Abstract
Purpose
Assess the relationship between optic nerve sheath diameter (ONSD) measured on bedside portable computed tomography (CT) scans and simultaneously measured intracranial pressure (ICP) in patients with severe traumatic brain injury.
Methods
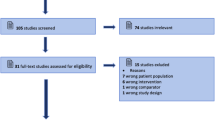
Retrospective cohort study of 57 patients admitted between 2009 and 2013. Linear and logistic regression were used to model the correlation and discrimination between ONSD and ICP or intracranial hypertension, respectively.
Results
The cohort had a mean age of 40 years (SD 16) and a median admission Glasgow coma score of 7 (IQR 4–10). The between-rater agreement by intraclass coefficient was 0.89 (95 % CI 0.83–0.93, P < 0.001). The mean ONSD was 6.7 mm (SD 0.75) and the mean ICP during CT was 21.3 mmHg (SD 8.4). Using linear regression, there was a strong correlation between ICP and ONSD (r = 0.74, P < 0.001). ONSD had an area under the curve to discriminate elevated ICP (≥20 mmHg vs. <20 mmHg) of 0.83 (95 % CI 0.73–0.94). Using a cutoff of 6.0 mm, ONSD had a sensitivity of 97 %, specificity of 42 %, positive predictive value of 67 %, and a negative predictive value of 92 %. Comparing linear regression models, ONSD was a much stronger predictor of ICP (R 2 of 0.56) compared to other CT features (R 2 of 0.21).
Conclusions
Simultaneous measurement of ONSD on CT and ICP were strongly correlated and ONSD was discriminative for intracranial hypertension. ONSD was much more predictive of ICP than other CT features. There was excellent agreement between raters in measuring ONSD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with severe traumatic brain injury (TBI), increased intracranial pressure (ICP) is an important cause of secondary brain injury and is a strong predictor of poor neurologic outcome in this population [1–3]. As a result of the rigid nature of the cranium, the intracranial compliance deteriorates precipitously with expansion of space-occupying lesions or cerebral edema due to limited intracranial compensatory reserve [4]. Ultimately, elevated ICP in this setting results in secondary ischemic injury by limiting cerebral blood flow, the principle determinant of cerebral oxygen delivery after TBI [5, 6]. The Brain Trauma Foundation guidelines recommend invasive ICP monitoring in patients who present with a severe TBI with a post resuscitation Glasgow coma score (GCS) of less than 9 [7]. However, access to ICP monitoring is not universal and may require triage and transfer of patients with a TBI. Unfortunately, the traditional features that are used on computerized tomography (CT) head imaging (midline shift >5 mm, basal cistern and sulcal effacement) do not reliably predict elevated ICP [8, 9]. ICP may be highly dynamic, almost instantly changing its value from normal baseline to grossly elevated [10]. Moreover, significant elevations in ICP > 20–25 mmHg due to cerebral edema, acute hydrocephalus, or space-occupying lesions are of importance for managing TBI despite results of recently conducted studies [11] and refinement of appropriate selection of patients suitable for invasive ICP monitoring has been advocated [12]. Noninvasive determination of ICP, as measured by optic nerve sheath diameter (ONSD), has garnered increased interest to identify patients for invasive ICP neurmonitoring [13].
The optic nerve sheath is continuous with the meninges of the central nervous system and is encased with the subarachnoid membrane. Cerebrospinal fluid (CSF), located in the subarachnoid space, accumulates in the optic nerve sheath thereby widening its diameter in the setting of increased ICP and limited intracranial compliance [14, 15]. Human studies have shown that this phenomenon occurs within minutes of acute changes in ICP [14–16].
Ultrasonography of ONSD in TBI patients has been shown to correlate with increased ICP [17–24] and systemic reviews have supported this observation [25, 26]. Although reliability of ONSD measurements with ultrasound has been established, an element of technical expertise is required to obtain adequate images which likely limits its ubiquitous clinical utility [27, 28]. ONSD measurement on magnetic resonance imaging (MRI) has been evaluated and also correlates with increased ICP [13–29]. Unfortunately, limited availability and imaging time constraints of MRI preclude its widespread use as a real-time estimate of ICP. Alternatively, ONSD measurements on MRI and CT are strongly correlated [30], with the latter modality being widely available for patients with TBI. Increased ONSD measured on CT scanning has been associated with mortality [31]. Unfortunately, few patients in this study underwent ICP monitoring, precluding the ability to examine for an association between ONSD and ICP. Therefore, the objective of our study was to determine the association between simultaneously obtained ONSD measured on portable bedside CT, and ICP in patients with severe TBI. In addition, we aimed to determine the ability of ONSD to discriminate between intracranial hypertension, ICP > 20 mmHg versus normotension, ICP ≤ 20 mmHg, as defined by international guidelines on the management of severe TBI [32]. Finally, we compared ONSD to other imaging features of elevated ICP on CT scan to the measured ICP.
Methods
This was a single-center retrospective cohort study and is reported as per the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines [33]. The protocol was approved by the Research Ethics Boards at the University of Cambridge who waived the requirement for written informed consent.
Patient inclusion and data collection
We used a database of all patients admitted to the Neurocritical Care Unit at Addenbrooke’s Hospital between 1 January 2009 and 31 December 2013 to identify eligible patients. We included adult patients (older than 18 years) with a closed TBI (admission GCS < 9) if they underwent invasive ICP monitoring recorded continuously on ICM+® brain monitoring software (Division of Neurosurgery, Cambridge University) and a portable bedside head CT during their admission. We excluded patients with an ocular or retro-orbital injury.
Data were collected into a standardized electronic case report forms using a Microsoft Excel 2013® database (Redmond, WA, USA). We collected the following characteristics: admission GCS, age, gender, and 6-month Glasgow outcome scores (GOS). We also collected information on the location, mechanism, and severity of TBI. The ICP for each patient was obtained from archived patient data that was recorded on the ICM+® brain monitoring which directly records data output from the Codman® ICP monitoring system (Codman & Shurtlett®, MA, USA). Continuous ICP measurements (each minute) were averaged over a 15-min period (from the start of CT scan to its completion of acquisition of all images) encompassing the duration of the head CT scan with portable bedside CT scanner which allowed one to avoid possible transport-induced increase in ICP. In addition, we collected the RAP index which is a measure of intracranial compensatory reserve. It is the correlation coefficient (R) between 30 samples of amplitude (A) and mean intracranial pressure (P), averaged over 10-s intervals [34].
The Rotterdam and Marshall scores were calculated using the admission CT head scan reports from the consultant neuroradiologist [35]. Presence of imaging features of increased ICP including midline shift >5 mm, herniation, compressed ventricles, basal cistern, and sulcal effacement were also recorded from these reports.
Study site
Affiliated with the University of Cambridge, the Neurocritical Care Unit at Addenbrooke’s Hospital is a 23-bed critical care unit at a tertiary trauma referral center which specializes in the management of neurotrauma and multimodal intracranial monitoring. It operates on an approximately 1:1.2 nurse-to-patient ratio with neurocritical care consultants and housestaff in attendance.
TBI management
The neurocritical care unit uses a TBI management protocol [36]. The TBI protocol aims to minimize ICP by using a tier approach to institute management strategies such as intravenous sedation, neuromuscular paralysis, osmolar therapy, therapeutic hypothermia, cerebral spinal fluid diversion, and surgical therapy. ICP is continuously recorded by the Codman® ICP monitoring system and archived by the ICM+® software on a bedside computer in real time.
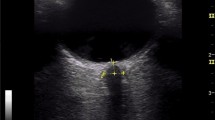
Computed tomography and ONSD measurements
Portable bedside head CT, with reconstruction slices <5 mm (CereTom®, Neurologica Danvers MA, USA), was performed on all patients included in the study [37]. Independently, five investigators (CR, EN, KW, NM, MS) blinded to the patient’s condition, demographics, baseline characteristics, clinical and physiologic data and who were not involved with data collection measured bilateral ONSD on all the portable CT head scans. For measurement, CT scan images were displayed on a digital viewer (Centricity PACS, General Electric Healthcare, USA). The images were magnified 2× on the particular image slice which demonstrated the largest diameter of the optic nerve sheaths. The images were changed to the ‘chest/abdomen’ window (Hounsfield unit range +25 to +40) which demonstrated the optic nerve sheaths in greatest detail and the ONSD was measured 3 mm behind the globe in a perpendicular vector in reference to the linear axis of the nerve. The optic nerve sheath is encased by the meningeal membranes, including the dural reflection. The ONSD was measured in its entirety which likely included a minor contribution of the meninges to the total width. We considered an optic nerve sheath adequate for measurement if the ONSD could be measured 3 mm behind the orbit and was not obscured by surrounding structures.
Statistical methods
We used Stata 10.0 (StataCorp, Texas, USA) and SPSS Statistics 20 (IBM Corporation, New York, USA) to analyze our data. The mean ONSD across the two sides and the mean ICP during the 15 min of the bedside portable head CT acquisition were used for the analysis. We described categorical data, normally distributed data, and non-normally distributed data using proportions [percent; 95 % confidence intervals (CI)], mean [standard deviation (SD)] and median [interquartile range (IQR)], respectively. Bivariate comparisons of continuous variables were done using t tests for normally distributed data and Wilcoxon signed-rank test for non-normally distributed data where appropriate. Bivariate comparisons of proportions were done using a Fisher’s exact test. We calculated the intraclass coefficient (ICC) to determine the between-rater and between-side agreement of ONSD measurements.
Simple linear regression was used to plot the relationship between simultaneously measured ONSD and ICP. The correlation coefficient (r) was calculated using the square root of the R 2 value from the model. We also used linear regression to determine the relationship between ONSD and RAP. In order to assess the ability of ONSD to predict intracranial hypertension, univariable logistic regression was used to model the association between ONSD and elevated ICP (>20 mmHg vs. ≤20 mmHg). This was used to calculate the area under the receiver operating curve (AUC). Finally, we wanted to compare ONSD to other CT head predictors of elevated ICP (cisternal effacement, sulcal effacement, ventricular compression, and cerebral herniation) [9]. To accomplish this, we compared two models, which contained all of these factors with and without ONSD included as an independent variable. These two models were then compared using a likelihood ratio test. We assess for linearity by visual inspection of the scatter plot between ICP and the continuous variable of interest. Residual homoscedasticity was ensured by plotting the standardized residuals against the predicted values following the linear regression. Residual normality was assessed by plotting a kernal density plot of the residuals. Multicolinearity was assessed by calculating the variance inflation factor (VIF). A VIF < 10 was interpreted as an absence of multicolinearity. The sample size was one of convenience and represented the number of patients in whom simultaneous ONSD and ICP data was available within the database. A complete case analysis was performed and we considered a P < 0.05 to be statistically significant.
Results
During the study period, 190 patients were admitted with a severe TBI with invasive neuromonitoring. Sixty-two patients had a simultaneous CT scan while undergoing continuous ICP monitoring. Five patients were excluded because the optic nerve sheaths were not amendable to visualization secondary to obscuration by surrounding structures due to orbital trauma, leaving 57 included in the final analysis (Table 1). Thirteen of 57 (23 %) patients had a poor outcome (GOS 1 or 2) and 5 of 57 (9 %) died.
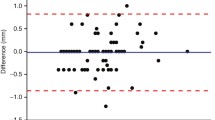
The between-rater agreement for ONSD measurements as determined by ICC was 0.89 (95 % CI 0.83–0.93, P < 0.001). ICC between right and left ONSD measurements was 0.96 (95 % CI 0.93–0.98, P < 0.001). The mean ONSD was 6.7 mm (SD 0.75) and the mean ICP during CT was 21.3 mmHg (SD 8.4). Using simple linear regression, there was a linear correlation between ICP and ONSD (r = 0.74, P < 0.001) (Fig. 1 and Table 2). Although there was a linear relationship between ONSD and RAP (r = 0.35, P = 0.007) there was considerable variability around the point estimate (data not shown).
Scatterplot of intracranial pressure (ICP, mmHg) and optic nerve sheath diameter (mm). The solid line is the linear prediction from the univariable regression. The short dashed lines are the 95 % confidence intervals for the linear prediction. The long dashed lines are the 95 % prediction interval for ICP given ONSD
ONSD displayed an AUC for the ability to elevated ICP (≥20 mmHg vs. <20 mmHg) of 0.83 (95 % CI 0.73–0.94) (Fig. 2). Using a cutoff of 6.0 mm, ONSD had the following performance characteristics: sensitivity 97 %, specificity 42 %, positive predictive value (PPV) 67 %, and negative predictive value (NPV) 92 %. Using a cutoff of 7.0 mm, the performance characteristics were sensitivity 45 %, specificity 96 %, PPV 93 %, and NPV 60 %. A complete table of diagnostic test characteristics is presented in the Electronic Supplementary Material.
Receiver operating curve (ROC) for ONSD on the risk of developing intracranial hypertension (ICP ≥ 20 mmHg). It is a plot of the true positive rate (sensitivity) vs. the false positive rate (1 − specificity) at various thresholds of ONSD. The area under the curve is a measure of the diagnostic accuracy for ONSD of predicting intracranial hypertension. The dotted line represents a test which is no better than chance
The results of the simple (model A) and multivariable (models B and C) linear regression models are presented in Table 2. Simple linear regression modeling ICP to ONSD had an R 2 value of 0.56 (model A). The multivariable linear regression containing only the CT predictors of increased ICP (model B) had an R 2 of 0.21. Addition of ONSD to model B resulted in an increased R 2 to 0.60 (model C). Likelihood ratio testing between model C and model A (i.e., model A nested within model C) revealed that the addition of the CT predictors to the model containing ONSD failed to improve the predictive ability of the model (P = 0.15). There was no evidence of colinearity on either multivariable model with the highest VIF being 2.3.
Discussion
In our single-center retrospective cohort study, we demonstrated a linear association between ONSD measured on portable CT and simultaneously measured ICP in critically ill patients with severe TBI. ONSD measurements showed excellent agreement both between raters and between sides in the same patient. ONSD also showed excellent discriminative ability to predict patients with intracranial hypertension. Finally, ONSD was a much stronger predictor of ICP than traditional CT features of intracranial hypertension (cisternal effacement, sulcal effacement, ventricular compression, and cerebral herniation).
The linear relationship between ONSD and ICP demonstrated in our study is similar to previously published studies using ultrasound [13, 22, 23] and MRI [29]. Prior studies have also confirmed the ability of ONSD on ultrasound and MRI to discriminate between elevated from non-elevated ICP with AUC above 0.90 [23, 29]. In the ultrasound study by Geeraerts et al. [23], the AUC was 0.91 with the best cutoff value being 5.86 mm which offered a sensitivity of 95 % and a specificity of 79 %. Subsequently, Geeraerts et al. [29] demonstrated that ONSD on MRI had an AUC of 0.94 with a cutoff of 5.82 mm having a sensitivity of 90 % and a specificity of 92 %. The AUC in our study (0.86), although highly discriminative, does not perform as well as these two prior studies. Furthermore, although the sensitivity seen in our study (97 %) at a cutoff of 6.0 mm was consistent with the two prior studies, the specificity observed (42 %) was much lower, affording a higher risk of a false-positive results. Discrepancies in these results may reflect differences in patient populations, discriminative abilities of the modalities, or a combination of both. It is likely that ONSD measurements on ultrasound or MRI would have higher accuracy and be less subject to measurement bias compared to those obtained on CT imaging. However, the benefit of CT is that it is more widely available than MRI and does not require the imaging acquisition expertise of ultrasound. Although ultrasound has good intraobserver reliability with repeated exams, there is definite skill acquisition required [28]. In contrast, our results demonstrate strong intraobserver reliability even with minimal training.
There is a sound biologic mechanism for ONSD to increase with ICP. The optic nerve sheath is continuous with the subarachnoid membrane and CSF is located in the space between the sheath and optic nerve [15]. ONSD widens when CSF is redistributed into the optic nerve sheath and this process likely occurs during limited intracranial compensatory reserve and compliance. The RAP index is a correlation coefficient (R) between amplitude (A) and mean intracranial pressure (P) and is a surrogate measure of intracranial compliance. A RAP approximating 0 indicates good compensatory reserve and adequate intracranial compliance [34]. Whereas, a RAP approaching +1 indicates limited compensatory reserve and intracranial compliance. In our study there was a linear correlation between increased ONSD and the RAP index, suggesting that ONSD likely widens from CSF shunting into the optic nerve sheath when intracranial compensatory reserve is limited.
An important limitation of ONSD estimation of ICP is that the distension of the optic nerve sheath requires normal intracranial CSF flow dynamics. Following TBI, CSF flow dynamics may become altered, in particular if obstructive hydrocephalus ensues or with placement of an external ventricular drain which is used for therapeutic CSF removal during episodes of increased ICP [38]. In these instances, altered CSF flow dynamics may make the interpretation of optic nerve sheath distension during increased episodes of ICP unreliable. In our cohort, no patients had obstructive hydrocephalus and only three patients had an EVD. This precludes examining the performance of ONSD in these subgroups. An important future step for investigation would be to examine ONSD in patients with obstructive hydrocephalus who have simultaneous invasive ICP monitoring with EVDs.
Finally, ONSD was a much better predictor of ICP than the CT findings of cisternal effacement, sulcal effacement, ventricular compression, and cerebral herniation. Thus, ONSD measured on CT could serve as a noninvasive predictor of intracranial hypertension in patients without invasive intracranial monitoring. Although our findings do not suggest a cutoff that is simultaneously sensitive and specific, the measurement of ONSD performs well at extremes. Thus, in our population, a low ONSD has a high negative predictive value and effectively rules out intracranial hypertension. This may be useful when triaging patients in the setting of limited resources. Furthermore, estimate of intracranial hypertension could be extrapolated to disease states when invasive neuromonitoring is contraindicated, such as fulminant hepatic failure with cerebral edema as well as concurrent coagulopathy and hypoxemic-ischemic brain injury post cardiac arrest with concomitant use of antiplatelet or anticoagulant therapies. However, these inferences are speculative and require further study.
Our study has important limitations that need to be considered. As with all observational studies, residual or unmeasured confounding may be an alternative explanation for our results. However, it is unclear what unmeasured or residual confounders would be independently associated with ONSD and ICP, limiting confounding as a significant source of bias. Importantly, we have a relatively small, single-center cohort of patients with TBI which limits the external validity. Furthermore, selection bias is likely as only a minority of patients within the cohort underwent simultaneous portable CT head scanning with ICP monitoring. Clinicians select which patients should undergo both CT scanning and ICP monitoring and these decisions will differ between clinicians and centers. Thus, extrapolation of our results to patients with less severe TBI, or with other disease states, should be done with caution. Future study with a larger population and multiple centers would help improve the external validity of our results.
Conclusion
In critically ill patients with severe TBI, ONSD measured on non-contrast CT was linearly associated with mean ICP recorded by invasive neuromonitoring. ONSD was also highly discriminatory in predicting intracranial hypertension (ICP ≥ 20 mmHg vs. <20 mmHg). ONSD also had superior predictive value for increased ICP compared to classical CT findings of intracranial hypertension. Finally, ONSD measurements on CT were highly reproducible among observers making its clinical utility potential generalizable.
References
Myburgh JA, Cooper DJ, Finfer SR et al (2008) Epidemiology and 12-month outcomes from traumatic brain injury in Australia and New Zealand. J Trauma 64:854–862
Juul N, Morris GF, Marshall SB, Marshall LF (2000) Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg 92:1–6
Vik A, Nag T, Fredriksli OA et al (2008) Relationship of “dose” of intracranial hypertension to outcome in severe traumatic brain injury. J Neurosurg 109:678–684
Treggiari MM, Schutz N, Yanez ND, Romand J-A (2007) Role of intracranial pressure values and patterns in predicting outcome in traumatic brain injury: a systematic review. Neurocrit Care 6:104–112
Balestreri M, Czosnyka M, Hutchinson P et al (2006) Impact of intracranial pressure and cerebral perfusion pressure on severe disability and mortality after head injury. Neurocrit Care 4:8–13
Chesnut RM, Marshall LF, Klauber MR et al (1993) The role of secondary brain injury in determining outcome from severe head injury. J Trauma 34:216–222
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care (AANS/CNS) et al (2007) Guidelines for the management of severe traumatic brain injury. I. Blood pressure and oxygenation. J Neurotrauma 24 Suppl 1:S7–S13
Hiler M, Czosnyka M, Hutchinson P et al (2006) Predictive value of initial computerized tomography scan, intracranial pressure, and state of autoregulation in patients with traumatic brain injury. J Neurosurg 104:731–737
Miller MT, Pasquale M, Kurek S et al (2004) Initial head computed tomographic scan characteristics have a linear relationship with initial intracranial pressure after trauma. J Trauma 56:967–972. Discussion 972–973
Czosnyka M, Pickard JD (2004) Monitoring and interpretation of intracranial pressure J Neurol Neurosurg Psychiatry 75:813–821
Chesnut RM, Temkin N, Carney N et al (2012) A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 367:2471–2481
Stocchetti N, Picetti E, Berardino M et al (2014) Clinical applications of intracranial pressure monitoring in traumatic brain injur: report of the Milan consensus conference. Acta Neurochir. doi:10.1007/s00701-014-2127-4
Kimberly HH, Noble VE (2008) Using MRI of the optic nerve sheath to detect elevated intracranial pressure. Crit Care 12:181
Launey Y, Nesseler N, Le Maguet P et al (2014) Effect of osmotherapy on optic nerve sheath diameter in patients with increased intracranial pressure. J Neurotrauma 31:984–988
Helmke K, Hansen HC (1996) Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatr Radiol 26:701–705
Hansen HC, Helmke K (1997) Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg 87:34–40
Soldatos T, Karakitsos D, Chatzimichail K et al (2008) Optic nerve sonography in the diagnostic evaluation of adult brain injury. Crit Care 12:R67
Cammarata G, Ristagno G, Cammarata A et al (2011) Ocular ultrasound to detect intracranial hypertension in trauma patients. J Trauma 71:779–781
Blaivas M, Theodoro D, Sierzenski PR (2003) Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med 10:376–381
Tayal VS, Neulander M, Norton HJ et al (2007) Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med 49:508–514
Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL (2011) Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care 15:506–515
Geeraerts T, Launey Y, Martin L et al (2007) Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med 33:1704–1711
Geeraerts T, Merceron S, Benhamou D et al (2008) Non-invasive assessment of intracranial pressure using ocular sonography in neurocritical care patients. Intensive Care Med 34:2062–2067
Kimberly HH, Shah S, Marill K, Noble V (2008) Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med 15:201–204
Moretti R, Pizzi B (2011) Ultrasonography of the optic nerve in neurocritically ill patients. Acta Anaesthesiol Scand 55:644–652
Dubourg J, Javouhey E, Geeraerts T et al (2011) Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med 37:1059–1068
Moretti R, Pizzi B, Cassini F, Vivaldi N (2009) Reliability of optic nerve ultrasound for the evaluation of patients with spontaneous intracranial hemorrhage. Neurocrit Care 11:406–410
Ballantyne SA, O’Neill G, Hamilton R, Hollman AS (2002) Observer variation in the sonographic measurement of optic nerve sheath diameter in normal adults. Eur J Ultrasound 15:145–149
Geeraerts T, Newcombe VFJ, Coles JP et al (2008) Use of T2-weighted magnetic resonance imaging of the optic nerve sheath to detect raised intracranial pressure. Crit Care 12:R114
Kalantari H, Jaiswal R, Bruck I et al (2013) Correlation of optic nerve sheath diameter measurements by computed tomography and magnetic resonance imaging. Am J Emerg Med 31:1595–1597
Legrand A, Jeanjean P, Delanghe F et al (2013) Estimation of optic nerve sheath diameter on an initial brain computed tomography scan can contribute prognostic information in traumatic brain injury patients. Crit Care 17:R61
Bratton SL, Chestnut RM, Ghajar J et al (2007) Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma 24(Suppl 1):S55–S58
Vandenbroucke JP, von Elm E, Altman DG et al (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 18:805–835
Radolovich DK, Aries MJH, Castellani G et al (2011) Pulsatile intracranial pressure and cerebral autoregulation after traumatic brain injury. Neurocrit Care 15:379–386
Maas AIR, Hukkelhoven CWPM, Marshall LF, Steyerberg EW (2005) Prediction of outcome in traumatic brain injury with computed tomographic characteristics: a comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery 57:1173–1182; discussion 1173–82
Patel HC, Menon DK, Tebbs S et al (2002) Specialist neurocritical care and outcome from head injury. Intensive Care Med 28:547–553
Rumboldt Z, Huda W, All JW (2009) Review of portable CT with assessment of a dedicated head CT scanner. AJNR Am J Neuroradiol 30:1630–1636
Czosnyka M, Pickard JD (2004) Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry 75:813–821
Acknowledgments
We would like to acknowledge the staff of the Neurocritical Care Unit at Addenbrooke’s Hospital for their support in the completion of this study.
Conflicts of interest
The ICM+ brain monitoring software (http://www.neurosurg.cam.ac.uk/icmplus) is licensed by the University of Cambridge. Dr. Czosnyka and Dr. Smielewski have a financial interest in the licensing fee.
Ethical standard
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Optic nerve sheath diameter measured on head computed tomography is correlated with intracranial pressure. Increased optic nerve sheath diameter is a more sensitive and specific predictor of increased intracranial pressure than classical CT findings suggestive of intracranial hypertension.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sekhon, M.S., Griesdale, D.E., Robba, C. et al. Optic nerve sheath diameter on computed tomography is correlated with simultaneously measured intracranial pressure in patients with severe traumatic brain injury. Intensive Care Med 40, 1267–1274 (2014). https://doi.org/10.1007/s00134-014-3392-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3392-7