Abstract
Objective
To demonstrate that among patients with acute respiratory distress syndrome (ARDS), the presence of diffuse alveolar damage (DAD) at histological examination, as compared to its absence, defines a specific subphenotype.
Methods
We studied 149 patients who died in our ICU with the clinical diagnosis of ARDS according to the Berlin Definition (BD) and who had autopsy examination. We compared the change over time of different clinical variables in patients with (n = 49) and without (n = 100) DAD. A predictive model for the presence of DAD was developed and validated in an independent cohort of 57 patients with ARDS and postmortem examination (21 of them with DAD).
Results
Patients with DAD, as compared to patients without DAD, had a lower PaO2/FiO2 ratio and dynamic respiratory system compliance, and a higher SOFA score and INR, and were more likely to die of hypoxemia and less likely to die of shock. In multivariate analysis, variables associated with DAD [odds ratio, 95 % confidence interval (CI)] were PaO2/FiO2 ratio [0.988 (0.981–0.995)], dynamic respiratory system compliance [0.937 (0.892–0.984)] and age [0.972 (0.946–0.999)]. Areas under the ROC curve (95 % CI) for the classification of DAD using the regression model or the BD were, respectively, 0.74 (0.65–0.82) and 0.64 (0.55–0.72) (p = 0.03). In the validation cohort, the areas under the ROC curve for the diagnosis of DAD were 0.73 (0.56–0.90) and 0.67 (0.54–0.81) for the regression model and the BD, respectively.
Conclusions
The presence of DAD appears to define a specific subphenotype in patients with ARDS. Targeting patients with DAD within the population of patients with the clinical diagnosis of ARDS might be appropriate to find effective therapies for this condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The acute respiratory distress syndrome (ARDS) is a common syndrome in critical care [1], associated with increased use of resources and a high mortality rate, greater than 50 % [2]. Diffuse alveolar damage (DAD), characterized by lung edema, inflammation, hyaline membranes and alveolar hemorrhage is considered to be the pathologic hallmark of ARDS [3–7]. However, DAD is present in only about half of the patients diagnosed clinically as having ARDS [3, 8–18].
Pathological findings other than DAD in patients with ARDS include conditions such as pneumonia, alveolar hemorrhage, cardiogenic pulmonary edema, pulmonary embolism, metastatic malignancies, pulmonary lymphoma, eosinophilic pneumonia, fibrosis, bronchiolitis obliterans, organizing pneumonia or drug reactions [8, 16, 19]. These conditions are not likely to share the same pathogenesis, pathophysiology, and pharmacologic treatment.
Indeed, the failure of investigators to find biomarkers or effective pharmacologic treatments of ARDS [20, 21] may be due, in part, to the fact that the syndrome includes a heterogeneous group of pathological diagnoses [22, 23]. Thus, it has been proposed that the identification of homogeneous populations of patients within the clinical diagnosis of ARDS may have implications for the design of clinical trials and the discovery of diagnostic and prognostic biomarkers [18]. For instance, the prediction of the subset of patients with clinical criteria for ARDS that have DAD may allow the inclusion of more homogeneous population of patients in therapeutic studies, thus increasing the probability of finding effective therapies.
However, it is unknown whether the presence of DAD at histological examination defines a specific subgroup of patients within ARDS. We hypothesized in the present study that, in patients with the clinical diagnosis of ARDS, the clinical characteristics and clinical course differ in patients with DAD and in patients without DAD.
Patients and methods
Patients
For the derivation cohort, we included in the present study all patients who died in the ICU of our institution from 2000 to 2012. For the validation cohort, we included patients dying in our institution in 2013 and 2014, as well as patients from two other institutions (Universidad del Bosque, Bogotá, Colombia, and Federal University of Juiz de Fora, Brasil) recruited since 2005. All patients had the clinical diagnosis of ARDS at the time of death and had autopsy examination. Exclusion criteria were: ICU length of stay less than 12 h; clinical diagnosis of heart failure; clinical diagnosis of pulmonary fibrosis; patients never intubated; organ donors; patients with legally mandated autopsies; and patients with missing data. As the relationship between clinical and histological findings may be lost as the time from diagnosis to death increases, we also excluded patients in whom death occurred more than 14 days after the diagnosis of ARDS.
All charts were retrospectively reviewed to determine whether patients met the clinical criteria for the diagnosis of ARDS at the moment of their demise. The diagnosis of ARDS was established by consensus of three intensivists (F.F., A.T. and P.C.) and discrepancies were resolved by assessment of other two intensivists (J.A.L. and A.E.). The diagnosis of ARDS was made according to the Berlin definition (BD) [24].
Study day 0 was the first day the patient met the criteria for the diagnosis of ARDS, considering the worst gas exchange that day and the worst chest X-ray taken within ±24 h. Demographic and clinical variables from day 0 to death were recorded. SAPS II was calculated at ICU admission and also at day 0, using the worst values [25]. Peak inspiratory pressure (PIP), positive end-expiratory pressure (PEEP) and tidal volume (V T) at 0800 hours each day were registered. Dynamic compliance of the respiratory system (C DYN) was calculated as V T/(PIP − PEEP).
Patients were considered to have a pulmonary risk factor for ARDS if they had the diagnosis of pneumonia, aspiration of gastric contents, inhalation injury or lung contusion, and an extra-pulmonary risk factor for ARDS if they had the diagnosis of non-pulmonary sepsis or septic shock, multiple blood transfusion or pancreatitis.
The cause of death was determined according to the following criteria: refractory shock, if systolic blood pressure was <90 mm Hg during the 6 h prior to death; refractory hypoxemia, if oxygen saturation was persistently below 85 % during the 6 h prior to death; refractory shock and hypoxemia if the two causes as defined coexisted; and other causes of death.
Informed consent to perform the autopsy and to use tissue samples for research or teaching purposes was always requested from patients’ relatives. Patients from 2000 to 2010 belong to a database previously used [3, 8, 15]. New not yet available information required for the present analysis was retrieved from those patients charts as well as for patients admitted after 2010 (IRB evaluation 12/14).
Pathological criteria for the diagnosis of DAD
Postmortem study was performed within 12 h of death. After removal from the thorax, the lungs were inflated with 10 % formalin to a pressure of 35 cm H2O and fixed en bloc with 10 % formalin. After fixation, the lungs were cut into 3-cm-thick slices. We took samples for microscopic analysis from each pulmonary lobe and additional samples from areas with macroscopic injuries. Two pathologists (A.B.B. and J.M.R.), blind as to the clinical diagnosis, independently analyzed each sample and discrepancies were resolved by consensus. As in previous studies [3, 8, 11, 13–15], criteria for the diagnosis of DAD included the presence of hyaline membranes plus at least one of the following: intra-alveolar edema, alveolar type II cell proliferation covering the denuded alveolocapillary membrane, interstitial proliferation of fibroblasts and myofibroblasts, or organizing interstitial fibrosis. The presence of hyaline membranes was qualitatively assessed (present or absent). Pneumonia without DAD required the presence of intense neutrophilic infiltration in the interstitium and in the intra-alveolar spaces, particularly around terminal bronchioles, and no hyaline membranes in any of the lung sections. Patients with DAD and pneumonia were included in the DAD group, as previously practised [3, 8, 15].
Statistical analysis
In patients with the clinical diagnosis of ARDS, we compared clinical and demographic variables present at day 0 between patients with DAD and patients without DAD, using the chi-square test and the Wilcoxon rank-sum test for proportions and quantitative data, respectively. The change over time of different clinical and laboratory variables was compared between the group with DAD and the group without DAD. The change over time of variables was modeled using locally weighted scatterplot smoothing (LOWESS) which is a non-parametric regression method that combines multiple regression models in a k-nearest-neighbor-based meta-model with the aim of modeling complex processes for which no theoretical models exists. This method provides an estimated mean of variables over time for each group without a measurement of the dispersion of the data. Generalized estimating equations (GEE) were used to compare the time course of variables over time in the different groups. GEE is robust enough to deal with modest departures from normality, as was the case of our data.
As most patients died in the first days after ARDS diagnosis, and fewer variables were available for analysis at later points in time, we chose to analyze only variables from day 0 to day 7 of ARDS diagnosis.
The clinical profile of patients with bilateral pneumonia without DAD may resemble that of patients with DAD. Thus, we compared patients with the histological diagnosis of pneumonia with patients with DAD, both by univariate analysis (by the chi-square test and the Wilcoxon rank sum test, for proportions and quantitative data, respectively) of variables present at day 0, and by LOWESS modeling of the time course of physiological variables and GEE analysis.
A predictive model of DAD was built in patients with the clinical diagnosis of ARDS. We used predictive multivariate logistic regression analysis. The maximal model contained all variables associated to the diagnosis of DAD on day 0 with a p value <0.10 in univariate analysis. The strength of the association was measured as the odds ratio (OR) and the 95 % confidence interval (CI). The area under the receiver operating characteristic curve (AURC) was used to measure the accuracy to predict DAD. The AURC for the predictive model and for the BD were compared by the DeLong test. The model was validated in a second cohort of patients dying with the diagnosis of ARDS (n = 21 with DAD; n = 36 without DAD), by calculating the AURC of the derived model to predict the presence of DAD in these patients.
Data were expressed as median and interquartile range. A p value <0.05 was considered statistically significant. All analyses were performed in the R package.
Results
Clinical features
We screened the clinical records of 434 patients who died in our ICU from 2000 to 2012 and received autopsy examination (Fig. S1). Of them, 149 met clinical criteria for the diagnosis of ARDS at the time of death and were diagnosed within 14 days prior to death. Histological changes in the 149 patients with ARDS were: DAD in 49, pneumonia in 45, not identified histological lesion in 23, cancer in 8, alveolar hemorrhage in 7, pulmonary embolism in 9, fibrosis in 3 and other diagnoses in 5.
Most patients died within the first days after the clinical diagnosis of ARDS (Fig. 1). Most common risk factors included shock, extra-pulmonary sepsis and pneumonia (Table S1). All patients were receiving PEEP ≥5 cm H2O when diagnosed of ARDS.
Patients with DAD were younger and presented a significantly higher proportion of chronic alcohol abuse than patients without DAD (Table 1; Table S1). There was a trend (p = 0.05) to a lower proportion of patients with extra-pulmonary sepsis in patients with DAD as compared to patients without DAD.
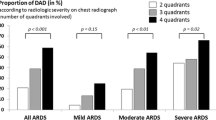
The relative proportion of patients with DAD increased according to ARDS severity at day 0 [5 of 38 (13.2 %), 25 of 75 (33.3 %) and 19 of 36 (52.8 %), for mild, moderate and severe ARDS, respectively]. Patients with DAD did not have ARDS for a longer period of time than patients without DAD (Table 1).
In the comparison of patients with histological pneumonia without DAD and patients with DAD, patients with DAD were also younger and DAD was associated with a greater ARDS severity (Tables S2, S3).
Physiological variables at day 0
At the time of the diagnosis of ARDS, PaO2/FiO2 ratio, PIP, the difference between PIP and PEEP, and C DYN differed between patients with DAD and patients without DAD, whereas variables related with organ failure did not (Table 1; Table S1).
Similar findings emerged in the comparison between patients with pneumonia and patients with DAD. Specifically, at the time of the diagnosis of ARDS, PaO2/FiO2 ratio, PIP, and the difference between PIP and PEEP differed in patients with DAD and patients with pneumonia (Tables S2, S3).
Physiological variables from the day 0 to day 7
During the ICU stay, PIP, the difference between PIP and PEEP, C DYN, and total SOFA score differed in patients with DAD versus patients without DAD (p < 0.05 for the comparison DAD versus non-DAD) (Figs. 2, 3). The time course (interaction effect of time × group) of PaO2/FiO2 ratio, PEEP and INR was different in patients without DAD as compared to patients with DAD.
Time course of respiratory variables in patients with (green) and without (blue) DAD. PaO 2/FiO 2 ratio between arterial partial pressure of oxygen and inspiratory oxygen fraction, PIP peak inspiratory airway pressure, PEEP positive end expiratory pressure, C DYN dynamic compliance of the respiratory system (ml/cmH2O). *p < 0.05 for the effect of time; † p < 0.05 for the effect of group (DAD vs. non-DAD); ¶ p < 0.05 for the interaction time × group
Time course of non-respiratory variables in patients with (green) and without (blue) DAD. SOFA sequential organ failure assessment, INR international normalized ratio, CRP C-reactive protein. *p < 0.05 for the effect of time; † p < 0.05 for the effect of group (DAD vs. non-DAD); ¶ p < 0.05 for the interaction time × group
Likewise, patients with pneumonia differed from patients with DAD in their PaO2/FiO2 ratio, PIP, difference between PIP and PEEP, and SOFA score (p < 0.05 for the comparison DAD versus pneumonia without DAD). The time course (interaction effect of time × group) of PIP, C DYN and INR was also different between patients with DAD and patients with pneumonia (Fig. 4; Fig. S2).
Time course of selected respiratory and non-respiratory variables in patients with DAD (green) and patients with pneumonia (without DAD) (blue). PaO 2/FiO 2 ratio between arterial partial pressure of oxygen and inspiratory oxygen fraction, PIP peak inspiratory airway pressure, PEEP positive end expiratory pressure, C DYN dynamic compliance of the respiratory system (ml/cmH2O), SOFA sequential organ failure assessment. *p < 0.05 for the effect of time; † p < 0.05 for the effect of group (DAD vs. non-DAD); ¶ p < 0.05 for the interaction time × group
Other features
Causes of death were different in patients with and without DAD (Table 1). Patients with DAD were about five times as likely to die of hypoxemia than patients without DAD, whereas patients without DAD were about twice as likely to die of shock than patients with DAD. The same pattern (not reaching statistical significance) was observed in patients with DAD as compared to patients with pneumonia (Table S2).
Drugs received prior to hospital admission (Tables S1, S3) or during their ICU course (Tables S4, S5), and tidal volumes prescribed during the ICU course (Fig. 1; Fig. S2) did not differ between the different groups.
Predictive model for DAD
The maximal multivariate model included the following variables present at the time of the clinical diagnosis of ARDS: age, diagnosis of clinical pneumonia, extra-pulmonary sepsis, alcohol abuse, PaO2/FiO2 ratio, C DYN and serum creatinine concentration on day 0. The final regression model included (OR, and 95 % CI and p value) the PaO2/FiO2 ratio [0.988 (0.981–0.995), p < 0.01], C DYN [0.937 (0.892–0.984, p < 0.01] and age [0.972 (0.946–0.999), p < 0.01]. Characteristics of this model (95 % CI) were: sensitivity 0.45 (0.31–0.59); specificity 0.82 (0.74–0.90); positive predictive value 0.55 (0.40–0.70); negative predictive value 0.75 (0.67–0.83); positive likelihood ratio 2.49 (1.48–4.20) and negative likelihood ratio 0.67 (0.51–0.88).
The AURC (95 % CI) for the prediction of DAD was significantly greater for the regression model than for the Berlin Definition [0.74 (0.65–0.82) vs. 0.64 (0.55–0.72)], respectively (p = 0.03) (Fig. 5). In the validation cohort (n = 21 with DAD, n = 36 without DAD) the area under the ROC curve was 0.73 (0.56 − 0.90) for the logistic regression model and 0.67 (0.54–0.81) for the BD (Fig. 5).
Receiver operating characteristic (ROC) curve of the Berlin definition classification (green) and the predictive model (blue) for the presence of DAD at histological examination in patients with the clinical diagnosis of ARDS in the derivation (lefthand graph) and validation (righthand graph) cohorts. The areas under the ROC curve in the derivation cohort were significantly different (p = 0.03). Values indicate area under the ROC curve and the 95 % confidence interval
Representative histological findings in 2 cases of DAD are shown in Fig. S3.
Discussion
We report for the first time in ARDS non-survivors different clinical characteristics depending on the underlying histology. These findings provide support to the concept that the presence of DAD defines a specific subphenotype within patients with the clinical diagnosis of ARDS.
The present results, showing differences also when patients with DAD were compared to patients with pneumonia (without DAD), at least in fatal cases, do not support the proposal that morphological changes other than DAD (e.g., pneumonia) can be included as the histological correlate of ARDS [18]. The results of previous studies on risk factors, pathogenesis, biomarkers and treatments of ARDS should be interpreted with caution considering that different clinical entities were almost certainly included in these studies.
Of note, the only effective therapies for ARDS are lung protective ventilation strategies such as lower volume and pressures ventilation, prone ventilation, and cisatracurium, the latter presumably for additional lung protection [26–28]. It is possible that these interventions may be effective for patients with many types of acute lung injury in addition to DAD. However, no pharmacological therapy has been proven to be of benefit for ARDS [20, 21]. If such therapy targeting DAD per se is to succeed, enrichment strategies are needed by the identification of patients with specific clinico-pathological manifestations.
The concept that ARDS contains different subphenotypes is further supported by a recent study by Calfee et al. [29]. Using latent class analysis and two large cohorts of ARDS patients, [28, 30] several variables were found to identify two distinct subphenotypes. Our study differs in that we sought to determine whether patients with a pre-specified variable (i.e., the presence of DAD at histological examination) have a particular clinical subphenotype. Notwithstanding the different methodology, we also found differences in age, PaO2/FiO2 ratio and airway pressure between the two clinical subphenotypes identified.
Our results are very much in line with two recent studies in patients with ARDS undergoing open lung biopsy (OLB) [16, 17]. Guerin et al. [16] reported, in a selected population of 83 patients with ARDS undergoing OLB because of non-resolving ARDS, that patients with DAD had a lower PaO2/FiO2 ratio, higher airway plateau pressure and (non-significantly) higher mortality rate. Similarly, Kao et al. [17] found in 101 ARDS patients undergoing OLB that DAD was associated in multivariate analysis with a higher mortality rate.
The clinical profile of DAD herein reported is defined by limited clinical variables (age, respiratory system compliance, PaO2/FiO2 ratio). Variables used to compare different groups vary over time and it is hard to use them to differentiate different groups of patients. Even in the context of this difficulty, studies using this approach (i.e., measuring certain physiological variables at particular points in time) have been useful to characterize differences between groups of patients [3, 8, 15–17, 29]. Despite these limitations and the constraints imposed by the current design, which precludes the use of other more sophisticated variables, we found significant differences in some variables, probably revealing different pathogenesis of DAD as the underlying histological finding of ARDS versus other pathological findings, seemingly including pneumonia. We propose that our results, in combination with the results of other studies [16, 17], suggest that ARDS associated with DAD defines a specific subphenotype distinct from ARDS associated with other pathological findings. Nevertheless, despite the strength of the present analysis and the significance of the differences found in age, gas exchange and mechanical properties of the respiratory system, it has to be acknowledged that the prediction model is of limited clinical usefulness for the detection of patients with DAD. Of particular interest, given the finding of higher airway pressures in patients with DAD as compared to patients without DAD [16], is the speculation of mechanical ventilation as a contributing cause for DAD.
It is possible that our model, built to predict the presence of DAD, is not more accurate for this prediction than the BD, the currently used method for the diagnosis of ARDS. Thus, we compared our model with the BD as to their accuracy to predict the presence of DAD. The analysis showed a low AURC for the BD, as is expected since the BD is not meant to predict DAD. The AURC for our model was also low, but significantly higher than that for the BD, suggesting that additional diagnostic tools are needed for the identification of DAD in patients. The model predictive of DAD was validated in an independent cohort of ARDS patients. Management details in the derivation cohort, both prior to and after the diagnosis of ARDS, did not differ in patients with and without DAD. Unfortunately, management details in the validation cohort are lacking.
As in previous studies, we used a retrospective approach for patient identification [3, 8, 15]. This may have led to over-diagnosis of ARDS, as there is evidence that ARDS may be unrecognized clinically [31]. The inclusion of only those clinically recognized, and probably the more severe cases and therefore more likely to have DAD, might likely have exaggerated the differences reported here.
This study has several limitations. First, we studied only autopsy cases, and therefore the reported findings may only reflect the extreme of the disease severity spectrum and may only apply to non-survivors. Second, while all x-rays met the BD definition, we did not examine more nuanced interpretations given concern for reliability [32]. Third, it can be argued that the differences found between patients with and without DAD solely reflect differences in severity or in the duration of the time course of the disease, and that both entities (ARDS with DAD and ARDS without DAD) are not really different but the same condition. The lack of differences in the SAPSII score or in the SOFA score at the time of ARDS diagnosis argues against a different clinical severity as a potential explanation for the differences observed in patients with and without DAD. In addition, the comparable length of ICU stay before the clinical diagnosis of ARDS does not support that patients with and without DAD have different disease duration before death. Fourth, our autopsy design precludes the use of mortality as one of the outcome measures to assess predictive validity. Fifth, the lack of information on plateau pressure impedes the correct calculation of static compliance which is, rather than peak airway pressure (which depends on inspiratory air flow and on airway resistance) and its related variable dynamic compliance, the variable of interest to relate to the development of DAD. This and the paucity of information to calculate tidal volume according to ideal body weight are limitations shared by other studies [3, 8] that need to be pointed out. Sixth, the sample size limits other interesting group comparisons, such as the comparison between patients with DAD (without pneumonia), patients with pneumonia (without DAD) and patients with both DAD and pneumonia. However, we propose that the main question of the present study (are there clinical differences in patients with ARDS if the histological examination shows DAD versus other findings?) is directly answered by the current design.
Some of the strengths of this study include the relatively large sample size, the inclusion of only patients with the clinical diagnosis of ARDS at the time of death, the inclusion of patients within 14 days of initial diagnosis (to strengthen the hypothesis of a potential relationship between the clinical and the histological findings), and rigorous pathology methods.
In conclusion, patients with ARDS and DAD at post-mortem have a different clinical phenotype than patients with ARDS and other histologic findings without DAD. Our findings suggest that, within the broader population of patients that fulfill ARDS criteria, a subgroup that is more likely to have DAD can be identified. This patient subset may fit into a distinct clinico-pathological entity, but additional studies in ARDS survivors, prospectively collecting a much broader dataset, would be needed to confirm this contention.
References
Villar J, Blanco J, Manuel Añón J et al (2011) The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med 37:1932–1941
Zambon M, Vincent JL (2008) Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest 133:1120–1127
Thille AW, Esteban A, Fernandez-Segoviano P et al (2013) Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med 187:761–767
Mukhopadhyay S, Parambil JG (2012) Acute interstitial pneumonia (AIP): relationship to Hamman-Rich syndrome, diffuse alveolar damage (DAD), and acute respiratory distress syndrome (ARDS). Semin Respir Crit Care Med 233:476–485
American Thoracic S, European Respiratory S. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias (2002) This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med 165:277–304
Katzenstein AL, Bloor CM, Leibow AA (1976) Diffuse alveolar damage–the role of oxygen, shock, and related factors. A review. Am J Pathol 85:209–228
Ashbaugh DG, Bigelow DB, Petty TL, Levine BE (1967) Acute respiratory distress in adults. Lancet 2:319–323
Esteban A, Fernandez-Segoviano P, Frutos-Vivar F et al (2004) Comparison of clinical criteria for the acute respiratory distress syndrome with autopsy findings. Ann Intern Med 141:440–445
Patel SR, Karmpaliotis D, Ayas NT et al (2004) The role of open-lung biopsy in ARDS. Chest 125:197–202
Kao KC, Tsai YH, Wu YK et al (2006) Open lung biopsy in early-stage acute respiratory distress syndrome. Crit Care 10:R106
Pinheiro BV, Muraoka FS, Assis RV et al (2007) Accuracy of clinical diagnosis of acute respiratory distress syndrome in comparison with autopsy findings. J Brasil Pneumol 33:423–428
de Hemptinne Q, Remmelink M, Brimioulle S et al (2009) ARDS: a clinicopathological confrontation. Chest 135:944–949
Sarmiento X, Almirall J, Guardiola JJ et al (2011) Study on the clinicopathological correlation in the secondary acute respiratory distress syndrome. Med Intensiva 35:22–27
Sarmiento X, Guardiola JJ, Almirall J et al (2011) Discrepancy between clinical criteria for diagnosing acute respiratory distress syndrome secondary to community acquired pneumonia with autopsy findings of diffuse alveolar damage. Resp Med 105:1170–1175
Thille AW, Esteban A, Fernández-Segoviano P et al (2013) Chronology of histological lesions in acute respiratory distress syndrome with diffuse alveolar damage: a prospective cohort study of clinical autopsies. Lancet Respir Med 1:395–401
Guerin C, Bayle F, Leray V, Debord S, Stoian A, Yonis H, Roudaut JB, Bourdin G, Devouassoux-Shisheboran M, Bucher E, Ayzac L, Lantuejoul S, Philipponnet C, Kemeny JL, Souweine B, Richard JC (2015) Open lung biopsy in nonresolving ARDS frequently identifies diffuse alveolar damage regardless of the severity stage and may have implications for patient management. Intensive Care Med 41:222–230
Kao KC, Hu HC, Chang CH, Hung CY, Chiu LC, Li SH, Lin SW, Chuang LP, Wang CW, Li LF, Chen NH, Yang CT, Huang CC, Tsai YH (2015) Diffuse alveolar damage associated mortality in selected acute respiratory distress syndrome patients with open lung biopsy. Crit Care 19:228
Thompson BT, Matthay MA (2013) The Berlin definition of ARDS versus pathological evidence of diffuse alveolar damage. Am J Respir Crit Care Med 187:675–677
Thille AW, Vuylsteke A, Bersten A (2015) Does the Berlin definition for acute respiratory distress syndrome predict the presence of diffuse alveolar damage? Intensive Care Med 41(2):342–344
Binnie A, Tsang JL, dos Santos CC (2014) Biomarkers in acute respiratory distress syndrome. Curr Opin Crit Care. 20:47–55
Tonelli AR, Zein J, Adams J, Ioannidis JP (2014) Effects of interventions on survival in acute respiratory distress syndrome: an umbrella review of 159 published randomized trials and 29 meta-analyses. Intensive Care Med 40:769–787
Cardinal-Fernández P, Ballén-Barragán, Lorente JA (2014) ARDS: a clinical syndrome or a pathological entity? In: VincentJL (ed) Annual update in intensive care and emergency medicine. Springer, Berlin, pp 219–229
Cardinal-Fernández P, Esteban A, Thompson BT, Lorente JA (2015) ARDS: lessons learned from the heart. Chest 147:7–8
Definition Task Force ARDS, Ranieri VM, Rubenfeld GD, Thompson BT et al (2012) Acute respiratory distress syndrome: the Berlin definition. JAMA 307:2526–2533
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Guerin C, Reignier J, Richard JC et al (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368:2159–2168
Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guérin C, Prat G, Morange S, Roch A, ACURASYS Study Investigators (2010) Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 363:1107–1116
Network The Acute Respiratory Distress Syndrome (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Calfee CS, Delucchi K, Parsons PE, the NHLBI ARDS Network (2014) Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med 2:611–620
Network The Acute Respiratory Distress Syndrome (2004) Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 351:327–336
Ferguson ND, Frutos-Vivar F, Esteban A et al (2005) Acute respiratory distress syndrome: underrecognition by clinicians and diagnostic accuracy of three clinical definitions. Crit Care Med 33:2228–2234
Rubenfeld GD, Caldwell E, Granton J, Hudson LD, Matthay MA (1999) Interobserver variability in applying a radiographic definition for ARDS. Chest 116:1347–1353
Acknowledgments
Instituto de Salud Carlos III FIS PI 12/02898, and FIS PI 12/02451. European Network (7th FP) ITN 264864.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Take-home message: The presence of DAD in ARDS patients defines a specific clinical-pathological entity, which means that the knowledge sourced from ARDS studies which do not take histology into account should be considered very cautiously as they include different entities (only half of ARDS patients present DAD).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lorente, J.A., Cardinal-Fernández, P., Muñoz, D. et al. Acute respiratory distress syndrome in patients with and without diffuse alveolar damage: an autopsy study. Intensive Care Med 41, 1921–1930 (2015). https://doi.org/10.1007/s00134-015-4046-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4046-0