Abstract
Numerous studies have reported qualitative and quantitative analysis of nerve supply in the anterior cruciate ligament; however, as yet relatively little is known about the distribution of substance-P nerve endings in the human anterior cruciate ligament. The objective of this work was to evaluate the distribution of substance-P nerve fibers in intact human anterior cruciate ligament, and determine if rupture of the ligament has any influence on occurrence of these receptors. The intact anterior cruciate ligament group (group 1) of osteoarthritis knee, undergoing total knee arthroplasty, consisted of nine patients (eight females) with a mean age of 65.3 years at surgery. The anterior cruciate ligament rupture group (group 2) consisted of 20 patients (18 males and 2 females) with a mean age of 27.8 years at reconstruction. Healing time of the torn ligament in vivo, determined by the time period between the rupture and reconstruction, lasted from 1 to 40 months and the patients were divided into 3 groups (I, II and III) embracing diverse time periods. All harvested anterior cruciate ligaments were sectioned in thirds so that there was a proximal, middle and distal third for each ligament. The distribution of nociceptive receptors was studied by immunohistochemistry with monoclonal antibody to substance-P, including the semi-quantitative assessment. No significant difference was found between the number of substance-P nerve fibers in the proximal, middle and distal third of the intact anterior cruciate ligament ( p >0.05). During the first 4 months after injury (group I) the mean number of neuropeptide-containing fibers was greater in the proximal than in the distal third ( p =0.048996). The number of SP-positive nerve fibers in the proximal third decreased between 5 and 12 months after rupture, in a statistically significant manner ( p =0.045864). This study showed that distribution of the nociceptive nerve supply, positively stained for substance-P, is equal among the intact anterior cruciate ligament. The substance-P nerve ending density was significantly affected by the injury as well as by the time since rupture. The results of this study provide immunohistochemical evidence suggesting that between 1 to 4 months after rupture the site of the injury undergoes neurogenic inflammation, which could have an influence on the healing course of the torn ligament.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ruptured anterior cruciate ligament demonstrates a time-dependent histological response such as inflammation, epiligamentous regeneration, proliferation and remodeling. During these phases, different factors can elicit specific biological events such as cell proliferation, chemotaxis, matrix synthesis and secretion of other factors. The role of cytokines like transforming growth factor-β1, epidermal growth factor, fibroblast growth factor as well as tumor necrosis factor-α that affect the healing rate of the anterior cruciate ligament has been reported [9, 16, 26]. Current studies focused on the nociceptive afferent nerve supply about the knee using substance-P (SP) or calcitonin gene-related peptide (CGRP) immunoreactivity have suggested that SP and CGRP are neurotransmitters of the nociceptive sensation [25]. Numerous studies have reported the qualitative and quantitative analysis of mechanoreceptors in the anterior cruciate ligament; however, as yet relatively little is known about the distribution of substance-P nerve positive endings in an intact and ruptured human anterior cruciate ligament [3, 7, 11, 12, 14]. SP, which is released from sensory neurons upon axonal stimulation, has the ability to contract the smooth muscle in the bowel, and has been implicated in neurogenic inflammation. This undecapeptide increases the microvascular permeability, induces proliferation of lymphocytes, chemotactic for phagocytes and causes the release of inflammatory mediators [13, 18, 21].
One objective of this work is to evaluate the distribution of substance-P nerve fibers in the intact human anterior cruciate ligament. A second objective is to determine if rupture of the anterior cruciate ligament has any influence on the occurrence of nociceptive nerve endings, positively stained for substance-P.
Patients and methods
The anterior cruciate ligaments of two groups of patients were evaluated in this study. The material for investigation was obtained during anterior cruciate ligament reconstruction or total knee arthroplasty. All patients underwent complete clinical examination of the lower extremity as well as routine examination of the knee. The patients were informed about the research study and agreed to participate in the investigation. The Institutional Review Board Approval was obtained before beginning the study.
The intact anterior cruciate ligament group (group 1) of osteoarthritis knee, undergoing total knee arthroplasty, consisted of nine patients (eight females). The mean age at surgery was 65.3 years (range 49–72 years). The intact ligaments were resected from insertion sites without intact bony origin.
The anterior cruciate ligament rupture group (group 2) consisted of 20 patients (18 males and 2 females). The mean age of patients at reconstruction was 27.8 years (range 16–44 years). Healing time of the torn ligament in vivo, determined by the time period between the rupture and reconstruction, lasted from 1 to 40 months; the patients were not randomized to the different groups, but subdivided into 3 groups covering diverse time periods after rupture. Group I up to 4 months after surgery, group II 5–12 months after surgery, and group III more than 12 months after surgery. The number in each group and average time from injury were five, ten and five and 3.0, 8.9 and 31.0 months respectively. The mean age and female/male ratio of each group (I, II and III) were 27.8, 28.3 and 27.0 years and 4:1, 9:1and 5:0 respectively. The rupture of all ligaments was located near the femoral insertion site, without infringements of osseous origin, as confirmed by the X-ray investigation; the ligament was resected from the tibial insertion without intact bony origin. Patients with intact remnants to posterior cruciate ligament were excluded from the study.
All harvested anterior cruciate ligaments were sectioned into equally-sized thirds, as suggested by Arcand et al., so that there was a proximal (femoral), middle and distal (tibial) third for each ligament [3].
The biopsies were prepared for routine light microscopic observations. The tissue samples were fixed for 24 h in 4% buffered formaldehyde and embedded in paraffin. Afterwards, 5μ thick sections were stained with hematoxylin and eosin (H&E) and examined using Carl Zeiss (Jena) microscopy.
Immunohistochemistry
Paraffin sections were mounted onto superfrost slides, deparaffinized and Streptavidin-biotin complex technique was employed. After re-hydration, sections were reacted for 5 minutes with 3% hydrogen peroxide in distilled water and rinsed in Tris-buffered saline (TBS). Then slides were incubated with rabbit anti-human substance-P antibody (PEPA40, Serotec Ltd, UK) in dilution 1:2000 overnight at 4°C in a moist chamber. Afterwards, sections were rinsed in TBS, and the DAKO LSAB+/HRP Universal Kit (DAKO A/S, Glostrup, Denmark) was used according to the instructions of the manufacturer. The positive immunoreactivity was visualized with DAB as chromogen. After washing in distilled water, sections were counter-stained with hematoxylin and coverslipped. Negative controls were carried out by incubation in the absence of the primary antibody and always yielded negative results. The observation of substance-P reactivity was made using Carl Zeiss (Jena) microscopy.
Method of assessment of SP-immunopositive fibers
Slices excised from remnants or intact anterior cruciate ligaments were examined semi-quantitatively for nerve fibers showing substance-P expression. The measurements were made in ten consecutive visual areas at 400-fold magnification. In each field the number of SP-positive fibers was determined using the three-grade scale: 0—lack of nerve fibers showing expression of substance-P in the evaluation field, 1—one immunopositive nerve fiber in the visual field, 2—two or more fibers with substance-P expression in the visual field. Subsequently in each case the arithmetic mean of SP-immunopositive fibers was assessed for the ten visual fields.
Statistical methods
All values were expressed as mean±SD (standard deviation) (Table 1). The differences between groups were tested using Student’s t -test for independent samples, preceded by the evaluation of normality and homogeneity of variances with Levene’s test. Additionally the Mann-Whitney U test was used where appropriate. Results were considered statistically significant if p <0.05.
Results
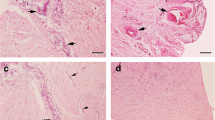
Using H&E staining, sections of biopsy specimens from group I showed increased vascularity and cellular congestion, mainly of fibroblasts, among collagen fascicles. In group II, the ligament consisted of dense bundles of collagen fibers, fibrocytes and small blood vessels. The intensity of the cellularity and vascularity was lower in comparison with ligament biopsies in group I. In group III, in most of biopsy specimens the vascularity and cell number density lowered to a level similar to that seen in group 1. In all groups the vascularity and cellularity appeared to decrease from proximal to distal.
Nerve fibers immunoreactive for SP were found in all examined intact anterior cruciate ligaments as well as in remnants. SP nerve fibers were most commonly associated with blood vessels, but there were free SP fibers which were not associated with any vascular profiles (Fig. 1). Immunopositive nerve fibers coursed parallel to the longitudinal axis of connective tissue fibers or vascular structures (Fig. 2).
In group 1, no significant difference was found between the number of substance-P nerve fibers in the proximal, middle and distal thirds of the anterior cruciate ligament (proximal vs middle p =0.6, proximal vs distal p =0.4, middle vs distal p =0.8). In group I the mean number of neuropeptide-containing fibers was greater in the proximal (site of injury) than in the distal third and this difference was statistically significant ( p =0.048996). No significant difference was found if the proximal vs middle thirds ( p =0.7) and middle vs distal thirds ( p =0.6) were compared in this group. There were no statistical differences in the distribution of substance-P nerve fibers in the proximal, middle and distal thirds in groups II and III ( p >0.05). The comparison of the specimens, from the same location, between the groups revealed that the proximal third of group I contained a greater number of SP-positive nerve fibers than the proximal third of group 1 (mean±SD 0.280000±0.204939 vs 0.111111±0.092796), however, the difference ( p =0.052169) did not reach significance. The proximal third of group II contained a lower mean number of immunopositive nerve fibers than the proximal third of group I, and the difference was statistically significant ( p =0.045864). There were no additional significant statistical differences in the distribution of substance-P nerve fibers in the proximal, middle and distal thirds of the ligament in each comparative group itself or between the groups ( p >0.05).
Discussion
Morphologic studies demonstrate that SP-immunoreactive nerve fibers are widespread in the soft tissue around the knee joint [2, 15, 19, 27, 28]. These tissues include the synovium, fat pad, menisci, ligaments and retinaculum. Prior study conducted by Witoński and Wągrowska-Danilewicz, on similar age-matched groups of patients, revealed no significant differences in the distribution of SP-positive nerve fibers in fat pad, medial and lateral retinaculum or synovium [27]. Also, to our knowledge there has been no prior study showing the significant effect of gender on distribution of SP nerve endings in the soft tissues around the knee. Therefore, analysis of data of this study was reliable enough to withdraw conclusions on the differences between the groups. The present study is the first report which has ever attempted to quantitative the distribution of substance-P nerve fibers in intact and ruptured anterior cruciate ligament. The significance of our study is that the distribution of SP-nerve fibers is equal in the proximal, middle and distal thirds of the intact ligament. This morphologic equality changed after the rupture, when the distribution of SP-positive nerve fibers varied in different part of the ligament. The time since injury was found to have a significant effect on staining for substance-P nerve fibers. The number of SP-positive nerve fibers increased during the four months after the lesion in the proximal third (which was the site of injury), if compared to the proximal part of the intact ligament as well as to the distal third of the ligament itself. The number of SP-positive nerve fibers decreased between 5 and 12 months after the rupture, in the proximal third, in a statistically significant manner, but after one year there are no statistically significant differences. The distribution of SP nerve fibers never in any part of the ruptured ligament decreased below the values observed in the intact ligament. Four distinct types of articular receptor endings (mechanoreceptors)—Ruffini endings, Pacinian corpuscles, Golgi tendon organ-like endings and free nerve endings—have been identified in human and other mammalian knee joints [15, 20]. The non-corpuscular endings (free nerve endings) are formed mainly by thinly myelinated group III and non-myelinated group IV, type a and b, afferent nerve fibers. Type IVa detect crude touch, pressure, pain, heat and cold; type IVb function as efferent vasomotors [10]. Studies conducted by Arcand et al. on the canine knee revealed that the proximal third of the anterior cruciate ligament contained a greater mean number of these receptors [3]. The authors found no statistical difference between the number of receptors between the middle and distal thirds. Zimny et al., based on morphometric analyses of human ligaments, showed that populations of mechanoreceptors are greater at the femoral and tibial ends and constitute nearly 2.5% of the ligament [29]. A similar observation was reported by Sjolander et al., who studied the histology of the cat anterior and posterior ligaments, where all receptors were most frequently found close to the tibial and femoral insertions [22]. The occurrence of free nerve endings in the soft tissue of the knee was studied by Biedert et al. [4]. The authors demonstrated that the highest levels of afferent nerve fibers type IVa are present in the retinacula, the patellar ligament, the pes anserinus and in the ligaments of Wrisberg and Humphry. The lowest level was found in the anterior cruciate ligament. The distribution of substance-P nerve endings observed in our study significantly differs in occurrence if compared with the distribution of other articular receptors, observed in numerous previous studies. We have found no significant difference in the distribution of SP-positive nerve endings in the proximal, middle and distal thirds of the intact ligament. Although most of the SP-nerve fibers were associated with blood vessels, their distributions varied in ligament vascularity. In the study of Murray et al., as well as in our own observations, vascularity of the intact ligament decreases proceeding from proximal to distal, whereas SP-fibers showed no changes in occurrence [17]. The presence of SP-positive endings unassociated with blood vessels may in part explain this difference. Denti et al. studied the fate of mechanoreceptors in torn and reconstructed anterior cruciate ligaments in humans, and observed that morphologically normal receptors remained in the ligament for 3 months after the injury, but gradually decreased after that time [5]. At 9 months post injury, only a few free nerve endings were observed, and were totally absent in the biopsy specimens from 1-year-old lesions. There is no doubt that injury of the anterior cruciate ligament decreased the number of mechanoreceptors, causing loss of proprioception. The increased number of SP-positive nerve fibers between 1 to 4 months post-injury observed in our study suggests that the anterior cruciate ligament may be susceptible to neurogenic inflammation, which occurs during the first phases following the rupture. Mediators known to contribute to the inflammatory process include cytokines, eicosanoids, complement and the kinin system, histamine and sensory neuropeptides substance-P and calcitonin gene-related peptide [21]. These sensory neuropeptides have potent trophic and vasodilatory properties, and as such are thought to be advantageous in wound repair. The appearance of the nerve fibers expressing peptides in other dense connective tissue undergoing healing is similar to our observations on remnants of anterior cruciate ligament. In studies conducted by Ackermann et al., CGRP-positive nerve endings were abundantly seen from 2 to 6 weeks post-injury in the proper Achilles tendon tissue undergoing healing [1]. Wallengren et al., using immunohistochemistry with antibodies against SP, CGRP, vasoactive intestinal peptide, neuropeptide Y and others in wound healing in rat skin, observed low nerve-fiber density in the wound tissue during the first few days after wound infliction, which started to increase on day 4, reaching a peak on day 7 [24]. Gronblad et al., based on the study of the experimentally-ruptured medial collateral ligament of the rabbit, noticed active involvement of neural elements in the healing process, which was suggested by kinetic studies showing a decrease in SP and CGRP staining as well as an increase in galanin staining during the study period [6]. However, Tamura et al. revealed that SP and CGRP are not always released, and work together in the joint under normal conditions [23]. Also, the data from the studies of Hanesch et al. indicate that acute inflammation induces the synthesis of CGRP but not of SP in joint afferents [8].
Murray et al. revealed, based on a patient profile similar to that for our study groups of patients, that the anterior cruciate ligament response to injury is similar to that reported for other dense connective tissue, such as fibroblast proliferation, angiogenesis and expression of α-smooth muscle actin, with three exceptions: formation of the α-smooth muscle actin-expressing synovial cell layer on the surface of the rupture ends, the lack of any tissue bridging the rupture site, and the presence of an epiligamentous reparative phase [17]. The authors suggest that a contiguous layer of α-smooth actin cells around a tissue could be responsible for retraction of the remnants of the anterior cruciate ligament. SP has the ability to contract the smooth muscle in the bowel (five times stronger than bradykinin). It is possible that this neuropeptide exerts a similar effect of contraction on α-smooth muscle actin cells of the connective tissue, causing contraction of the ruptured anterior cruciate ligament. Also it has long been known that fibroblasts often transform into myofibroblasts, which contain smooth muscle actin fibers and can therefore actively contract. This happens in pathological conditions like rheumatic arthritis, Dupuytren’s contracture and a few other inflammatory processes, and may occur at the inflammation phase of ligament healing.
In conclusion, this study revealed that distribution of nociceptive nerve supply positively stained for SP is equal in the proximal, middle and distal thirds of the intact anterior cruciate ligament. An abundant of SP-positive nerve supply, at the site of injury, between 1 and 4 months after rupture may indicate neurogenic inflammation. Since substance-P has the ability to contract smooth muscles in the bowel, one might suppose that during the first 4 months after injury it may also cause the most excessive contracture of α -smooth muscle actin, leading to retraction of the remnants of the anterior cruciate ligament. Also accepting that restoration of proprioception is the result of re-innervation of the anterior cruciate ligament, leaving the remnants as a source, we should take into consideration the possible influence of nociceptive innervation on bone-graft healing. The clinical significance of the results of this study, and the precise estimation of prevalence of responders in the population, at the present stage of knowledge, are unknown. A deeper understanding of the role of SP-positive nerve fibers in the pathophysiology of ruptured ligament healing, with the known effects of substance-P on fibroblasts, macrophages, inflammatory mediators as well as on blood vessels and smooth muscles will require further work on the role of nociceptive innervation in the torn anterior cruciate ligament.
References
Ackermann PW, Ahmed M, Kreicbergs A (2002) Early nerve regeneration after Achilles tendon rupture—a prerequisite for healing? A study in the rat. J Orthop Res 20:849–856
Ackermann PW, Finn A, Ahmed M (1999) Sensory neuropeptidergic pattern in tendon, ligament and joint capsule. A study in the rat. Neuroreport 10:2055–2060
Arcand MA, Rhalmi S, Rivard CH (2000) Quantification of mechanoreceptors in the canine anterior cruciate ligament. Int Orthop 24:272–275
Biedert RM, Stauffer E, Friederich NF (1992) Occurrence of free nerve endings in the soft tissue of the knee joint. A histologic investigation. Am J Sports Med 20:430–433
Denti M, Monteleone M, Berardi A, Panni AS (1994) Anterior cruciate ligament mechanoreceptors. Histologic studies on lesions and reconstruction. Clin Orthop 308:29–32
Gronblad M, Korkala O, Konttinen YT, Kuokkanen H, Liesi P (1991) Immunoreactive neuropeptides in nerves in ligamentous tissue. An experimental neuroimmunohistochemical study. Clin Orthop 265:291–296
Halata Z, Haus J (1989) The ultrastructure of sensory nerve endings in human anterior cruciate ligament. Anat Embryol (Berl) 179:415–421
Hanesch U, Heppelmann B, Schmidt RF (1997) Quantification of cat’s articular afferents containing calcitonin gene-related peptide or substance-P innervating normal and acutely inflamed knee joints. Neurosci Lett 233:105–108
Hannafin JA, Attia ET, Warren RF, Bhargava MM (1999) Characterization of chemotactic migration and growth kinetics of canine knee ligament fibroblasts. J Orthop Res 17:398–404
Heppelmann B, Messlinger K, Neiss WF, Schmidt RF (1990) Ultrastructural three-dimensional reconstruction of group III and group IV sensory nerve endings (“free nerve endings”) in the knee joint capsule of the cat: evidence for multiple receptive sites. J Comp Neurol 292:103–116
Hirasawa Y, Okajima S, Ohta M (2000) Nerve distribution to the human knee joint: anatomical and immunohistochemical study. Int Orthop 24:1–4
Kennedy JC, Alexander IJ, Hayes KC (1982) Nerve supply of the human knee and its functional importance. Am J Sports Med 10:329–335
Kolasinski SL, Haines KA, Siegel EL, Cronstein BN, Abramson SB (1992) Neuropeptides and inflammation. A somatostatin analog as a selective antagonists of neutrophil activation by substance-P. Arthritis Rheum 35:369–375
Krauspe R, Schmidt M, Schaible H (1992) Sensory innervation of the anterior cruciate ligament. An electrophysiological study of the response properties of single identified mechanoreceptors in the cat. J Bone Joint Surg Am 74:390–397
Marshall KW, Theriault E, Homonko DA (1994) Distribution of substance-P and calcitonin-related peptide immunoreactivity in the normal feline knee. J Rheumatol 21:883–889
Marui T, Niyibizi C, Georgescu HJ, Cao M, Kavalkovich KW, Levine RE, Woo SL-Y (1997) Effect of growth factors on matrix synthesis by ligament fibroblasts. J Orthop Res 15:18–23
Murray MM, Martin SD, Martin TL, Spector M (2000) Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am 82:1387–1397
Pernow B (1983 ) Substance-P. Pharmacol Rev 35:85–141
Sanchis-Alfonso V, Rosello-Sastre E (2000) Immunochistochemical analysis for neural markers of the lateral retinaculum in patients with isolated symptomatic patellofemoral malalignment. A neuroanatomic basis for anterior knee pain in the active young patients. Am J Sports Med 28:725–731
Schutte MJ, Dabezies EJ, Zimny ML, Happel L (1987) Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am 69:243–247
Scott DT, Lam FY, Ferrell WR (1994) Acute joint inflammation – mechanisms and mediators. Gen Pharmacol 25:1285–1296
Sjolander P, Johansson H, Sojka P, Rehnholm A (1989) Sensory nerve endings in the cat cruciate ligaments: a morphological investigation. Neurosci Lett 102:33–38
Tamura R, Hanesch U, Schmidt RF, Kumazawa T, Mizumura K (1998) Examination of co-localization gene-related peptide- and substance-P-like immunoreactivity in the knee joint of the dog. Neurosci Lett 18:53–56
Wallengren J, Chen D, Sundler F (1999) Neuropeptide-containing C-fibers and wound healing in rat skin. Neither capsaicin nor peripheral neurotomy affect the rate of healing. Br J Dermatol 140:400–408
Walsh DA, Salmon M, Mapp I, Garrett N, Blake D, Polak J (1994) Microvascular substance-P binding to normal and inflamed rat and human synovium. J Pharmacol Exp Ther 267:951–960
Witkowski J, Yang L, Wood DJ, Sung KL (1997) Migration and healing of ligament cells under inflammatory conditions. J Orthop Res 15:269–277
Witoński D, Wągrowska-Danilewicz M (1999) Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome. A preliminary report. Knee Surg Sport Traumatol Arthrosc 7:177–183
Wojtys EM, Beaman DN, Glover RA, Janda D (1990) Innervation of the human knee joint by substance-P fibers. Arthroscopy 6:254–263
Zimny ML, Schutte M, Dabezies E (1986) Mechanoreceptors in the human anterior cruciate ligament. Anat Rec 214:204–209
Acknowledgements
This study was supported by University of Łódź School of Medicine, grant # 502–11–713(64). The experiments comply with the current laws of Poland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Witoński, D., Wągrowska-Danilewicz, M. Distribution of substance-P nerve fibers in intact and ruptured human anterior cruciate ligament: a semi-quantitative immunohistochemical assessment. Knee Surg Sports Traumatol Arthrosc 12, 497–502 (2004). https://doi.org/10.1007/s00167-003-0453-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0453-9