten knees (77%) and partially functional in three (23%). The choice of the semitendinosus graft was convenient at a time when allograft tissues were not available for us The tensile strength of the LCL has been reported to be 309 N on average [26]. The sedimentinosus has a tensile strength of 1216 N on average [21]. It appears that a double semitendinosus graft has enough strength to adequately substitute the LCL.
We preferred to insert the LCL graft straight into the remnants of the native LCL. This positioning duplicates the normal anatomy and tensioning pattern of the LCL, which is tight in extension and relaxes in flexion to allow for the natural mobility of the lateral compartment. Recent biomechanical studies suggest that the LCL is tight in extension while the popliteofibular ligament tightens in flexion [26]. These observations support reconstruction of both the LCL and popliteofibular ligament [15, 29]. Further clinical studies are needed to confirm the effectiveness of these procedures.
References
Aglietti P, Buzzi R, D’Andria S et al (1991) Ricostruzione del legamento crociato anteriore per lassità cronica con il terzo centrale del tendine rotuleo: revisione a distanza di 3–9 anni. Ital J Orthop Traumatol 27:491
Aglietti P, Buzzi R, Menchetti PPM et al (1995) Reconstruction of the posterior cruciate ligament for acute and chronic injuries. J Sports Traumatol 17:231–241
Aglietti P, Buzzi R, Lazzara D (2001) Posterior cruciate ligament reconstruction with the quadriceps tendon in chronic injuries. Knee Surg Sports Traumatol Arthrosc 10:266–273
Burks RT, Schaffer JJ (1990) A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop 254:216–219
Clancy WG, Martin SD (1996) Posterolateral instability of the knee: treatment using the Clancy biceps femoris tenodesis. Operative techniques in sports medicine. Oper Techn Sports Med 4:182–191
Fanelli GC, Giannotti BF, Edson CJ (1996) Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy 12:521–530
Gollehon DL, Torzilli PA, Warren R F (1987) The role of the posterolateral cruciate ligaments in the stability of the human knee: a biomechanical study. J Bone Joint Surg Am 69:233–242
Grood ES, Stowers SF, Noyes FR (1988) Limits of movement in the human knee. J Bone Joint Surg Am 70:88–97
Harner CD, Vogrin TM, Hoeher J et al (2000) Biomechanical analysis of the posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med 28:32–39
Hefti V, Muller W, Jakob RP et al (1993) Evaluation of knee ligament injuries with IKDC form. Arthroscopy 1:226
Hughston JC, Jacobson KE (1985) Chronic posterolateral rotatory instability of the knee. J Bone Joint Surg Am 67:351–359
LaPrade RF, Resig S, Wentorf FA et al (1999) The effects of grade 3 posterolateral knee injuries on force in ACL reconstruction graft. A biomechanical analysis. Am J Sports Med 27:469
Larson RV (2000) Anatomy and management of posterolateral corner injuries. Instructional course lecture, 67th AAOS Meeting, March, Orlando, Florida
Latimer HA, Tibone JE, ElAttrache NS et al (1998) Reconstruction of the lateral collateral ligament of the knee with patellar tendon allograft. Report of a new technique in combined ligament injuries. Am J Sports Med 26:656–662
Markolf KL, Wascher DC, Finerman GA (1993) Direct in vitro measurement of forces in the cruciate ligaments. l. The effect of section of the posterolateral structures. J Bone Joint Surg Am 75:387–394
Maynard MJ, Deng XH, Wickiewicz TL et al (1996) The popliteofibular ligament: rediscovery of a key element in posterolateral stability. Am J Sports Med 24:311–316
Meister BR, Michael SP, Moyer RA et al (2000) Anatomy and kinematics of the lateral collateral ligament of the knee. Am J Sports Med 28:869–878
Noyes FR, Barber-Westin SD (1995) Surgical reconstruction of severe chronic posterolateral complex injuries of the knee using allograft tissues. Am J Sports Med 23:2–12
Noyes FR, Barber-Westin SD (1996) Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med 24:415–426
Noyes FR, Barber-Westin SD (1999) Letter to the Editor. Am J Sports Med 27:269–270
Noyes FR, Butler DL, Grood ES et al (1984) Biomechanical analysis of human ligament graft used in knee ligament repairs and recostructions. J Bone Joint Surg Am 66:387–394
Noyes FR, Barber-Westin SD, Roberts CS (1994) Use of allografts after failed treatment of rupture of the anterior cruciate ligament. J Bone Joint Surg Am 76:1019–1031
O’Brien SJ, Warren RF, Wickiewicz TL et al (1991) Anterior cruciate ligament reconstruction using central third patellar tendon in chronic insufficiency. J Bone Joint Surg Am 73:278
Scranton PE, Pinczewski L, Auld KM et al (1996) Outpatient endoscopic quadruple hamstring anterior cruciate ligament reconstruction. Oper Techn Orthop 6:177
Seebacher JR, Inglis AE, Marshall JL et al (1982) The structure of the posterorolateral aspect of the knee. J Bone Joint Surg Am 64:536
Sugita T, Amis AA (2001) Anatomic and biomechanical study of the lateral collateral and popliteofibular ligaments. Am J Sports Med 29:466–472
Terry GC, La Prade RF (1996) The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med 24:732–739
Veltri D, Warren RF (1994) Posterolateral instability of the knee. J Bone Joint Surg Am 7:460
Veltri D, Deng X-N, Torzilli R et al (1996) The role of popliteofibular ligament in stability of the human knee. Am J Sports Med 24:19–27
Vogrin TM, Hoeher J, Aroen A et al (2000) Effects of sectioning the posterolateral structures on knee kinematics and in situ forces in the posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 8:93–98
Wascher DC, Grauer JD, Markoff KL (1993) Biceps tendon tenodesis for posterolateral instability of the knee. Am J Sports Med 21:400–406
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buzzi, R., Aglietti, P., Vena, L.M. et al. Lateral collateral ligament reconstruction using a semitendinosus graft. Knee Surg Sports Traumatol Arthrosc 12, 36–42 (2004). https://doi.org/10.1007/s00167-003-0456-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0456-6