Abstract
Extensive calcification of the patellar tendon following ACL reconstruction with central-third bone–patellar tendon–bone autograft is a rarely seen complication. A 45-year-old male patient underwent combined intraarticular reconstruction of ACL with 1/3 central patellar bone–tendon–bone graft and extraarticular reconstruction with modified MacIntosh technique. Two cm of calcification of the patellar tendon was observed incidentally when he underwent a high tibial osteotomy due to medial compartment degeneration, secondary to varus malalignment, 18 months after the ACL surgery. The calcification, being painless, was left untouched during the surgery. At the final examination, 136 months postoperatively, the patient still had no complaint relating to the patellar tendon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellar-tendon calcification following the removal of the central third for ACL reconstruction is an uncommon complication. This situation has been reported by a limited number of studies in the literature [9, 19]. The most frequent complications related to the patellar tendon harvesting site are fracture of patella [3, 5, 11, 16], avulsion or rupture of patellar tendon [2, 8, 12] and infrapatellar contracture syndrome (patella baja) [14]. This report describes a case of patellar-tendon calcification after ACL reconstruction surgery using bone–patellar tendon–bone as autograft with more than 11 years of follow-up.
Case report
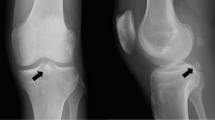
Intraarticular reconstruction of ACL with 1/3 central-patellar bone–tendon–bone graft and extraarticular reconstruction with modified MacIntosh technique were performed on a retired soccer player who was 45 years old in May 1991 (Fig. 1). The interval between the injury and surgery was 5 months. The patient referred to the clinic with knee pain and effusion 18 months after the operation. On clinical examination, minimal effusion, patella–femoral crepitus and increased sensitivity over the medial joint space were found. All stability tests were normal and range of motion was full. No complaint was observed on the donor site. Weight-bearing antero-posterior and lateral X-rays revealed narrowing of the medial joint space and also a calcification from the lower pole of the patella extending distally into the patellar tendon with 2 cm of length (Fig. 2). High tibial osteotomy with closed wedge was performed due to medial compartment degeneration and varus alignment. The calcification of the tendon was left untouched during the surgery, as it did not cause any symptoms. On later postoperative observation, the patient had no complaints over the patellar harvesting site, and no surgical decision was indicated (Fig. 3). Whilst the preoperative Lysholm knee score was 15, 136 months postoperatively it was found to be 100 when the patient came for the hard ware removal, and the calcification inside of the patellar tendon remained the same size as it was before (Fig. 4). Even though the patient had the same radiological view on his lateral X-ray of the knee, clinically he had neither limitation of range of motion nor a problem of sensitivity over the patellar donor site.
Discussion
Calcification of the patellar tendon can be seen in some disorders such as jumper’s knee [1], Sinding–Larsen–Johansson disease [18] or as a sequel of Osgood–Schlatter’s disease [6, 13]; however, all of which have different appearances. It may also form secondary to tendinitis [4] or trauma [10]. Spotted ossification of the tendon, which is not dense, is observed radiologically in all these situations. In this present case, this calcification was seen after ACL reconstruction using central 1/3 bone–patellar tendon–bone autograft.
Calcification of the patellar tendon as a complication of ACL surgery has been mentioned in a few reports [9, 19]. Lerat et al. [9] observed superior patellar-tendon calcification in their cases, but none of them was extensive. In their procedure, they filled tibial and patellar defects with bone debris from the drilling. They did not perform surgical removal in any patients, as all were without pain. In another study, Specchiulli et al. [19] had performed 75 cases of ACL reconstruction, and some of the patients showed slight radiographic evidence of intratendinous calcification at the latest follow-up.
Ossification in the quadriceps tendon after total patellectomy is a common finding. However it is very seldom found in the patellar tendon [7]. Patellar-tendon shortening as a result of cicatricial contraction is seen in about 10% in the literature [14], but the present case showed no shortening of the tendon associated with calcification.
Bone debris may trigger calcification, as it occurs in heterotopic ossification; however, bone cavities were not filled in our case. Cicatricial changes and vascular damage may be responsible for this calcification during the healing process. Bonamo et al. [2] stated the possibility of devascularization of the tendon during graft harvesting, which resulted in avascular degeneration. In the report of Mickelsen et al. [12], describing a patient of late patellar-tendon rupture after ACL reconstruction, they speculated that mechanical, histologic, and vascular properties of the remaining two thirds of the tendon had been altered. This alteration in vascularization, and also excessive loading, may result in focal degeneration followed by calcification.
Another possible pathogenesis may be aggressive rehabilitation in the early postoperative period which results in microtears within the remaining tendon. However, the same procedure and rehabilitation program were performed on all our series of ACL reconstructions, and none of them showed such extensive calcification. Lateral tibial tenodesis, which is the associated technique, does not add any surgical trauma to the patellar tendon, but it encourages the rehabilitation program [15, 17, 20].
This case shows that extensive calcification of the patellar tendon may form after removal of the central third for grafting. It is amazing that although it persisted for more than eleven years, it did not cause any complaint about either range of motion or pain.
References
Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ (1973) Jumper’s knee. Orthop Clin North Am 4:665–678
Bonamo JJ, Krinick RM, Sporn AA (1984) Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction. A report of two cases. J Bone Joint Surg Am 66:1294–1297
Christen B, Jakob RP (1992) Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg Br 74:617–619
Fritschy D, De Gautard R (1988) Jumper’s knee and ultrasonography. Am J Sports Med 16:637
Graf B, Uhr F (1988) Complications of intra-articular anterior cruciate reconstruction. Clin Sports Med 7:835–848.
Holstein A, Lewis GB, Schulze R (1964) Heterotopic ossification of patellar tendon. Bull Hosp Jt Dis 25:191–200
Kelly MA, Insall JN (1987) Postpatellectomy extensive ossification of patellar tendon. Clin Orthop 215:148–152
Langan P, Fontanetta AP (1987) Rupture of the patellar tendon after use of its central third. Orthop Rev 16:317–321
Lerat JL,Besse JL,Vincent P, Bontemps S, Limouzy F, Moyen B, Brunet-Guedj E (1995) Sequelae in the knee extensor system following graft removal for the “Mac in Jones” type procedure. Rev Chir Orthop Reparatrice Appar Mot 81:404–409
Matsumoto H, Kawakubo M, Otani T, Fujikawa K (1999) Extensive post-traumatic ossification of the patellar tendon. J Bone Joint Surg Br 81:34–36
McCarnal JR (1983) Fracture of the patella during a golf swing following reconstruction of the ACL. A case report. Am J Sports Med 11:26–27
Mickelsen PL, Morgan SJ, JohnsonWA, Ferrari JD (2001) Patellar tendon rupture 3 years after anterior cruciate ligament reconstruction with a central one third bone–patellar tendon–bone graft. Arthroscopy 17:648–652
Ogden JA, Southwick WO (1976) Osgood–Schlatter’s disease and tibial tuberosity development. Clin Orthop 116:180
Paulos L, Rosenberg TD, Dravbert J (1987) Infrapatellar contracture syndrome. An unrecognized cause of knee stiffness with entrapment and patella infera. Am J Sports Med 15:331–341
Richmond JC, Gladstone J, MacGillivray J (1991) Continuous passive motion after arthroscopically assisted anterior cruciate ligament reconstruction: comparison of short- versus long-term use. Arthroscopy 7:39–44
Roberts FS, Drez D, Parker W (1989) Prevention of late patellar fracture in ACL deficient knees reconstructed with bone–patellar tendon–bone autografts. Am J Knee Surg 2:83–86
Shelbourne KD, Klootwyk TE, DeCarlo MS (1992) Update on accelerated rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 15:303–308
Sinding-Larsen C (1921) A hitherto unknown affliction of the patella in children. Acta Radiol 1:171
Specchiulli F, Laforgia R, Mocci A, Miolla L, Scialpi L, Solarino G Jr (1995) Anterior cruciate ligament reconstruction. A comparison of 2 techniques. Clin Orthop 311:142–147
Zavatsky AB, Phil D, Beard DJ, O‘Connor JJ (1994) Cruciate ligament loading during isometric muscle contractions: a theoretical basis for rehabilitation. Am J Sports Med 22:418–423
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erdogan, F., Aydingoz, O., Kesmezacar, H. et al. Calcification of the patellar tendon after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 12, 277–279 (2004). https://doi.org/10.1007/s00167-003-0424-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0424-1