Abstract
Mucoid degeneration (MD) of the meniscus has received little attention. The pathology deserves special interest as it may lead to loss of the meniscus even in very young individuals. The cause of MD and the clinical features of meniscal tears due to that pathology have not been understood. This study analyzed the age profile and the role of trauma in patients with torn menisci with MD, examined meniscal tear patterns and clinical features, and investigated the role of bacterial infection in causing MD. Meniscal samples obtained from 27 consecutive patients during arthroscopic resection of torn menisci considered to be due to MD (typical yellow color) underwent pathological investigation. The samples were scored according to the light microscopic criteria of Copenhaver; 24 menisci (23 patients) with stage 2–3 MD comprised the study group. Magnetic resonance imaging obtained in 11 patients typically revealed increased intrasubstance signal intensity that extended to at least one of the meniscal surfaces. Pieces of resected meniscal tissue were also subject to PCR investigation to search for presence of bacteria. Of the 24 knees 21 (87%) had no history of trauma. Mean Tegner activity level was 4 (1 and 7). Mean duration of symptoms was 11.6 months (1–36). Pain was the most frequent symptom (n=22). Joint line tenderness and McMurray's test (pain and/or clicking) were present in 22 and 16 knees, respectively. Medial meniscus was affected in 16 and lateral meniscus in 8. Meniscal cyst and incomplete discoid meniscus was present in 5 and 2 of the lateral menisci. All of the torn menisci were degenerated and yellow in color. The most common tear patterns were radial and/or flap, and longitudinal-horizontal tears. PCR study revealed no bacteria. Mucoid degeneration of the meniscus does not seem to be related to the aging process. Clinical findings of torn such menisci are insidious compared to traumatic tears. Lack of history of trauma may delay the diagnosis. Bacterial infection has no role in the cause.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucoid or myxoid degeneration (MD) is a degenerative lesion characterized by an increase in the mucoid ground substance in the connective tissue containing glycoprotein and mucoprotein [5]. There is excessive accumulation of proteoglycans in interstitial tissue [21]. MD of menisci has been considered as a single entity which may present itself in one of two pathological forms: stromal MD and cystic parameniscal degeneration. The former type is an intrameniscal degeneration characterized by degeneration of fibrocartilage with an increase in mucoid ground substance that starts around the cells and extends progressively through the interstitial area. In the latter form degeneration is located in the parameniscal area and is characterized by integrated clefts and pseudocysts [5, 6]. MD has also been referred to as cystic degeneration [6, 17] and foamy degeneration [1].
Endogenous and exogenous trauma [16, 17, 21], endothelial inclusions in the cartilage during its development [14], chronic infection with hemorrhage [8, 21], and intraparanchymal hemorrhage [9] have been proposed as causes but without solid evidence. Meniscal MD is characterized by the typical yellow discoloration in the meniscal substance that appears as the torn meniscus is resected during arthroscopy. Such tears are usually irreparable. The disorder is encountered in considerable number of cases in the senior surgeon's (H.P.) experience. Despite the relatively common occurrence and the importance of the disorder only a few studies have appeared in the literature [6, 7].
Lack of knowledge in the literature on meniscal MD prompted the authors to study some aspects of the pathology. The purpose of the study was to analyze the age profile and the role of trauma in patients with torn menisci with MD, examine meniscal tear patterns and the clinical features, and investigate the role of bacterial infection in causing MD.
Materials and methods
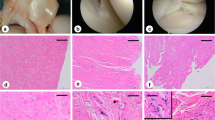
Excised pieces of tissue from 28 menisci (27 consecutive patients) considered during arthroscopy to have been torn due to MD underwent pathology laboratory for diagnosis and histological grading. The initial selection process was based on the degenerative nature of the tear that extended to at least one surface, and the typical yellow discoloration that appeared as the menisci were excised by mechanical instruments. The meniscal samples were taken only from the portions of torn meniscal tissue which have been excised arthroscopically. Meniscal samples were fixed in formalin and embedded in paraffin after tissue processing. The blocks were cut in 5.4-µm slides, and the slides were stained with hematoxylin-eosin. The slides were examined under ×100 magnification, and MD was scored according to the histological criteria described by Copenhaver et al. [3] (stage 0 n=1, stage I n=3, stage II n=9, stage III n=15; Fig. 1). Stage 0 represents normal meniscus, and stage I can be seen in asymptomatic individuals in the normal population [10, 18]. So, four patients were excluded from the study; thus the study group consisted of 24 menisci (23 patients) with stage II and III MD.
Histological classifications; hematoxylin-eosin stain, original magnification ×10. a Stage 0: homogeneous staining collagen with interposed chondrocytes (n=1). b Stage I: discrete foci of mucoid degeneration (n=3). c Stage II: bands of mucoid degeneration (n=9). d Stage III: mucoid degeneration combined with fibrocartilogenous separation (n=14)
There were 14 men and 9 women with an average age of 28 years (range 16–68); 17 patients were aged under 40 years. The left knee was involved in 9, the right in 14, and both in one. Detailed history and physical examination findings were recorded. Anteroposterior, lateral, tunnel, and axial radiographs were taken in all patients. Anteroposterior radiography was performed in supine position in patients aged under 40 years and in weightbearing position in those aged over 40 years. Orthoroentgenography was performed only when joint space narrowing and abnormal angulation was seen on the above radiographs. Patients with any signs of degenerative arthritis were not even considered for the arthroscopic selection process. Magnetic resonance imaging (MRI) was performed in 11 patients. All menisci were classified as grade III according to Stoller's [18] criteria, that is, all had increased signal intensity in the meniscal substance that extended to at least one articular surface in T1- and T2-weighted images; T1-weighted images were more typical. In most of the cases the signal intensity of the entire meniscus was increased, but the triangular borders of the meniscus were maintained (but broken in at least one point in some images) giving the appearance of a window. We describe these menisci as "empty" (Fig. 2). Arthroscopic findings and procedures were recorded in detail.
The meniscal samples taken during arthroscopic treatment were also sent to microbiology laboratory to search for bacterial presence by polymerase chain reaction (PCR). Presence of bacterial DNA was sought by PCR in which broad spectrum primers (P1–5′GAGGAAGGTAGGGACTGACGT3′ and P2–5′AGGCCCGGGAACGTATTCACCG3′) for bacterial 16 S rRNA gene were used. The yield was a 216-bp product. PCR was performed for 35 cycles of 1 min at 96°C, 2 min at 55°C, and 1 min at 72°C. After amplification the products were electrophoresed on %1.5 agarose gels in 1× Tris-borate-EDTA buffer and detected by ethidium bromide staining. Escherichia coli ATCC 25922 was included in all PCR reactions as positive controls.
Results
The mean duration of symptoms was 11.6 months (range 1–36 months). A history of trauma was present in only three knees (13%). Sixty-one percent of the patients were not active in sports. Mean Tegner activity level [20] was 4 (range 1–7). Pain was common in all knees. A history of locking was present in eight knees. Two patients reported episodes of giving way. Four patients had difficulty squatting. When asked, three patients reported knees to have experienced catching sensations. Joint line tenderness was present in 22 knees (13 medial, 7 lateral, 2 medial and lateral). McMurray's test (pain and/or clicking) was positive in 16 knees. All knees but one were clinically stable.
On arthroscopic examination all knees were found to have meniscal tears. All the torn menisci were degenerated and yellow in color (Fig. 3). In 15 knees there were isolated meniscal tears. One or more associated lesions were found in 8 knees: one torn anterior cruciate ligament, five lateral meniscal cysts (they were indeed cystic parameniscal mucoid degeneration; Fig. 4), and two incomplete discoid lateral menisci. Hypermobile menisci were noted in seven knees. Radial and/or flap and longitudinal-horizontal tears were the most common tear patterns (Table 1). There were 16 medial and 8 lateral meniscal tears. Seven partial meniscectomies (3 anterior to posterior, 3 middle-posterior two-thirds, 1 posterior one-third), 14 subtotal meniscectomies (5 anterior to posterior, 5 middle-posterior two-thirds, 4 posterior one-third), and three total meniscectomies (1 anterior to posterior, 2 middle-posterior two-thirds) were performed. The PCR evaluation revealed no findings corresponding to the presence of bacteria in meniscal samples taken during arthroscopy.
Discussion
The preservation of viable meniscus tissue is vital to maintain long-term knee function, and therefore every effort should be made to preserve them. Unfortunately, varying amounts of tissue need to be excised when the tears result from a degenerative process; the menisci are irreparable in this situation. Three degenerative lesions have been described in the meniscal tissue: dystrophic or metastatic calcification, hyaline acellular degeneration, and MD [5, 6].In our experience MD is the most frequent, and thus clinically the most significant one. It has been considered as a single entity which may present itself in one of two pathological forms: stromal MD and cystic parameniscal degeneration. Interestingly, the pathology seems to have received little attention in the literature despite its common occurrence.
The cause of both types of meniscal MD is usually attributed to endogenous and/or exogenous trauma [16, 17, 21]. In addition to trauma, Smillie [17] suggested that accumulation of mucopolysaccharides are also a response to nutritional deficiency. Ferrer-Roca and Vialalta [5] pointed to the possible role of mechanical strains and stated that intrameniscal stromal degeneration is a nonspecific reaction to injury and a physiological condition in all knees. Another study [10] as well as that mentioned above further suggested that stage I morphological changes are frequent in asymptomatic individuals. Ferrer-Roca and Vialalta [6] cited a study (Blanco, 1953) that proposed a traumatic origin for the displacement of synovial cells in the meniscus. According to Kleinberg [9], the degenerative process is secondary to a vascular disturbance initiated by trauma or other causes. Lindström [11] rejected the posttraumatic hematoma theory because he could find no microscopic signs of fresh or old hemorrhage in or around the lesion site. He did not totally disregard the role of trauma and added that it might play an aggravating role for some unknown factors that lead to degeneration.
McDevitt and Webber [12] proposed that the chondrocytes synthesize proteoglycans in response to altered mechanical stresses. Further support for the trauma theory comes from a study suggesting that the meniscus can respond aggressively to alterations in its environment and possibly to changes in load by increased synthesis and deposition of proteoglycans in its extracellular matrices [13]. The role of trauma is not supported by the present study because a history of trauma was present in only 13% of the patients. This also means that the tears were typically nontraumatic, and that the meniscal structure had been weakened by MD. Repetitive trauma also does not seem to play a role as 61% of patients were not active in sports, and average Tegner activity level [20] was relatively low. Varus and valgus angulations of the knee overloads the corresponding meniscus and may thus be a source of endogenous trauma. Although we did not record the mechanical axes for the patients, we encountered no patients with abnormal lower extremity axes; we perform orthoroentgenography whenever an abnormal angulation is suspected from weight-bearing anteroposterior radiography. No orthoroentgenography was needed. Based on the above features of our patient population we cannot agree with a prospective postexercise MRI study [15] that showed progressive degenerative changes in the menisci of football players over the course of a single football season. In addition to having no pathological confirmation in that study, there was no control group with sedentary patients. The authors did not explain why most of the menisci remained normal or stable.
Although some studies report lateral predominance [6, 17], this series obviously suggests higher incidence of medial involvement. This is also true for our cases after the completion of this series. Medial involvement is usually confined to the body of the medial meniscus due to its firm capsular attachment. Palpable cystic swelling is rare. Lateral cases may also be in the form of stromal degeneration or present as a cystic swelling. In the present study 5 of 8 lateral cases presented as cysts, in contrast to 16 medial lesions in which none displayed cystic presentation.
Lindström [11] has also proposed aging to be an etiological factor in degeneration of the meniscus. Aging may certainly lead to degeneration of the meniscus, as any other tissue, but MD seems to be a different entity that leads to premature degeneration. Our patient population with histological confirmation of MD demonstrated no physiological degenerative process. It should be stressed that the vast majority of these patients were aged under 40 years. Boden et al. [2] reported significantly more asymptomatic meniscal tears on MRI in patients older than 45 years. It should be noted that their series included physiologically degenerated menisci. Jean (1924), as cited by Ferrer-Roca and Vialalta [6] reported that MD was a degenerative condition that resulted from chronic infection and hemorrhages. PCR investigation in the present study revealed no presence of bacteria in mucoid degeneration.
MRI was performed in fewer than one-half of the patients, and a detailed analysis was not the subject of this study. However, a few comments can be made without drawing any conclusions. Whether grade II meniscal degenerations progress to symptomatic tears remains controversial and is not the subject of this study. During the course of this study we noted confusion in the literature regarding the MRI grading of meniscal degeneration. According to Crues et al. [4], grade I and II lesions show focal or linear increased signal intensity not extending to articular surfaces. Boden et al. [2] reported a 30% incidence of such grade II lesions in asymptomatic subjects, but these cases lacked histological confirmation. Stoller et al. [19] examined the correlation between MRI findings and a pathological model. The MRI appearances of the menisci in our series can be best described as tearing (grade III) superimposed on "extensive" grade I or II lesions because the entire meniscus in a single section showed increased signal and only the borders of the "meniscal triangle" displayed normal signal intensity. We refer to such menisci as "empty meniscus." The MRI findings of our patients are exactly the same as those of Hamada et al. [7], but our description of the images differ. In their group I menisci the high signal intensity is not linear and horizontal, as they state, but rather total intrameniscal degeneration. Also, in their example for group II the meniscus is "'empty," that is, it is left with its triangular borders. Hamada et al. [7] concluded that the finding of grade II (according to Crues et al. but indeed they are "empty" menisci) signals in the lateral discoid meniscus was of more clinical significance than noted in a nondiscoid meniscus. We have also seen same type of degeneration in nondiscoid lateral meniscus; it has been associated with cystic parameniscal degeneration in some of those cases and presents as a cystic swelling on lateral joint line. This swelling has been referred to as a meniscal cyst in the literature and is almost always associated with a tear. In this regard we propose that the meniscal cysts are indeed a type of mucoid degeneration. Due to loose capsular attachments they are usually encountered in the lateral meniscus, but after the completion of this series we have also seen some rare cases in the medial meniscus. The pathology usually seems to be confined in the medial meniscal substance.
To our knowledge, clinical data related to torn menisci with histological confirmation of MD have not been previously reported. Relatively long duration of symptoms before presentation means that such tears are usually not seriously symptomatic. We have encountered some patients who refused to undergo operation when they were called a few weeks after the diagnosis was made. Although they had pain, it was not serious, at least for some time despite having known that they had complex tears on MRI. The physical findings may also not be suggestive of a meniscal tear. The absence of history of trauma further delays the diagnosis. They are typically nontraumatic tears. Surprisingly, we have seen no studies on nontraumatic tears of the menisci. They are relatively common in our practice, and the results of arthroscopic meniscectomy following such tears will be reported in another study. If asked, some patients recall an instant when they felt minor pain on the stairs, while squatting, or while rising from a squat. Most of the time they do not recall even a minor event that led to sudden pain; the course is insidious and the symptoms are intermittent and develop gradually. Advanced MD ("empty meniscus" or "extensive" grade II on MRI) may give rise to joint line pain and tenderness even prior to being torn (grade III on MRI). The accumulation of mucopolysaccharides is responsible for this appearance, and it weakens the meniscal structure. The meniscus thus becomes prone to tearing. To our knowledge the tear patterns in menisci with histologically proven MD have not been previously reported. In the present series there were one longitudinal, three radial, and two displaced bucket-handle tears that sounds repairable, but this was not the case; closer look disclosed the extensive intrameniscal degeneration.
Tears of the menisci with mucoid degeneration are common in our experience. The pathology deserves special interest as it may lead to loss of the meniscus even in very young individuals. Unfortunately, such meniscal tears are not appropriate for repair most of the time. This study attempted to direct attention to mucoid degeneration, a disease of the meniscus that should be diagnosed and treated before it leads to tearing and loss of the meniscus. If it is diagnosed prior to tearing, patient counseling remains the only approach at the present time. A preexisting MD may be responsible for less than optimal healing following meniscal repair and allograft transplantation.
MD of the meniscus differs from physiological degeneration as it does not seem to be related to aging process. When menisci affected by MD are torn, the diagnosis may be delayed due to the lack of history of trauma and to relatively less severe symptoms. Bacterial infection is not a causal factor.
References
Barrie HJ (1979) The pathogenesis and significance of meniscal cysts. J Bone Joint Surg Br 61:184–189
Boden SD, Davis DO, Dina TS, Stoller DW, Brown SD, Vailas JC, Labropoulos PA (1992) A prospective and blinded investigation of magnetic resonance imaging of the knee: abnormal findings in asymptomatic subjects. Clin Orthop 282:177–185
Copenhaver WM, Kelly DR, Wood RL (1978) Bailey's textbook of histology. Williams & Wilkins, Baltimore, pp 170–178
Crues JV, Mink J, Levy TL, Lotysch M, Stoller DW (1987) Meniscal tears of the knee: accuracy of MR imaging. Radiology 164:445–448
Ferrer-Roca O, Vialalta C (1980) Lesions of the meniscus. I. Macroscopic and histologic findings. Clin Orthop 146:289–300
Ferrer-Roca O, Vialalta C (1980) Lesions of the meniscus. II. Horizontal cleavages and lateral cysts. Clin Orthop 146:301–307
Hamada M, Shino K, Kawano K, Araki Y, Matsui Y, Doi T (1994) Usefulness of magnetic resonance imaging for detecting intrasubstance tear and/or degeneration of lateral discoid meniscus. Arthroscopy 10:645–653
Hernandez FJ (1976) Cysts of the semilunar cartilage of knee: a light and electron microscopic study. Acta Orthop Scand 47:436–440
Kleinberg S (1938) Cysts of external semilunar cartilage: report of three cases. Arch Surg 37:827–834
Kornick J, Trefelner E, McCarthy S, Lange R, Lynch K, Jokl P (1990) Meniscal abnormalities in the asymptomatic population at MR imaging. Radiology 177:463–465
Lindström A (1950) Trauma and ganglia of the semilunar cartilages of the knee. Acta Orthop Scand 23:237–246
McDevitt CA, Muir H (1976) Biochemical changes in the cartilage of the knee in experimental and natural osteoarthritis in the dog. J Bone Joint Surg Br 58:94–101
McDevitt CA, Webber RJ (1990) The ultrastructure and biochemistry of meniscal cartilage. Clin Orthop 252:8–18
Ollerenshaw R (1921) The development of cysts in connection with the external semilunar cartilage of the knee-joint. Br J Surg 8:409–412
Reinig J, McDevitt ER, Ove PN (1991) Progression of meniscal degenerative changes in college football players: evaluation with MR imaging. Radiology 181:255–257
Romanini L, Calvisi V, Collodel M, Masciocchi C (1988) Cystic degeneration of the lateral meniscus. Pathogenesis and diagnostic approach. Ital J Orthop Traumatol 14:493–500
Smillie IS (1978) Surgical pathology of the menisci. In: Smillie IS (ed) Injuries of the knee joint. Churchill Livingstone, Edinburgh, pp 83–111
Stoller DW (1997) Magnetic resonance imaging of the knee: meniscal degenerations and tears. In: Stoller DW (ed) Magnetic resonance imaging in orthopaedics and sports medicine. Lippincott-Raven, New York, pp 257–262
Stoller DW, Martin C, Crues III JV, Kaplan L, Mink JH (1987) Meniscal tears: pathological correlation with MR imaging. Radiology 163:731–735
Tegner Y, Lysholm J (1985) Rating systems in evaluation of knee ligament injuries. Clin Orthop 198:43–49
Walter JB, Talbot IC (1996) Connective tissue: its normal structure and the effects of disease. In: Walter JB, Talbot IC (eds) General pathology. Churchill Livingstone, Edinburgh, pp 103–116
Acknowledgement
This study was financially supported by Dokuz Eylül University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boya, H., Pınar, H., Gülay, Z. et al. Clinical and arthroscopic features of meniscal tears and a search for the role of infection in histologically confirmed meniscal mucoid degeneration. Knee Surg Sports Traumatol Arthrosc 12, 294–299 (2004). https://doi.org/10.1007/s00167-003-0412-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0412-5