Abstract
Purpose
To test the effectiveness of a central venous catheter (CVC) insertion strategy and a hand hygiene (HH) improvement strategy to prevent central venous catheter-related bloodstream infections (CRBSI) in European intensive care units (ICUs), measuring both process and outcome indicators.
Methods
Adult ICUs from 14 hospitals in 11 European countries participated in this stepped-wedge cluster randomised controlled multicentre intervention study. After a 6 month baseline, three hospitals were randomised to one of three interventions every quarter: (1) CVC insertion strategy (CVCi); (2) HH promotion strategy (HHi); and (3) both interventions combined (COMBi). Primary outcome was prospective CRBSI incidence density. Secondary outcomes were a CVC insertion score and HH compliance.
Results
Overall 25,348 patients with 35,831 CVCs were included. CRBSI incidence density decreased from 2.4/1000 CVC-days at baseline to 0.9/1000 (p < 0.0001). When adjusted for patient and CVC characteristics all three interventions significantly reduced CRBSI incidence density. When additionally adjusted for the baseline decreasing trend, the HHi and COMBi arms were still effective. CVC insertion scores and HH compliance increased significantly with all three interventions.
Conclusions
This study demonstrates that multimodal prevention strategies aiming at improving CVC insertion practice and HH reduce CRBSI in diverse European ICUs. Compliance explained CRBSI reduction and future quality improvement studies should encourage measuring process indicators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Healthcare-associated infections (HAIs) result in increased morbidity, mortality, hospital stay, and additional healthcare costs. In Europe, an average of 6% of hospitalized patients are affected, but HAI prevalence differs between countries [1, 2]. Although some differences can be explained by case-mix variation, they may be also due to infection prevention and control (IPC) practices [3].
The Prevention of Hospital Infections by Intervention and Training (PROHIBIT) project, funded by the European Commission 7th Framework Programme, aimed to address and analyze the variation of IPC practices in Europe. Through its multiple work packages, PROHIBIT generated an overview of IPC at various levels [4–7], including the present study, with the objective of measuring the effectiveness of two interventions of known efficacy in the prevention of CRBSI in European intensive care units (ICUs) (https://plone.unige.ch/prohibit/publications). The results discussed here have partly been presented before, as abstracts [8–10].
Methods
Settings
Intensive care units from European hospitals were invited either through the European Center for Disease Prevention and Control (ECDC) national contact points for the HAI surveillance network (HAI-Net), or directly if registered in the European Antimicrobial Resistance Surveillance System. Eligible hospitals had to have a sufficient density of central venous catheter (CVC) use in the ICU and adequate diagnostic microbiological capacity. Germany and the Netherlands were excluded because the national surveillance protocols differed from the study protocol. Each hospital appointed a dedicated on-site investigator (OSI) and a study nurse. PROHIBIT offered reimbursement of a 0.5 full-time equivalent study nurse salary.
Study design
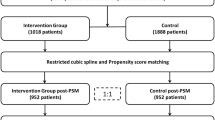
This study was conducted between January 2011 and June 2013. All adult patients (≥ 16 years of age) with a CVC inserted in a study hospital and admitted to one of the participating ICUs were eligible. The study followed a stepped-wedge, cluster randomized, controlled design (Fig. 1), which allowed control for secular trends, and enabled the comparison of hospitals with other hospitals and themselves. After a baseline of 6 months for all hospitals, every subsequent quarter, three hospitals were computer-randomized to one of three interventions: (1) a comprehensive CVC insertion strategy developed and successfully implemented at the University of Geneva Hospitals (CVCi) [11]; (2) a hand hygiene improvement strategy based on World Health Organization (WHO) recommendations (HHi) targeting the entire ICU-unit [12]; and (3) both interventions combined (COMBi) (more information in Supp. Methods). CRBSI was the primary outcome, process indicators, i.e. a CVC insertion score and hand hygiene compliance, were secondary outcomes. Interventions targeting quality of care were implemented at ICU-ward level (cluster level) whereas ICU patients were monitored for CRBSI and healthcare professionals for compliance.
Central venous catheters and CRBSI
Surveillance was performed prospectively by the local PROHIBIT study nurse. Tunnelled or peripherally-inserted central catheters, as well as CVCs already present at hospital admission or in situ for only one day were excluded. CVCs were followed up from insertion to removal. Dwell-time was censored in the case of CRBSI, beyond 48 h after ICU discharge, and after fatal outcome. CRBSI was measured as an incidence density (per 1000 CVC-days). Bloodstream infection (BSI) was defined according to the US Centers for Disease Control and Prevention (CDC) criteria for laboratory-confirmed BSI. CVC relation was defined using the ECDC HAI-Net criteria for microbiologically-confirmed CVC-related BSI (CRI3) [13], with the added criterion of the timely resolution of clinical symptoms after CVC removal or after starting antimicrobial therapy (Supp. Methods and results).
Process indicator surveillance
CVC insertion compliance was measured by direct observation using a list based on the CRBSI prevention protocol developed at the University of Geneva Hospitals (Supp. Figure 1) and expressed as the proportion of fulfilled protocol items divided by the total number of protocol items (CVC insertion score). Hand hygiene compliance was measured by direct observation according to the WHO “My five moments for hand hygiene” concept [14].
Observations of CVC insertion were randomized for date (weekdays) and place of insertion [ICU, operating theatre (if ICU patients regularly received the CVC there)] and were performed during daytime. Hand hygiene observations were randomized for date (weekdays), time slots (08–12:00, 12:00–16:00 and 16:00–20:00), and ICU beds. OSIs and study nurses were advised not to disclose any outcome or process indicator results during baseline. During the intervention, quarterly feedback reports on CRBSI and process indicator(s), according to the allocated intervention, were made available to OSIs by the project coordination team.
Co-variables
The recorded patient and CVC characteristics were age, sex, type of admission, type of ICU, length-of-stay, place of CVC insertion, insertion site, CVC type, number of lumens, indication for CVC insertion, and CVC dwell-time. Local study teams provided the Simplified Acute Physiology Score (SAPS) II or the Acute Physiology and Chronic Health Evaluation (APACHE) II score at patient admission, where available.
Training of study participants
Six weeks before the start of the study baseline the PROHIBIT study nurses were trained in the direct observation of CVC insertion and hand hygiene compliance at the University of Geneva Hospitals. Three to 6 months before the start of the intervention, study nurses and physicians attended a 2-day PROHIBIT workshop for training best practices and implementation science. Parallel to the WHO training material on hand hygiene (http://www.who.int/gpsc/5may/tools/en/), an e-learning program developed at the University of Geneva Hospitals was adapted to the PROHIBIT protocol and made available publicly at www.carepractice.net. Hospitals were encouraged to adapt the intervention program to their local context.
Implementation activities
The hospitals adapted CVC insertion procedures and introduced material (e.g. large drapes) as needed and feasible. They promoted strategy elements through educational sessions and bed-side training, using the WHO material and/or the Carepractice e-learning program. Some CVCi hospitals filmed the ‘old and new’ local insertion procedure to be used in educational sessions. All HHi hospitals applied posters and/or other reminders in the workplace and many came up with various additional activities. Detailed intervention activities are described in Supp. Tables 1a and 1b.
Statistical methods
For sample size calculations, we anticipated a baseline CRBSI incidence density of 3/1000 CVC-days. We hypothesized that the HHi-, CVCi-, and COMBi interventions would reduce CRBSI by 15, 35 [15], and 50% (alpha = 0.05; approximately 60% power for HHi, and over 80% power for CVCi and COMBi), respectively. χ 2 and exact tests were used to calculate 95% confidence intervals (CIs) for CRBSI incidence densities and compliance proportions. Differences between medians were tested with the Kruskal–Wallis test. CVC removal without CRBSI, discharge from the ICU with the CVC in place, and death were modelled as competing events for CRBSI (Supp. Methods and results) [16]. The association of the three interventions (CVCi, HHi and COMBi) with CRBSI incidence density was analyzed using a sub-distribution Cox proportional hazard analysis, stratified by hospitals. As patients can have more than one CVC, we adjusted for possible clustering at the patient level using robust covariance estimation. Records with missing values for a variable were excluded from the regression analysis of that variable. Patient and CVC characteristics with a p value < 0.2 were included in the multivariable regression model.
Following distribution of the dependent variables, the association of the interventions with the CVC insertion score was analyzed using generalized linear mixed modelling with a binomial distribution, and with hand hygiene using generalized linear mixed modelling with a normal distribution, both allowing for clustering at the hospital level. The association with professional category, type of ICU, shift, weekday, and activity index (number of hand hygiene opportunities per hour [17], averaged per quarter) was evaluated and these were included in the multiple regression model in case of a p value < 0.2.
All analyses were performed 1) without assuming a time-dependent trend, and 2) with assuming a baseline hospital-specific time-dependent trend and an additional intervention-specific time-dependent trend. Time was modelled as quarters during baseline (2 to a maximum of 6), and intervention (4 to a maximum of 8), assuming a linear trend. These models were fixed models, with hospitals included as a covariate to allow interaction terms of hospitals with the time-dependent trend.
The direct association of the two process indicators (CVC insertion score and hand hygiene compliance) with CRBSI incidence was explored using the quarterly averages of the CVC insertion score and hand hygiene compliance (both as percentages) and the quarterly CRBSI numbers, using Poisson regression modelling, allowing for clustering at the hospital level. Quarterly averages of covariates associated with CRBSI in the Cox regression model were evaluated in this analysis and included in the multiple regression model in case of a p value < 0.2. We used SAS software, version 9.3 for all statistical analyses.
Ethics
The medical ethical committees of all participating hospitals approved the study before randomization. In one centre individual patient consent was deemed necessary and therefore obtained.
Study registration
We retrospectively registered the protocol at the ISRCTN registry (ISRCTN24828982).
Role of the funding source
The PROHIBIT study was funded by the European Commission 7th Framework Programme. The study funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript. The study funder was not involved in the decision to submit the paper for publication.
Results
Participating hospitals
Fifteen hospitals were selected from 18 applicants to provide an even geographical distribution across Europe. Two hospitals dropped out before study start: one due to local ethics review board requiring individual written informed consent from patients, and one due to the workload anticipated by the ICU as non-feasible. One hospital was excluded during baseline because it failed to comply with the study protocol. Two of the three drop-out hospitals were replaced. Fourteen hospitals from 11 European countries completed the study: four were randomized to HHi, five to CVCi, and five to COMBi. Seven hospitals were university-affiliated. Four centres counted > 50,000 admissions per year, four between 30,000 and 50,000, and five < 30,000. The median (range) number of ICU beds per hospital was 30 (10–53). Median nurse-to-patient ratio in the ICU was 0.42 (0.25–1). Median [interquartile range (IQR)] activity index was 10.7 (8.2–12.7) hand hygiene opportunities per hour.
Patients and CVC utilization
A total of 25,348 patients with 35,831 CVCs were included in the study. Patient and CVC characteristics are summarized in Table 1 (per study arm) and Supp. Table 2 (overall). Patient and CVC characteristics differed significantly among the three intervention arms (Table 1). The APACHE II and SAPS II scores were available for only 35 and 37% of patients, respectively (Supp Table 3); and therefore excluded from the main analysis. CVC utilization decreased in all three intervention arms, but significantly only in the CVCi arm (Supp. Table 4). Median CVC dwell-times decreased in the COMBi arm (6 to 5 days, p < 0.0001), but did not change significantly in the HHi- (6 and 7 days, p = 0.41) and CVCi arms (5 and 5 days, p = 0.46).
CRBSI incidence densities
The overall CRBSI incidence density decreased from 2.4/1000 CVC-days at baseline to 0.9/1000 during the intervention (rate ratio, 0.39; 95% CI, 0.32–0.48; p < 0.0001). CRBSI incidences at baseline differed significantly between the three study arms: 2.0, 1.4, and 5.3/1000 CVC-days for HHi, CVCi and COMBi, respectively. Figure 2 shows the quarterly CRBSI incidence density for each study arm (results for each centre in Supp. Fig. 2). Table 2 shows the results of the univariable and multivariable regression analyses. CRBSI incidence density reduction between baseline and intervention was significant in all study arms. When adjusted in the multivariable regression analysis, the sub-distribution hazard ratios (HRsub; 95% CI) for the CVCi-, HHi-, and COMBi arms were 0.59 (0.43–0.81), 0.46 (0.28–0.74), and 0.33 (0.24–0.47), respectively.
Incidence density of catheter-related bloodstream infections (top), central venous catheter insertion scores (centre), hand hygiene compliance (bottom)—stratified by intervention arm. COMBi hand hygiene intervention and central venous catheter intervention combined, CRBSI central venous catheter-related bloodstream infection, CVCi central venous catheter intervention, HHi hand hygiene intervention, Q quarter. Of note: no CVC insertion scores during Q1
CRBSI incidence density tended to decrease already during baseline [HRsub 0.93; (0.84–1.02), per baseline quarter]. When adjusting for possible underlying hospital-specific trends and taking into account an intervention-specific trend, CRBSI reduction remained significant in the HHi- and COMBi arms: HRsub 0.37 (0.16–0.87) and 0.47 (0.27–0.83), respectively. In this model, CRBSI reduction was not significant in the CVCi arm: HRsub 1.16 (0.63–2.16). The interventions did not result in significant changes of the baseline trends (Supp. Methods and results). The overall median CVC dwell-time until infection was prolonged from 10 to 11.5 days (p = 0.042).
Microorganisms
The overall distribution of isolated microorganisms was as follows: Gram negative organisms: 44.0%; Gram positive organisms: 41.6%; Candida spp. 6.8%; and multiple organisms: 7.6%. The most frequent species were Acinetobacter baumannii (17.3%), Staphylococus epidermidis (15.7%), other coagulase negative staphylococci (CoNS) (14.1%), Klebsiella pneumoniae (9.7%), Pseudomonas aeruginosa (9.2%), Staphylococcus aureus (8.4%), Candida spp. (7.9%), Enterococcus faecium (4.7%), and E. faecalis (4.5%). CRBSI-reduction was significant for Acinetobacter baumannii [HRsub 0.39 (0.23-0.67)], Staphylococcus epidermidis [0.33 (0.19–0.56)], Pseudomonas aeruginosa [0.39 (0.18-0.83)] and CoNS other than S. epidermidis [0.04 (0.01–0.20)].
CVC insertion score
A total of 3572 CVC insertions were observed, i.e. 8.9% (IQR 6.4–15.6%) of all study CVCs. Supp. Table 5 shows the results for each insertion score element. CVC insertion scores improved in all study arms (Fig. 2, individual hospitals in Supp. Fig. 3): between baseline and intervention period, the mean insertion scores in the CVCi-, HHi- and COMBi arms improved from 69 to 92% [OR (95% CI): 4.0 (3.7–4.4); p < 0.0001], from 66 to 85% [1.3 (1.2–1.5); p < 0.0001], and from 78 to 96% [6.0 (5.5–6.6); p < 0.0001], respectively. The CVC insertion score per quarter improved already during baseline [OR 1.05 (1.02–1.09)]. When adjusting for the possible underlying hospital-specific trends and taking into account an intervention-specific trend, the odds ratios for the CVCi-, HHi-, and COMBi arms were 2.6 (2.2–3.0), 1.1 (0.6–1.3), and 3.4 (2.9–4.0), respectively. The improvement per quarter increased after the introduction of the intervention in the CVCi and COMBi arms [average additional OR 1.2 (1.1–1.5) and 1.5 (1.3–1.8), respectively], but did not change significantly in the HHi arm [OR 0.95 (0.9–1.1)].
Increasing CVC insertion scores were significantly associated with decreasing CRBSI incidence density: the incidence rate ratio (95% CI) per percentage point (PP) increase of the CVC score over the entire study was 0.97 (0.96–0.98). After adjustment for the proportions of patients with bloodstream infection at the time of insertion and of patients with prolonged ICU stay before insertion, this association remained significant with an incidence rate ratio of 0.97 (0.96–0.98) for the entire population, and for both the CVCi and COMBi arm; however, the adjusted association was not significant in the HHi arm (Supp. Table 6).
Hand hygiene compliance
A total of 59,122 hand hygiene opportunities were observed during 6749 observation sessions. Nurses were the main contributors (74.4%), followed by medical doctors (14.5%), auxiliaries (8.8%), and other healthcare professionals (2.3%). Overall hand hygiene compliance at baseline averaged 49%.
Between baseline and intervention period, hand hygiene compliance in the CVCi-, HHi- and COMBi arms improved from 51% (50–52%) to 62% (61–63%; p < 0.0001), from 36% (34–37%) to 58% (57–59%; p < 0.0001), and from 54% (52–55%) to 63% (62–64%; p < 0.0001), respectively (Fig. 2, individual hospital data in Supp. Figure 4). During baseline, hand hygiene compliance decreased by − 1 (− 2 to − 0.05) percentage points (PPs) per quarter. When adjusted for healthcare professional category, ICU type and activity index, improvement of hand hygiene compliance in the CVCi-, HHi-, and COMBi arms was 6 PP (4–8 PP), 20 PP (18–22 PP), and 8 PP (7–10 PP), respectively. When adjusted for underlying hospital-specific trends and taking into account an intervention-specific trend, improvement of hand hygiene compliance in the CVCi-, HHi-, and COMBi arms was 10 PP (6–14 PP), 18 PP (15–22 PP) and 6 PP (3–9 PP), respectively.
Hand hygiene compliance improved in all four healthcare professional categories in the HHi- and COMBi arms, while hand hygiene compliance in the CVCi arm improved only in nurses (Supp. Table 7). HH compliance by indication is displayed in Supp. Table 8.
As with the CVC insertion score, increasing hand hygiene compliance was associated with decreasing CRBSI incidence density: the incidence rate ratio (95% CI) per PP increase of hand hygiene compliance over the entire study was 0.99 (0.98–1.00). After adjustment for the proportions of patients with bloodstream infection at the time of insertion and of patients with prolonged ICU stay before insertion, this association did not remain significant, with an incidence rate ratio of 1.00 (0.99–1.01) for the entire population, and for the CVCi- and COMBi arms. However, the adjusted association was significant in the HHi arm (Supp. Table 6).
Discussion
Our results demonstrate that the introduction of a best practice CVC insertion strategy, a WHO-based HH promotion strategy, and the combination of both, significantly improve process indicators and reduce CRBSI incidence densities. When taking into account a decreasing trend during baseline, both the HH program and the combined HH and CVC insertion strategy were still effective. The low baseline rates in the CVCi arm limited the power to demonstrate the same effect in this arm.
This is the first multinational randomized multicentre CRBSI prevention study providing sufficiently powered information on both outcome and process indicators. Many studies have reported successful CVC insertion or hand hygiene improvement initiatives [18–22]. However, most CRBSI prevention studies reported outcome data only, without mentioning process indicator data, as evidenced in a recent systematic review by Ista et al. [18]. In a randomized Canadian study, compliance with CRBSI-prevention measures increased from 10% at baseline to 70% during intervention in the intervention ICUs, while compliance increased from 31 to 52% in the control ICUs [20]. The study did not report CRBSIs and numbers of CVCs were low. Non-randomized before-and-after studies, partially using retrospective data, have reported CVC “bundle” compliance in the range of 20–37% [23], 55.2% [24], 74% [25] and 90–100% [21, 26, 27]. An Australian multicentre study reported variation of bundle compliance between hospitals ranging from 0 to 100% (personal communication from McLaws) [21]. Most studies used an “all or nothing” approach, where the outcome was met if all items of the bundle were fulfilled. Our CVC checklist consisted of 20 items, which is beyond the usual bundle promotions. Thus, in order to be discriminatory and to capture gradual quality improvement over time, we analyzed CVC insertion as a score.
Our baseline hand hygiene compliance of 48% is similar to the 52% identified by the MOSAR study in 13 European ICUs [28], and to the 40–50% reported by a review summarizing 65 ICU studies [29]. The effects of our intervention are in line with the specific efficacy of the WHO multimodal promotion strategy [30] and other hand hygiene promotion strategies [22]. Hand hygiene improvement was highest for the HHi arm while the average increase of hand hygiene in the CVCi- and COMBi arms was moderate. Together with “HH study fatigue” in one centre, economic constraints resulting in budget and salary cuts, low staffing levels, and high workload were mentioned to play a role in prioritizing CVC-intervention over HH intervention in the COMBi arm. Nurses performed better than doctors across all study arms as has been reported by many others [29].
The average baseline CRBSI incidence density of 2.4/1000 CVC-days as seen in our study has become standard in high-income countries [31–33], although the hospital specific incidence density ranged from 0 to 10.2/1000 at baseline. This range may reflect not only real variation in CVC insertion and infection prevention practice but also differences in culturing quality and frequency. To minimize this bias we discussed these issues with the on-site investigators and study nurses during the kick-off and observer training that took place before baseline measurements began.
Meta-analyses about the effectiveness of CVC bundle or checklist interventions on central line-associated BSI (CLABSI) identified significant reductions (odds ratio of 0.34 [19] and incidence rate ratio 0.45 [18]), but the lowest baseline incidence densities in both meta-analyses were higher (3.4 and 5.7/1000 CVC-days) compared to our study. However, it must be taken into account that CRBSI is a more specific definition than CLABSI [34]. CRBSI decreased already during baseline. This trend may have been the result of external factors, but probably also was a result of the concurrent study, and particularly due to direct observations of CVC insertion and hand hygiene, as shown by increasing CVC insertion scores and HH compliance. However, other aspects of care may have improved as well, e.g. catheter care due to general patient safety awareness. Feedback reports were sent only after the formal start of the intervention, and thus, are barely responsible for the observed ‘surveillance effect’ [35–37]. Alternatively, the improvement of baseline CRBSI rates and CVC insertion scores may also represent a secular trend as reported by the English “Matching Michigan” programme, which was due to pre-existing or ongoing quality improvement initiatives [38]. In contrast, many of our centres had little or no exposure to national quality improvement initiatives and adopted the PROHIBIT project as an opportunity to improve practice [39].
Measuring process indicators allows testing whether the target of an intervention is achieved, provides insight into the implementation process, and allows evaluation of direct association between process parameters and outcome. We report that one percentage point increase in compliance was associated with a two to five percentage point decrease in CRBSI. However, the magnitude of the observed associations must be interpreted with caution, as aggregated data on CVC insertion and hand hygiene compliance had to be used and other factors could be relevant [40–42].
Our study has several strengths. The multicentre design with 14 hospitals from 11 different countries embraces a range of variable IPC practices across Europe, and thus offers greater generalisability than previous studies. The number of CVC-days observed in each centre was large and the combination of a shared baseline and intervention period and the randomized, stepped wedge introduction of the interventions helped to control for unknown trends and confounders. Lastly, the measurement of process indicators demonstrated that CRBSI reduction was the result of improved practice, even if some of this occurred before the formal intervention.
The study has limitations. First, our stepped-wedge design did not allow block randomization based on baseline rates. As a consequence, and unfortunately, the CVCi arm had four out of the five hospitals with low baseline incidence densities. The small effect of the prevention program on CRBSI in the CVCi arm, that was significant in the before-and-after analysis but not significant when considering the decreasing trend already observed during baseline, could well be due to the low baseline rate (1.4/1000 CVC-days), which may be partly explained by the overrepresentation of cardiothoracic surgery patients undergoing elective CVC insertions in this study arm. Second, process indicators not only improved in allocated arms, but in all study arms (HH in the CVCi arm; CVC insertion score in the HHi arm). The PROHIBIT project was a priority or the only ongoing patient safety project in many of our centers. Such project prioritization, together with Hawthorne effects [43] due to the surveillance of process indicators, may have contributed to this finding. Third, some patient- and CVC characteristics differed between baseline and intervention, and between the study arms. Although significance of many differences are due to large numbers, cardiothoracic patients, and hence scheduled surgical admissions, were more frequent in the CVCi arm. While we could not adjust for severity-of-illness score for the entire study population due to missing data, all other critical variables were taken into account in the multivariable models. The analysis on the subset where Apache II scores were reported showed comparable results (Supp.Methods and results). Fourth, although the study duration was 30 months in total, we did not go back to the hospitals to test for sustainability. Others have shown sustainable effects of behavioural change studies aiming at CLABSI prevention [44].
In conclusion, this study demonstrates that multimodal prevention strategies aiming at improving CVC insertion practice and hand hygiene compliance reduce CRBSI in culturally diverse European ICUs. The CVC insertion score explained the reduction of CRBSI and helped to explain the dynamics of behaviour change. Future quality improvement studies should encourage measuring process indicators.
References
ECDC (2013) Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals. European Centre for Disease Prevention and Control, Stockholm
Zingg W, Hopkins S, Gayet-Ageron A, Holmes A, Sharland M, Suetens C, for the ECDC PPS group (2017) Health-care-associated infections in neonates, children, and adolescents: an analysis of paediatric data from the European Centre for Disease Prevention and Control point-prevalence survey. Lancet Infect Dis 17:381–389
Hansen S, Schwab F, Behnke M, Carsauw H, Heczko P, Klavs I, Lyytikainen O, Palomar M, Riesenfeld Orn I, Savey A, Szilagyi E, Valinteliene R, Fabry J, Gastmeier P (2009) National influences on catheter-associated bloodstream infection rates: practices among national surveillance networks participating in the European HELICS project. J Hosp Infect 71:66–73
Hansen S, Schwab F, Gastmeier P, on behalf of the PROHIBIT study group (2015) Provision and consumption of alcohol-based hand rubs in European hospitals. Clin Microbiol Infect 21:1047–1051
Hansen S, Zingg W, Ahmad R, Kyratsis Y, Behnke M, Schwab F, Pittet D, Gastmeier P, on behalf of the PROHIBIT study group (2015) Organization of infection control in European hospitals. J Hosp Infect 91:338–345
Martin M, Zingg W, Hansen S, Gastmeier P, Wu AW, Pittet D, Dettenkofer M, on behalf of the PROHIBIT study group (2013) Public reporting of healthcare-associated infection data in Europe. What are the views of infection prevention opinion leaders? J Hosp Infect 83:94–98
Martin M, Zingg W, Knoll E, Wilson C, Dettenkofer M, on behalf of the PROHIBIT study group (2014) National European guidelines for the prevention of Clostridium difficile infection: a systematic qualitative review. J Hosp Infect 87:212–219
van der Kooi T, Wolkewitz M, van Benthem B, de Greeff S, Grundmann H, Zingg W, on behalf of the PROHIBIT study group (2013) Prohibit (Preventing hospital-acquired infections by intervention and training): preliminary results of a European multi-center study on the effectiveness of a hand hygiene campaign and a central venous catheter bundle (abstract O83). In: International conference of prevention and infection control (ICPIC), Geneva
van der Kooi T, Wolkewitz M, van Benthem B, de Greeff S, Grundmann H, Zingg W, on behalf of the PROHIBIT study group (2014) Unusual distribution of pathogens in a European multi-centre study about central venous catheter-related bloodstream infections (Abstract P0519). In: European congress of clinical microbiology and infectious diseases (ECCMID), Barcelona
van der Kooi T, Wolkewitz M, van Benthem B, de Greeff S, Grundmann H, Zingg W, on behalf of the PROHIBIT study group (2014) The PROHIBIT (Preventing hospital-acquired infections by intervention and training) intervention tria—results of a cluster-randomized European multi-center study on the reduction of central-line related bloodstream infections (Abstract O198). In: European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), Barcelona
Zingg W, Cartier V, Inan C, Touveneau S, Theriault M, Gayet-Ageron A, Clergue F, Pittet D, Walder B (2014) Hospital-wide multidisciplinary, multimodal intervention programme to reduce central venous catheter-associated bloodstream infection. PLoS ONE 9:e93898
Pittet D, Allegranzi B, Storr J (2008) The WHO Clean Care is Safer Care programme: field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health 1:4–10
ECDC (2010) European surveillance of healthcare-associated infections in intensive care units—HAI-Net ICU protocol, version 1.01. European Centre for Disease Prevention and Control, Stockholm
Sax H, Allegranzi B, Chraiti MN, Boyce J, Larson E, Pittet D (2009) The World Health Organization hand hygiene observation method. Am J Infect Control 37:827–834
Eggimann P, Harbarth S, Constantin MN, Touveneau S, Chevrolet JC, Pittet D (2000) Impact of a prevention strategy targeted at vascular-access care on incidence of infections acquired in intensive care. Lancet 355:1864–1868
Wolkewitz M, Cooper BS, Bonten MJ, Barnett AG, Schumacher M (2014) Interpreting and comparing risks in the presence of competing events. BMJ 349:g5060
Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, Perneger TV (2000) Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet 356:1307–1312
Ista E, van der Hoven B, Kornelisse RF, van der Starre C, Vos MC, Boersma E, Helder OK (2016) Effectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis 16:724–734
Blot K, Bergs J, Vogelaers D, Blot S, Vandijck D (2014) Prevention of central line-associated bloodstream infections through quality improvement interventions: a systematic review and meta-analysis. Clin Infect Dis 59:96–105
Scales DC, Dainty K, Hales B, Pinto R, Fowler RA, Adhikari NK, Zwarenstein M (2011) A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA 305:363–372
Burrell AR, McLaws ML, Murgo M, Calabria E, Pantle AC, Herkes R (2011) Aseptic insertion of central venous lines to reduce bacteraemia. The Central Line Associated Bacteraemia in, N. S. W. Intensive Care Units Collaborative. Med J Aust 194:583–587
Schweizer ML, Reisinger HS, Ohl M, Formanek MB, Blevins A, Ward MA, Perencevich EN (2014) Searching for an optimal hand hygiene bundle: a meta-analysis. Clin Infect Dis 58:248–259
Jeong IS, Park SM, Lee JM, Song JY, Lee SJ (2013) Effect of central line bundle on central line-associated bloodstream infections in intensive care units. Am J Infect Control 41:710–716
Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC (2014) The impact of central line insertion bundle on central line-associated bloodstream infection. BMC Infect Dis 14:356
Bonello RS, Fletcher CE, Becker WK, Clutter KL, Arjes SL, Cook JJ, Petzel RA (2008) An intensive care unit quality improvement collaborative in nine Department of Veterans Affairs hospitals: reducing ventilator-associated pneumonia and catheter-related bloodstream infection rates. Jt Comm J Qual Patient Saf 34:639–645
Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJ, Lloyd SM, Lang C (2011) Elimination of central-venous-catheter-related bloodstream infections from the intensive care unit. BMJ Qual Saf 20:174–180
McLaws ML, Burrell AR (2012) Zero risk for central line-associated bloodstream infection: are we there yet? Crit Care Med 40:388–393
Derde LP, Cooper BS, Goossens H, Malhotra-Kumar S, Willems RJ, Gniadkowski M, Hryniewicz W, Empel J, Dautzenberg MJ, Annane D, Aragao I, Chalfine A, Dumpis U, Esteves F, Giamarellou H, Muzlovic I, Nardi G, Petrikkos GL, Tomic V, Marti AT, Stammet P, Brun-Buisson C, Bonten MJ, Team MWS (2014) Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: an interrupted time series study and cluster randomised trial. Lancet Infect Dis 14:31–39
Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, van Beeck EF (2010) Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol 31:283–294
Allegranzi B, Gayet-Ageron A, Damani N, Bengaly L, McLaws ML, Moro ML, Memish Z, Urroz O, Richet H, Storr J, Donaldson L, Pittet D (2013) Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis 13:843–851
ECDC (2012) Annual epidemiological report. Reporting on 2010 surveillance data and 2011 epidemic intelligence data. European Centre for Disease Prevention and Control, Stockholm
Dudeck MA, Horan TC, Peterson KD, Allen-Bridson K, Morrell G, Anttila A, Pollock DA, Edwards JR (2013) National Healthcare Safety Network report, data summary for 2011, device-associated module. Am J Infect Control 41:286–300
Rosenthal VD, Maki DG, Mehta Y, Leblebicioglu H, Memish ZA, Al-Mousa HH, Balkhy H, Hu B, Alvarez-Moreno C, Medeiros EA, Apisarnthanarak A, Raka L, Cuellar LE, Ahmed A, Navoa-Ng JA, El-Kholy AA, Kanj SS, Bat-Erdene I, Duszynska W, Van Truong N, Pazmino LN, See-Lum LC, Fernandez-Hidalgo R, Di-Silvestre G, Zand F, Hlinkova S, Belskiy V, Al-Rahma H, Luque-Torres MT, Bayraktar N, Mitrev Z, Gurskis V, Fisher D, Abu-Khader IB, Berechid K, Rodriguez-Sanchez A, Horhat FG, Requejo-Pino O, Hadjieva N, Ben-Jaballah N, Garcia-Mayorca E, Kushner-Davalos L, Pasic S, Pedrozo-Ortiz LE, Apostolopoulou E, Mejia N, Gamar-Elanbya MO, Jayatilleke K, de Lourdes-Duenas M, Aguirre-Avalos G, International Nosocomial Infection Control C (2014) International Nosocomial Infection Control Consortium (INICC) report, data summary of 43 countries for 2007–2012. Device-associated module. Am J Infect Control 42:942–956
Centers for Disease Control and Prevention (CDC)/National Healthcare Safety Network (NHSN) (2017) https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf. Accessed 6 Dec 2017
Mannien J, van den Hof S, Muilwijk J, van den Broek PJ, van Benthem B, Wille JC (2008) Trends in the incidence of surgical site infection in the Netherlands. Infect Control Hosp Epidemiol 29:1132–1138
Zuschneid I, Schwab F, Geffers C, Ruden H, Gastmeier P (2003) Reducing central venous catheter-associated primary bloodstream infections in intensive care units is possible: data from the German nosocomial infection surveillance system. Infect Control Hosp Epidemiol 24:501–505
Almirante B, Limon E, Freixas N, Gudiol F, Program V (2012) Laboratory-based surveillance of hospital-acquired catheter-related bloodstream infections in Catalonia Results of the VINCat Program (2007–2010). Enferm Infecc Microbiol Clin 30(Suppl 3):13–19
Bion J, Richardson A, Hibbert P, Beer J, Abrusci T, McCutcheon M, Cassidy J, Eddleston J, Gunning K, Bellingan G, Patten M, Harrison D, Matching Michigan C, Writing C (2013) ‘Matching Michigan’: a 2-year stepped interventional programme to minimise central venous catheter-blood stream infections in intensive care units in England. BMJ Qual Saf 22:110–123
Dixon-Woods M, Leslie M, Tarrant C, Bion J (2013) Explaining Matching Michigan: an ethnographic study of a patient safety program. Implement Sci 8:70
Beggs CB, Shepherd SJ, Kerr KG (2008) Increasing the frequency of hand washing by healthcare workers does not lead to commensurate reductions in staphylococcal infection in a hospital ward. BMC Infect Dis 8:114
Nicolau DV Jr, Kith G, Oshmyansky A (2010) Evidence for a simple linear relationship between MRSA rates and hand-washing compliance. J Hosp Infect 75:140–141
Wang J, Wang L, Magal P, Wang Y, Zhuo J, Lu X, Ruan S (2011) Modelling the transmission dynamics of meticillin-resistant Staphylococcus aureus in Beijing Tongren hospital. J Hosp Infect 79:302–308
Srigley JA, Furness CD, Baker GR, Gardam M (2014) Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study. BMJ Qual Saf 23:974–980
Pronovost PJ, Goeschel CA, Colantuoni E, Watson S, Lubomski LH, Berenholtz SM, Thompson DA, Sinopoli DJ, Cosgrove S, Sexton JB, Marsteller JA, Hyzy RC, Welsh R, Posa P, Schumacher K, Needham D (2010) Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ 340:c309
Acknowledgements
We thank Sylvie Touveneau, Marie-Noëlle Chraïti and Benedetta Allegranzi, who devoted themselves to the training of the on-site investigators and study nurses in the workshops, both at the University Medical Center Groningen and the HUG. We thank Lauren Clack for editing. Our gratitude extends also to the participating centres for collaborating in this study, especially the on-site investigators and study nurses, physicians, (auxiliary) nurses and other healthcare professionals that responded positively to the challenge to improve their hand hygiene and CVC insertion practices and thus contributed to the increased safety of the patients in their care. Martin Wolkewitz has been funded by the German Research Foundation (Deutsche Forschungsgemeinschaft; Grant No WO 1746/1-1).
PROHIBIT Consortium: PROHIBIT Study Group: Pittet D (principaI investigator), Zingg W (coordinator), Ahmad R, Allegranzi B, Cookson B, Dettenkofer M, Gastmeier P, Grundmann H, Hansen S, Heczko PB, Holmes A, Kyratsis Y, Magiorakos A, Martin M, Richet H, Sax H, Szilágyi E, van Benthem B, van der Kooi T, Wu AW.
Author information
Authors and Affiliations
Consortia
Contributions
DP, HG, AW, WZ and HS conceived the study. HG, WZ, HS, BB and TK further designed the study and developed the study protocol. BW, LC and VC trained the on-site investigators and study nurses. ME, AB, KL, MPM, OP, MP, ES, TW, SF, AR, UD, PS, MZ, CG and TL were responsible for the local study coordination, data collection and implementation of the interventions. TK was responsible for random allocation of interventions to hospitals, data management and, together with MW, SH, JK and HB, for statistical analyses. TK and WZ wrote the initial draft of the manuscript, with contributions of HS, HG, JD, and LC, which was revised and approved by all authors. The guarantor is TK.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no interests to disclose.
Data sharing
The data are stored with the RIVM. Applications to use the data for further research can be sent to Dr. Walter Zingg (e-mail, Walter.Zingg@hcuge.ch).
Additional information
Hajo Grundmann and Walter Zingg contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
van der Kooi, T., Sax, H., Pittet, D. et al. Prevention of hospital infections by intervention and training (PROHIBIT): results of a pan-European cluster-randomized multicentre study to reduce central venous catheter-related bloodstream infections. Intensive Care Med 44, 48–60 (2018). https://doi.org/10.1007/s00134-017-5007-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-5007-6