Abstract
Purpose
Caloric insufficiency during the first week of intensive care unit (ICU) stay was reported to be associated with increased infection rates, especially ICU-acquired bloodstream infection (ICU-BSI). However, the predisposition to ICU-BSI by a given pathogen remains not well known. We aimed to determine the impact of early energy-calorie deficit on the pathogens responsible for ICU-BSI.
Design
Prospective, observational, cohort study in a 18-bed medical ICU of a tertiary care hospital.
Methods
Daily energy balance (energy-calorie intakes minus calculated energy-calorie expenditure) was compared according to the microbiological results of the blood cultures of 92 consecutive prolonged (at least 96 h) acute mechanically ventilated patients who developed a first episode of ICU-BSI.
Results
Among the 92 ICU-BSI, nine were due to methicillin-resistant Staphylococcus aureus (MRSA). The cumulated energy deficit of patients with MRSA ICU-BSI was greater than those with ICU-BSI caused by other pathogens (−1,348 ± 260 vs −1,000 ± 401 kcal/day from ICU admission to day of ICU-BSI, p = 0.008). ICU admission, risk factors for nosocomial infections, nutritional status, and conditions potentially limiting feeding did not differ significantly between the two groups. Patients with MRSA ICU-BSI had lower delivered energy and similar energy expenditure, causing higher energy deficits. More severe energy deficit and higher rate of MRSA blood cultures (p = 0.01 comparing quartiles) were observed.
Conclusions
Early in-ICU energy deficit was associated with MRSA ICU-BSI in prolonged acute mechanically ventilated patients. Results suggest that limiting the early energy deficit could be a way to optimize MRSA ICU-BSI prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacteremia is one of the major causes of nosocomial infection in the intensive care unit (ICU) [1–4]. ICU-acquired bloodstream infection (ICU-BSI) is associated with increased morbidity and length of stay, resulting in excess costs and high mortality of critically ill patients [3–7]. Although there are variations due to heterogeneous information sources and variety of local clinical practices, coagulase-negative staphylococci, Staphylococcus aureus, and Enterobacteriaceae species are the pathogens most frequently responsible for nosocomial bacteremia [1, 3, 4, 6]. The distribution of pathogens responsible for nosocomial bacteremia differs markedly in the ICUs where multidrug-resistant bacteria like Pseudomonas spp. or methicillin-resistant staphylococci are highly dominant [2, 4, 8–10]. Increased mortality due to ICU-BSI is associated with host conditions, responsible pathogen(s), time to ICU-BSI, and appropriateness of treatment [4, 10]. Specialized ICUs, severity at ICU admission, longer length of ICU stay, colonization with multidrug-resistant pathogens, intravenous catheters or invasive procedures, and low caloric intake are known risk factors for developing ICU-BSI [3, 5–7, 10–12]. However, the predisposition to ICU-BSI by a given pathogen is still not well known, probably because the numerous risk factors for ICU-BSI may render the analysis of the susceptibility to infection by a given pathogen difficult.
Protein–energy malnutrition (PEM) is commonly associated with impaired immune responses and affects the clinical course of some infections, such as pneumonia or bacteremia [12–14]. ICU patients are prone to develop early protein–energy deficit. The latter is associated with a higher rate of nosocomial infections, longer ICU stays, and higher healthcare costs [15]. Energy deficit in ICU patients is mainly caused by reduced intake due to underprescribed calories and frequent feeding interruptions because of gastrointestinal intolerance or diagnostic and/or therapeutic procedures [16–19]. Energy deficit results in an early energy gap during the first week of ICU stay, which is never overcome thereafter [16]. Cumulated energy deficit build-up during the first days of ICU stay appears to be an independent factor contributing to nosocomial infections [15, 16, 20]. In addition, a large negative energy balance was observed during prolonged acute mechanical ventilation in the most critically ill patients and might affect their ICU outcomes [18]. However, randomized intervention studies limiting energy deficit by combining parenteral nutrition with insufficient enteral nutrition have yielded conflicting results among ICU-acquired nosocomial infections [21–23]. Indeed, limiting early energy deficit in ICU patients might be reserved for those that are in a situation of chronic critical illness, e.g., patients with prolonged acute mechanical ventilation (at least 96 h) and severe energy deficits are likely to benefit most from preventive measures [15, 24, 25]. In this context, we have previously shown that the level of energy deficit is an independent determinant for acquiring S. aureus ventilator-associated pneumonia in ICU patients receiving prolonged acute mechanical ventilation [26]. The aim of this study was therefore to investigate the impact of energy deficit on the microbiological results of the blood cultures of prolonged acute mechanically ventilated patients who experienced a first ICU-BSI episode.
Methods
Patients and study design
This prospective, observational, cohort study was conducted from January 2004 to December 2012 in the 18-bed medical ICU of a tertiary teaching hospital. Because of the observational design, no local institutional review board authorization was required according to French bioethics laws. The study was approved by the Commission Nationale de l’Informatique et des Libertés to use the computerized medical data with protection of patient confidentiality. Adult patients intubated at ICU admission and mechanically ventilated for at least 96 h before a first ICU-BSI episode were eligible for analysis. Exclusion criteria included previous episodes of nosocomial bloodstream infection during the current hospital stay, and the rare cases of total parenteral nutrition, thus limiting bias in the analysis of the risk factors for ICU-BSI. All study patients were ventilated with an Evita 4 ventilator (Dräger Medical, Antony, France). Enteral nutrition (EN) (Fresubin Original®, Fresenius-Kabi, France, 0.9 kcal/ml, 55 % carbohydrates, 35 % lipids, and 15 % proteins) was to be started within 24 h of ICU admission, and increased in accordance with the recommendations of the Société de Reanimation de Langue Française as detailed elsewhere [18]. Combining enteral with parenteral nutrition was not used during the study period. When required, glycemia control was achieved by insulin infusion with a glucose cut-off value of 8 mmol/l. Systematic precise nutritional intake (daily estimation of resting energy expenditure (REE), energy-calorie prescribed and delivered) was calculated from ICU admission to day of ICU-BSI to focus our investigations on the early level of energy balance and its impact on the pathogen(s) responsible for ICU-BSI.
ICU-acquired bloodstream infections
ICU-BSI was defined as onset of infection and at least one positive blood culture result unrelated to an infection incubating at ICU admission occurring after 48 h of ICU stay [4]. All blood cultures (BacT ALERT®, Biomérieux Inc, Durham, NC) were obtained from peripheral blood samples by trained nurses. ICU-BSI not related to another site of infection was classified as primary. ICU-BSI related to a causative source of infection (lung, intra-abdominal, urine, soft tissue, and intravascular catheter) was classified as secondary. Catheter-related infections were documented by quantitative tip cultures. Multidrug-resistant microorganisms were defined as methicillin-resistant S. aureus (MRSA), vancomycin-resistant enterococci, third-generation cephalosporins-resistant Enterobacteriaceae, imipinem/ceftazidine- or fluoroquinolones-resistant Pseudomonas aeruginosa, and ticarcillin-resistant Acinetobacter baumannii according to national [27] and local Anti-Infectious Comities definitions. Coagulase-negative Staphylococcus bacteremia and polymicrobial ICU-BSIs were excluded from analysis, thereby limiting confounding.
Energy balance
Total energy prescribed was calculated from glucose infusions and EN prescriptions. Energy really delivered daily included energy from enteral feeding and glucose infusions. Propofol was not used for continuous sedation. Because indirect calorimetry was not available for every patient, the daily REE was calculated with the following validated equation, incorporating static and dynamic biometric parameters that measure the highly variable and rapidly changing REE (kcal/day) of critically ill patients [18, 26]: 8 × body weight (kg) + 14 × height (cm) + 32 × minute ventilation (l/min) + 94 × body temperature (°C) − 4,834. Every day from ICU admission to day of ICU-BSI, the following data were collected from charts: weight measured with an electronic scale, temperature (mean of four values measured electronically at 6-h intervals), and minute ventilation (mean of four values determined with the respiratory device at 6-h intervals). Height, assessed with measuring tape and the patient lying in a supine position, was collected at ICU admission. Every day, from ICU admission to day of ICU-BSI, energy balance (energy-calorie really delivered minus REE) was calculated. Since the length of stay from ICU admission to ICU-BSI was not constant, cumulated energy balance was expressed per day of ICU stay before ICU-BSI, thereby limiting temporal relationship. Stored energy (adipose tissue, intramuscular triglycerides, and blood fatty acids or triglycerides) was ignored for the calculation of energy balance [28].
Patient data
Baseline demographic data at the time of ICU admission included age, smoking status, immune deficiencies (corticosteroids, diabetes, cancer treatment, transplants, others), main diagnosis, and simplified acute physiology score (SAPS) II. Protein-calorie malnutrition at ICU admission was assessed by the nutritional risk score (NRS) and actual weight less than 90 % of ideal body weight [16, 29, 30]. Other risk factors for nosocomial infections (prior antibiotics or prior hospitalization within 3 months, previous colonization with multidrug-resistant pathogens or carriage of multidrug-resistant bacteria screened at ICU admission in high-risk patients by using rectal swabs, central venous catheters, transfusions of blood products, days on mechanical ventilation, hemodialysis), days with EN interruptions due to gastrointestinal intolerance or ICU procedures, and days on medications that could diminish nutrient absorption or limit the prescribed feeding-rate volume were assessed from ICU admission to the day of ICU-BSI [18, 26].
Statistical analyses
Results are expressed as numbers (%), means ± SD, or medians (range) for data with non-normal distributions. The sample size was calculated a priori on the basis of the following assumptions: an expected minimal difference in energy deficit of 250–500 kcal/day between groups has clinical relevance. To detect such differences, using a β risk of 0.20, an α error of 0.05, and an energy deficit SD close to 250 kcal/day, at least 34 patients (17/group) for a difference of 250 kcal/day or 12 patients (6/group) for a difference of 500 kcal/day are required. Between groups comparisons used Student’s t test for normally distributed variables. Non-normally distributed variables were compared with the Mann–Whitney U test. Fisher’s exact test was applied for comparisons of categorical variables. Factors with a significance of p < 0.20 in the univariate analysis were considered for multivariate analysis. Logistic regression was used for multivariate analysis. Relationships between pathogen-positive blood cultures and energy-deficit quartiles were assessed using analysis for linear trends in proportion (Mantel–Haenszel test). Statistics were calculated with the StatView 4.5 (Abacus Concept Inc., Berkeley, CA, USA) and EPI INFO 3.4 (Centers for Disease Control and Prevention, Atlanta, GA, USA) software. p < 0.05 was considered significant.
Results
Patients and blood cultures
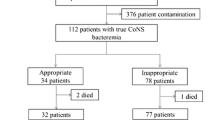
During the study period, 92 patients intubated at ICU admission and on mechanical ventilation for at least 96 h before a first ICU-BSI episode were eligible for analysis. The main characteristics of the studied patients and usual risk factors for nosocomial infections are summarized in Table 1, which also details the nutritional intake results from ICU admission to day of ICU-BSI. Among the 92 episodes of positive blood cultures, 36 were due to Enterobacteriaceae (Escherichia coli, n = 18; Klebsiella pneumoniae, n = 6; Proteus mirabilis, n = 5; Enterobacter cloacae, n = 3; Citrobacter koseri, n = 2; Morganella morganii, n = 1; Serratia marcescens, n = 1), 25 grew Staphylococcus aureus, 10 Pseudomonas aeruginosa, 10 Streptococcus spp. (Streptococcus pneumoniae, n = 3; Streptococcus mitis, n = 3; Streptococcus anginosus, n = 2; Streptococcus oralis, n = 1; Streptococcus constellatus, n = 1), six Enterococcus faecalis, three Bacteroides fragilis, one Acinetobacter baumannii, and one Fusobacterium. Nineteen microorganisms isolated from blood cultures were considered as multidrug-resistant: MRSA, n = 9; Escherichia coli, n = 3; Klebsiella pneumonia, n = 2; Pseudomonas aeruginosa, n = 1; Proteus mirabilis, n = 1; Enterobacter cloacae, n = 1; Acinetobacter baumannii, n = 1; Serratia marcescens, n = 1. Twenty ICU-BSI were classified primary. Among the 72 secondary ICU-BSI, the causative source of infection was ventilator-associated pneumonia in 39 cases, 10 were intra-abdominal, nine were catheter-related infections, nine soft tissues, and five urinary tract.
Energy balance and pathogens responsible for ICU-BSI
Energy balance did not differ significantly between patients infected with Gram-positive (n = 41) or Gram-negative (n = 51) pathogens (−1,068 ± 379 vs −1,007 ± 421 kcal/day from ICU admission to day of NBI, p = 0.39). As shown in Table 2, patients with MRSA ICU-BSI had a significantly higher mean energy deficit than those with positive blood cultures due to other pathogens. Energy balance was not associated with the multidrug resistance of isolated microorganism (−1,131 ± 444 for 19 patients with ICU-BSI caused by multidrug-resistant pathogens vs −1,009 ± 390 kcal/day for 73 patients with ICU-BSI due to non-multidrug-resistant pathogens, p = 0.24) or with the causative source of infection (−1,175 ± 392 for 20 patients with primary ICU-BSI vs −995 ± 399 kcal/day for 72 patients with secondary ICU-BSI, p = 0.07). Energy balance was comparable for patients with (n = 51) or without (n = 41) immune deficit (−1,053 ± 366 vs −1,010 ± 447 kcal/day, p = 0.47).
Factors associated with MRSA ICU-BSI
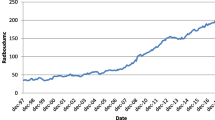
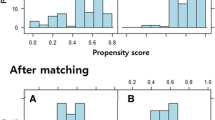
Patients with MRSA blood cultures had similar characteristics and risk factors for nosocomial infections to those with ICU-BSI due to other microorganism(s) (Table 1). Primary/secondary ICU-BSI ratio did not differ significantly between patients with MRSA positive blood cultures and those with positive blood cultures due to other microorganism(s) (3/6 and 17/66, respectively, p = 0.40). Nutritional status at ICU admission, conditions potentially limiting EN, REE, and intubation duration before ICU-BSI were similar for the two groups. However, patients with MRSA ICU-BSI had lower prescribed or delivered energy, resulting in higher energy deficits (Table 1). Patients with MRSA ICU-BSI had a daily energy deficit higher than those with ICU-BSI due to other microorganism(s) and that difference was statistically significant from day 4 of mechanical ventilation (Fig. 1). Logistic regression analysis identified energy balance as being independently associated with MRSA positive blood cultures (Table 3). The estimated odds ratios for MRSA-positive blood culture associated with an increase in energy deficit of 250 or 500 kcal/day from ICU admission to ICU-BSI were respectively 2.12, 95 % CI [1.28–3.40] and 4.48, 95 % CI [1.65–11.58]. An increasing trend for MRSA-positive blood cultures across the energy-deficit quartiles estimated between ICU admission and day of ICU-BSI was found with the Mantel–Haenszel test (Fig. 2).
Evolution of daily energy deficit of patients with MRSA ICU-BSI (n = 9) and those with ICU-BSI due to other microorganism(s) (n = 83). ICU intensive care unit, MRSA methicillin-resistant Staphylococcus aureus, ICU-BSI ICU-acquired bloodstream infection. Values are means with their standard deviations depicted by vertical bars. *p < 0.05, # p < 0.01 MRSA vs other pathogens
Relationship between MRSA-positive blood culture and cumulated energy-deficit quartiles estimated between ICU admission and day of positive blood culture for 92 patients with a first episode of ICU-BSI. ICU intensive care unit, MRSA methicillin-resistant Staphylococcus aureus, ICU-BSI ICU-acquired bloodstream infection, OR odds ratio (comparison vs second quartile). Values are expressed as percentages with 95 % confidence intervals (blue vertical lines). Cumulated energy from ICU admission to day of ICU-BSI was normalized by the duration of ICU stay (or intubation duration) before ICU-BSI. Asterisk statistics were assessed with the analysis for linear trends in proportion (Mantel–Haenszel test)
Discussion
The results of this study demonstrated that large negative energy balance was independently associated with MRSA ICU-BSI. This study confirms previous data indicating that early energy deficit is a risk factor for acquiring Staphylococcus aureus infectious complications in the ICU [26]. The relationship between chronic PEM and Staphylococcus aureus infections was identified a century ago in malnourished children in developing countries. Chronic PEM leads to T lymphocyte deficiency and impaired immune regulation and worsens mucous membrane oxidative stress and barrier defects, causing changes in microbial flora and increasing susceptibility to bacterial and viral infections. The increasing trend for MRSA acquisition across energy-deficit magnitudes herein suggests that acute caloric insufficiency favors MRSA ICU-BSI in critically ill patients through other mechanisms.
The magnitude of the gap between calculated REE and prescribed energy intakes was unexpected considering the procedures used to enable adequate feeding. The present result may be explained, at least in part, by the inclusion of very seriously ill patients with a high incidence of clinical situations predisposing to gastroparesis or interruption of feeding. Another explanation may be the relatively high incidence of renal failure in our patients necessitating limitation of feed volume to limit fluid overload. Additionally, the duration of EN interruptions for procedures or severe gastrointestinal intolerance could explain the differences between delivered and prescribed energy-calories. However, more than 70 % of the energy prescribed was delivered, suggesting that energy deficit was not mostly caused by nursing practices. We conclude that unintentional underestimation of energy-calorie requirements, delay in starting or increasing EN, and overprecautionary interruptions in EN resulted in underfeeding in our ICU patients. Our findings illustrate the gap between evidence and practice (“the true life”) for EN support in the most severely injured patients. Finally, the present observational study indicates that the gap between recommended nutrition care and practice regarding enteral feeding still exists and it results from lack of knowledge and interest of the importance of nutritional assessment by nurses and doctors.
The rate of MRSA ICU-BSI in our patient population and the proportion of primary/secondary ICU-BSI are consistent with the literature data [3–5, 10]. Risk factors for acquisition of Staphylococcus aureus bacteremia are prior colonization, severity of underlying disease, previous antibiotics use, length of hospital stay, older age, chronic hemodialysis, and immune deficiency, while the risks for acquiring MRSA infection appear to be dominated by the presence of patients colonized with MRSA in the same ICU, previous antibiotic use, and central venous catheter insertion [11]. MRSA is one of the leading causes of nosocomial infection associated with higher mortality and costs. That is why infection control programs based on identification and isolation of MRSA-colonized or MRSA-infected patients, antibiotic policy, hand hygiene, and care of central venous catheters have been underway for more than a decade with contrasting results depending on the type of patients, geographic area, and local settings [31, 32]. Indeed, traditional MRSA control methods have focused on the prevention of cross-transmission, while the majority of nosocomial infections seem to be of endogenous origin [33]. Host responses to infection are commonly pathogen specific in animals and humans. In this way, the present findings suggest that early in-ICU energy deficit is an MRSA ICU-BSI risk factor readily accessible to preventive measures by limiting large energy deficit the first week of ICU stay in acute chronic critically ill patients.
Clinical and experimental evidence supporting that caloric insufficiency is associated with Staphylococcus aureus methicillin resistance remain scarce. In a previous study, we found that the link between early in-ICU energy deficit and Staphylococcus aureus ventilator-associated pneumonia was independent of methicillin sensitivity [26]. Differences between ventilator-associated pneumonia and ICU-BSI pathogenesis may explain, at least in part, this apparent discrepancy. Indeed, staphylococcal adhesion on abiotic surfaces, such as central venous catheters, is mediated by the expression of microbial surface component-recognizing adhesive matrix molecules and the production of polysaccharide intercellular adhesins leading to bacterial aggregation and biofilm production [34]. In contrast, damage or destruction of the respiratory epithelium by exotoxins is a necessary condition for fostering the adhesion of Staphylococcus aureus on epithelial basal membrane.
The regulation of many Staphylococcus aureus virulence determinants by host nutrient availability has been extensively examined [35]. Acute environmental and nutritional stresses, such as pulses of carbon availability, markedly affect the modulation of staphylococcal virulence determinants via catabolite control protein A (CcpA) repression, a transcriptional regulator, leading to biofilm production and biosynthesis of capsular polysaccharides or toxigenic proteins like α-toxin or toxic shock syndrome toxin-1 [35, 36]. Other regulators, such as Agr, CodY, or atl, are stimulated by changes in nutrient substrates, increasing Staphylococcus aureus virulence [35, 36]. However, there is no evidence that MRSA is more virulent than MSSA [37]. To date, no data support that carbohydrate availability may regulate the staphylococcal chromosomal cassette mec (SCCmec), which encodes Staphylococcus aureus resistance to β-lactams and other antibiotics [38]. However, MgrA, a multiple gene regulator controlling several efflux systems that confer Staphylococcus aureus resistance to antibiotics, is modulated by host nutrient availability [35]. In addition, Staphylococcus aureus expresses nitrogen-dependent regulators as GlnR that regulates glutamine synthetase, which is important for maintaining methicillin resistance in MRSA [35], suggesting the possibility of pharmaco-nutrition intervention for optimizing MRSA ICU-BSI prevention in critically ill patients [39]. Further investigations are needed to determine how acute energy deficits and pulses of nutrient availability facilitate Staphylococcus aureus resistance to antibiotics and promote virulence characteristics favoring ICU-BSI caused by MRSA in humans.
A limitation of this study is the relatively small sample of MRSA ICU-BSI and caution is needed before extrapolating the present results beyond our patient population and procedures of enteral feeding. The high ICU mortality rate observed herein is similar to a previous cohort of patients in which a large negative energy balance was an independent determinant of ICU outcome [18], suggesting that limiting early energy deficit should be reserved for the sickest patients. The present investigation was undertaken to compare patients with ICU-BSI caused by different microorganisms, but not patients with and without ICU-BSI. Another possible limitation is REE estimation with a predictive method, even though the equation was validated in mechanically ventilated patients [40]. Nevertheless, indirect calorimetry, the gold standard for REE assessment, is not available everywhere and it has been shown that more than 40 % of mechanically ventilated ICU patients had conditions invalidating calorimetric measurements [41]. Consequently, most current studies comparing measured REE and predicted REE are skewed by lack of clear steady state criteria or quality criteria to validate the calorimetric measurements during the metabolic assessments [18, 40, 41]. In the absence of such criteria, many clinical conditions are responsible for erroneous values of O2 consumption, CO2 production, and REE [40, 41]. In addition, most of these research studies fail to address the presentation of data that might influence energy expenditure and CO2 production: catecholamines, opioid agonists, β2-agonists, neuromuscular blocking agents, body temperature, type of nutrition (formulation) administered, continuation of enteral feeding during calorimetric measurements, and the mode of mechanical ventilation used. These biases largely explain why there are sometimes large discrepancies between modern multiparametric predictive equation estimates and indirect calorimetry measurements in individuals and group.
Conclusion
Our findings demonstrated that early negative energy balance was an independent determinant of MRSA ICU-BSI in prolonged acute mechanically ventilated patients. Feeding prescriptions based on limiting the energy deficit during the first week of ICU stay could be a way to optimize MRSA ICU-BSI prevention.
References
Brun-Buisson C, Doyon F, Carlet J, Dellamonica P, Gouin F, Lepoutre A, Mercier JC, Offenstadt G, Régnier B (1995) Incidence, risk factors, and outcome of severe sepsis and septic shock in adults. A multicenter prospective study in intensive care units. French ICU group for severe sepsis. JAMA 274:968–974
Brun-Buisson C, Doyon F, Carlet J (1996) Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. French Bacteremia-Sepsis Study Group. Am J Respir Crit Care Med 154:617–624
Laupland KB, Kirkpatrick AW, Church DL, Ross T, Gregson DB (2004) Intensive-care-unit-acquired bloodstream infections in a regional critically ill population. J Hosp Infect 58:137–145
Garrouste-Orgeas M, Timsit JF, Tafflet M, Misset B, Zahar JR, Soufir L, Lazard T, Jamali S, Mourvillier B, Cohen Y, De Lassence A, Azoulay E, Cheval C, Descorps-Declere A, Adrie C, Costa de Beauregard MA, Carlet J (2006) Excess risk of death from intensive care unit-acquired nosocomial bloodstream infections: a reappraisal. Clin Infect Dis 42:118–126
Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ (2002) Population-based assessment of intensive care unit-acquired bloodstream infections in adults: incidence, risk factors, and associated mortality rate. Crit Care Med 30:2462–2467
Wenzel RP (2007) Health care-associated infections: major issues in the early years of the 21st century. Clin Infect Dis 45:S85–S88
Tacconelli E, Smith G, Hieke K, Lafuma A, Bastide P (2009) Epidemiology, medical outcomes and costs of catheter-related bloodstream infections in intensive care units of four European countries: literature- and registry-based estimates. J Hosp Infect 72:97–103
Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, Wolff M, Spencer RC, Hemmer M (1995) The prevalence of nosocomial infection in intensive care units in Europe. Results of the European prevalence of infection in intensive care (EPIC) study. EPIC international advisory committee. JAMA 274:639–644
Garrouste-Orgeas M, Chevret S, Mainardi JL, Timsit JF, Misset B, Carlet J (2000) A one-year prospective study of nosocomial bacteraemia in ICU and non-ICU patients and its impact on patient outcome. J Hosp Infect 44:206–213
Tabah A, Koulenti D, Laupland K, Misset B, Valles J, Bruzzi de Carvalho F, Paiva JA, Cakar N, Ma X, Eggimann P, Antonelli M, Bonten MJ, Csomos A, Krueger WA, Mikstacki A, Lipman J, Depuydt P, Vesin A, Garrouste-Orgeas M, Zahar JR, Blot S, Carlet J, Brun-Buisson C, Martin C, Rello J, Dimopoulos G, Timsit JF (2012) Characteristics and determinants of outcome of hospital-acquired bloodstream infections in intensive care units: the EUROBACT international cohort study. Intensive Care Med 38:1930–1945
Garrouste-Orgeas M, Timsit JF, Kallel H, Ben Ali A, Dumay MF, Paoli B, Misset B, Carlet J (2001) Colonization with methicillin-resistant Staphylococcus aureus in ICU patients: morbidity, mortality, and glycopeptide use. Infect Control Hosp Epidemiol 22:687–692
Rubinson L, Diette GB, Song X, Brower RG, Krishnan JA (2004) Low caloric intake is associated with nosocomial bloodstream infections in patients in the medical intensive care unit. Crit Care Med 32:350–357
Chandra RK (1997) Nutrition and the immune system: an introduction. Am J Clin Nutr 66:S460–S466
Cunningham-Rundles S, McNeeley DF, Moon A (2005) Mechanisms of nutrient modulation of the immune response. J Allergy Clin Immunol 56:S73–S76
Berger MM, Pichard C (2012) Best timing for energy provision during critical illness. Crit Care 16:215
Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux RNMC, Delarue J, Berger MM (2005) Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 24:502–509
Petros S, Engelmann L (2006) Enteral nutrition delivery and energy expenditure in medical intensive care patients. Clin Nutr 25:51–59
Faisy C, Lerolle N, Dachraoui F, Savard JF, Abboud I, Tadie JM, Fagon JY (2009) Impact of energy deficit calculated by a predictive method on outcome in medical patients requiring prolonged acute mechanical ventilation. Br J Nutr 101:1079–1087
Passier RH, Davies AR, Ridley E, McClure J, Murphy D, Scheinkestel CD (2013) Periprocedural cessation of nutrition in the intensive care unit: opportunities for improvement. Intensive Care Med 39:1221–1226
Dvir D, Cohen J, Singer P (2006) Computerized energy balance and complications in critically ill patients: an observational study. Clin Nutr 25:37–44
Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Lev S, Grozovski E, Theilla M, Frishman S, Madar Z (2011) The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 37:601–609
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G (2011) Early versus late parenteral nutrition in critically ill adults. New Engl J Med 365:506–517
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, Thibault R, Pichard C (2013) Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet 381:385–393
Kyle UG, Genton L, Heidegger CP, Maisonneuve N, Karsegard VL, Huber O, Mensi N, Andre Romand J, Jolliet P, Pichard C (2006) Hospitalized mechanically ventilated patients are at higher risk of enteral underfeeding than non-ventilated patients. Clin Nutr 25:727–735
Zilberberg MD, Kramer AA, Higgins TL, Shorr AF (2009) Prolonged acute mechanical ventilation: implications for hospital benchmarking. Chest 135:1157–1162
Faisy C, Candela Llerena M, Savalle M, Mainardi JL, Fagon JY (2011) Early ICU energy deficit is a risk factor for Staphylococcus aureus ventilator-associated pneumonia. Chest 140:1254–1260
French Ministry of Health (1999) Control measures to limit the spread of multi-drug resistant bacteria: recommendations for healthcare institutions. http://www.sante.gouv.fr/maitrise-de-la-diffusion-des-bacteries-multiresistantes-aux-antibiotiques.html. Assessed 3 Sept 2014
Berger MM, Revelly JP, Cayeux MC, Chiolero RL (2005) Enteral nutrition in critically ill patients with severe hemodynamic failure after cardiopulmonary bypass. Clin Nutr 1:124–132
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G (2009) Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). J Parenteral Enteral Nutr 33:277–316
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z (2003) Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 22:321–336
Butterly A, Schmidt U, Wiener-Kronish J (2010) Methicillin-resistant Staphylococcus aureus colonization, its relationship to nosocomial infection, and efficacy of control methods. Anesthesiology 113:1453–1459
Carbonne A, Arnaud I, Maugat S, Marty N, Dumartin C, Bertrand X, Bajolet O, Savey A, Fosse T, Eveillard M, Sénéchal H, Coignard B, Astagneau P, Jarlier V, MDRB Surveillance National Steering Group (BMR-Raisin) (2013) National multidrug-resistant bacteria (MDRB) surveillance in France through the RAISIN network: a 9 year experience. J Antimicrob Chemother 68:954–959
Silvestri L, Monti Bragadin C, Milanese M, Gregori D, Consales C, Gullo A, Van Saene HK (1999) Are most ICU infections really nosocomial? A prospective observational cohort study in mechanically ventilated patients. J Hosp Infect 42:125–133
Yarwood JM, Bartels DJ, Volper EM, Greenberg EP (2004) Quorum sensing in Staphylococcus aureus biofilms. J Bacteriol 186:1838–1850
Somerville GA, Proctor RA (2009) At the crossroads of bacterial metabolism and virulence factor synthesis in staphylococci. Microbiol Mol Biol Rev 73:233–248
Seidl K, Müller S, François P, Kriebitzsch C, Schrenzel J, Engelmann S, Bischoff M, Berger-Bächi B (2009) Effect of a glucose impulse on the CcpA regulon in Staphylococcus aureus. BMC Microbiol 9:95
Gordon RJ, Lowy FD (2008) Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis 46:S350–S359
DeLeo FR, Diep BA, Otto M (2009) Host defense and pathogenesis in Staphylococcus aureus infections. Infect Dis Clin North Am 23:17–34
Briassoulis G, Filippou O, Hatzi E, Papassotiriou I, Hatzis T (2005) Early enteral administration of immunonutrition in critically ill children: results of a blinded randomized controlled clinical trial. Nutrition 21:799–807
Savard JF, Faisy C, Lerolle N, Guerot E, Diehl JL, Fagon JY (2008) Validation of a predictive method for an accurate assessment of resting energy expenditure in medical mechanically ventilated patients. Crit Care Med 36:1175–1183
Faisy C, Guerot E, Diehl JL, Labrousse J, Fagon JY (2003) Assessment of resting energy expenditure in mechanically ventilated patients. Am J Clin Nutr 78:241–249
Acknowledgments
We are indebted to Patrick Grohs for microbiological database management.
Conflicts of interest
The authors have not disclosed any potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: This study indicates that early negative energy balance is an independent determinant of methicillin-resistant Staphylococcus aureus nosocomial bacteremia in acute prolonged mechanically ventilated patients. Feeding prescriptions to limit early energy deficit during intensive care unit stay appear to be a potential way to optimize prevention of methicillin-resistant S. aureus nosocomial bacteremia.
Rights and permissions
About this article
Cite this article
Ekpe, K., Novara, A., Mainardi, JL. et al. Methicillin-resistant Staphylococcus aureus bloodstream infections are associated with a higher energy deficit than other ICU-acquired bacteremia. Intensive Care Med 40, 1878–1887 (2014). https://doi.org/10.1007/s00134-014-3502-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3502-6