Abstract
Background
In severe sepsis, guidelines recommend de-escalating the empirical antimicrobial treatment as soon as the microbiological results are available. We aimed to determine the rate of de-escalation of the empirical antimicrobial treatment in neutropenic patients with severe sepsis. The characteristics of antimicrobial treatment associated with de-escalation and its impact on short- and long-term survival were also determined.
Methods
In the intensive care unit (ICU) of a cancer referral center, we prospectively collected observational data related to the antimicrobial management in neutropenic patients who developed severe sepsis and were admitted to ICU for at least 48 h. De-escalation of antimicrobial therapy consisted either of deleting one of the empirical antibiotics of a combined treatment, or, whenever possible, to use a betalactam antibiotic with a narrower spectrum of activity. Multivariate logistic regression was conducted to determine the factors associated with de-escalation, while a Cox proportional hazards model with a time-dependent covariate was fitted to assess the effect of de-escalation on 30-day survival. Finally 1-year survival after ICU discharge was compared across de-escalation groups.
Results
Cumulative incidence of de-escalation of the empirical antimicrobial treatment among the 101 patients of the cohort was 44 %, [95 % confidence interval (CI) 38–53 %], including 30 (68 %) patients with ongoing neutropenia. A microbiological documentation was available in 63 (63 %) patients. Factors associated with de-escalation were the adequation of the empirical antimicrobial treatment in ICU [OR = 10.8 (95 % CI 1.20–96)] for adequate documented treatment versus appropriate empirical treatment, the compliance with guidelines regarding the empirical choice of the anti-pseudomonal betalactam [OR = 10.8 (95 % CI 1.3–89.5)]. De-escalation did not significantly modify the hazard of death within the first 30 days [HR = 0.51 (95 % CI 0.20–1.33)], nor within 1 year after ICU discharge [HR = 1.06 (95 % CI 0.54–2.08)].
Conclusion
Our data suggest that, in ICU, de-escalation of the empirical antimicrobial treatment is frequently applied in neutropenic cancer patients with severe sepsis. No evidence of any prognostic impact of this de-escalation was found.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In severe sepsis and septic shock, guidelines recommend de-escalating the empirical antimicrobial treatment as soon as the microbiological results are available [1]. This strategy is aimed to reduce the selection pressure and the treatment cost [2, 3]. In intensive care units (ICU), previous studies have shown that de-escalation is safe [4–6]. As routine, de-escalation is performed in around 40 % of septic patients [7].
Neutropenia remains a constant outcome after aggressive chemotherapies as part of bone marrow transplantation, acute leukemia, lymphoma, and certain solid tumor treatments. The price to pay for increasing treatment intensity and duration is a rise in treatment-related toxicity and susceptibility to infection [8, 9]. Thus, in neutropenic patients, suspicion of sepsis should lead to the immediate onset of empirical antimicrobial treatment [10, 11]. In the neutropenic patient with severe sepsis or septic shock, use of broad-spectrum antibiotics is recommended [11]. The changes of empirical antimicrobial treatment should be guided by clinical and microbiological data [12]. To date, there is no study assessing the safety of de-escalation in neutropenic patients with severe sepsis.
Our hypothesis was that de-escalation is feasible in about 40 % of the patients with neutropenia at the onset of severe sepsis. Our first aim was to assess the rate of de-escalation of the first antimicrobial treatment in neutropenic cancer patients with severe sepsis or septic shock admitted to the ICU. Our secondary aims were to test whether characteristics of the empirical antimicrobial treatment (namely, adequation to documentation and compliance to guidelines) were associated with de-escalation, and to determine the impact of the de-escalation on the patient survival.
Methods
All neutropenic cancer patients admitted to the ICU of the Paoli-Calmettes Institute (Marseille, France) from January 2008 to May 2010 and meeting criteria for severe sepsis or septic shock were prospectively included in this observational survey. The patients deceased or discharged alive from the ICU within the first 48 h were excluded from the analysis. All patients were followed over a period of 12 months after ICU admission. The Paoli-Calmettes Institute is a 211-bed cancer referral center. The Institutional Review Board of the Paoli-Calmettes Institute approved this study and waived the need for informed consent due to the observational nature of the study. The methodology adheres to the STROBE statement.
Definitions and data collection
Neutropenia was defined as a neutrophil count below 500 cells/mm3 or leucocytes below 1,000 cells/mm3 [12]. Severe sepsis, septic shock, and acute respiratory distress syndrome (ARDS) were defined according to international criteria [13, 14]. Cancer status at ICU admission was graded as follows: newly diagnosed, remission, progression, or unknown. Knaus scale definitions were used to record pre-existing chronic organ failures [15]. Reasons for the ICU admission were categorized as acute respiratory failure, shock, coma, acute kidney injury, severe sepsis, tumor lysis syndrome, and others. Simplified acute physiology score (SAPS) II [16] and sequential organ failure assessment (SOFA) [17] scores were computed on day 1. During the first 5 days after ICU admission, changes in SOFA score (Δ SOFA) were calculated as follows: [score on day 5 (or the day of ICU discharge if discharge occured before day 5) – score on day 1]. When the Δ SOFA was >1, the SOFA score was considered as having worsened. Organ failure was defined as a SOFA score of 3 or more for any system. The patients were included if they had suspected or proven infection. From ICU admission, X-rays, computed tomography scan, and biological and microbiological tests were standardized and performed as indicated by the clinical presentation [12, 18, 19].
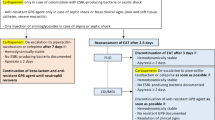
In agreement to guidelines, antibiotics were administered as early as possible after ICU admission [12, 20]. Aminoglycosides or fluoroquinolones were added in those patients requiring fluid resuscitation or vasopressors [12, 20]. Antibiotics directed against methicillin-resistant Staphylococcus aureus (MRSA) were used as recommended by guidelines [12, 20]. Patients with fever and neutropenia during more than 5 days received an antifungal agent. Our local guidelines recommend continuing antibiotics until clinical resolution was obtained.
For each patient, the episodes of febrile neutropenia were classified as fever of unknown origin, clinically documented or microbiologically documented [21]. A microbiologically documented infection was defined as fever with identification of pathogens in blood samples or samples from the suspected infection site. A clinically documented infection was defined as fever with a focal infection (e.g., pneumonia or skin and soft tissue inflammation) not accessible to specimen sampling or sampled with negative microbiological results. Fever of unknown origin was defined as fever >38 °C over at least 1 h or twice within 12 h, with no detectable cause. Details are available in the Online Supplementary File.
The last antimicrobial treatment before ICU admission and the first antimicrobial treatment after ICU admission were recorded. Antimicrobial treatment were categorized in a 4-class variable according to the existence of microbiological documentation and the compliance with guidelines. Thus, when microbiological documentation was available, antimicrobial treatment was considered as adequate, inadequate if it was active, or not active against the identified pathogens based on in vitro susceptibility testing. In the absence of microbiological documentation, antimicrobial treatment was considered as appropriate or inappropriate, based on the compliance with guidelines) [12]. For Gram-negative bacilli, monotherapy with aminoglycoside was considered as inappropriate [22].
De-escalation of the empirical antimicrobial treatment consisted of either deleting one of the antimicrobials of a combined treatment including anti-MRSA antibiotics, antifungal treatment, antiviral treatment, or, whenever possible, the use of betalactams with a narrower spectrum of activity [5]. Criteria for narrowing the antimicrobial regimen were based on the results of susceptibility testing of identified bacteria. In our ICU, de-escalation was not performed according to a protocol. It was left to the discretion of the senior intensivist. De-escalation was only evaluated during ICU stay. Escalation of antimicrobial treatment consisted of either the addition of an antibiotic of another family to the betalactam or the use of betalactam with a broader-spectrum of activity. A combination was defined as aminoglycosides or fluoroquinolones given in addition to betalactams.
Statistical analysis
Our hypothesis was that, as reported in non-neutropenic patients [4–7], de-escalation was feasible in 40 % of neutropenic patients with severe sepsis. Thus, the inclusion of 100 patients would permit the estimatation of the proportion of de-escalation with an imprecision [half the width of the 95 % confidence interval (CI)] of <10 %.
All data are presented as percentages for qualitative variables and median (25th–75th percentiles) for quantitative variables. The features of patients during their ICU stay were compared across the groups of patients undergoing de-escalation of the antimicrobial treatment (de-escalation group) and those who did not (non-de-escalation group) by using Fisher’s exact test and Wilcoxon rank-sum test. Our second hypothesis was that adequation of antimicrobial treatment was associated with de-escalation. A multivariate logistic model with AIC-based stepwise selection was fitted to identify which of the covariates that described compliance with guidelines was significantly independently associated with de-escalation. The Hosmer–Lemeshow test was used to check goodness-of-fit of the selected logistic model.
Effect of de-escalation on 30-day mortality was assessed by fitting a Cox proportional hazards model using de-escalation as a time-dependent covariate. For patients with de-escalation the same day of antibimicrobial treatment discontinuation (or discharge alive), de-escalation was considered as having been done 12 h before. A sensitivity analysis was performed by considering that, for these patients, no de-escalation was performed. Effect of de-escalation on long-term survival was estimated on the subset of patients discharged alive from ICU, by comparing 1-year survival post-ICU between patients for whom the antimicrobial treatment had or had not been de-escalated.
All tests were two-sided, and p values lower than 0.05 were considered statistically significant. Analysis was performed using SPSS, v.16.0 software (SPSS, Chicago, IL, USA) and R v.2.13 (http://www.R-project.org/).
Results
During the study period, severe sepsis and septic shock were diagnosed in 118 neutropenic patients out of 1,803 patients admitted to ICU. Seventeen (14 %) patients were excluded because they died within the first 48 h after admission. Thus, 101 patients were included in the study. The underlying cancers were acute leukemia (n = 44), lymphoma (n = 24), myeloma (n = 12), and miscellaneous (n = 21). Hematopoietic stem cell transplantation was observed in 24 patients, including 14 autologous and 10 allogeneic transplants (Table 1). ICU admission occurred 6 days (2–10) after the onset of neutropenia. Neutropenia duration was 11 days (8–16). In 52 patients, neutropenia was resolutive during the ICU stay. In ICU, granulocyte colony-stimulating factor (G-CSF) was used in 55 patients (Table 2).
Major reasons for ICU admission were acute respiratory failure (n = 36) and shock (n = 32) (Table 1). At ICU admission, sepsis was identified in 83 patients, and 18 patients developed a subsequent sepsis during the ICU stay. Septic shock and severe sepsis were identified in 54 and 47 patients, respectively (Table 2).
Totals of 63, 21, and 17 patients had microbiologically documented infections, clinically documented infections, and fever of unknown origin, respectively (Table 3). Bacteria (n = 63), fungi (n = 22), and viruses (n = 7) were identified in 59, 18, and 5 patients, respectively. Polymicrobial infection was found in 20 patients. The major sites of infection were lungs (n = 44) and abdomen (n = 11). Blood cultures were positive in 11 patients (Table 3). The characteristics of the microbiological documentation are available in Electronic Supplementary Material Table 1.
Before ICU admission, antibiotics were administered to 79 (79 %) patients. Betalactams were used in all but one patients. In 74 (94 %) of these 79 patients, they were active against Pseudomonas aeruginosa. Vancomycin and linezolid were used in 28 (35 %) and 2 (3 %) patients, respectively. A combined antibiotic was used in 36 (46 %) patients, consisting of aminoglycosides (n = 18) and fluoroquinolones (n = 18). Antifungal and antiviral agents were given to 30 (38 %) and 14 (18 %) patients, respectively.
In the ward, 79 patients received an empirical antimicrobial treatment. Among them, infection was microbiologically documented in 49 (62 %) patients, with adequate treatment in 27 (55 %) of these patients. The treatment was appropriate for 17 (57 %) out of the 30 patients without microbiological documentation. Twenty-two patients did not receive antibiotics before ICU admission. Among them, infection was microbiologically documented in 15 (68 %) cases.
After ICU admission, antimicrobial treatments were continued in 37 patients and initiated in 22 patients. Changes were performed in 42 patients. The time elapsed between the first antimicrobial therapy and the first signs of severe sepsis in ICU was 1.6 (0.7–3.1) h (Table 1). Betalactams were administered to all patients. They were inactive against Pseudomonas aeruginosa in 2 patients. In 57 patients, aminoglycosides (n = 27) or fluoroquinolones (n = 30) were added. Antibiotics active against MRSA were used in 48 patients. Antifungal and antiviral agents were used in 30 and 17 patients, respectively (Electronic Supplementary Material Table 2). The median duration of antimicrobial treatment was 7 days [4–14] for median duration of ICU stay of 9 days [5–18].
At ICU admission, the empirical antimicrobial treatment was appropriate in 50 patients and adequate in 42 patients. Eight out of the 38 patients without microbiological documentation received an appropriate treatment (Table 4). Of note, in these 38 patients, the anti-pseudomonal antibiotic was appropriate in 31 (82 %).
The empirical antimicrobial treatment was de-escalated in 44 patients of the 101 patients (Electronic Supplementary Material Fig. 1). Cumulative incidence of de-escalation in ICU at day 15 was 44 % (95 % CI 38–53 %) (Fig. 1). De-escalation was performed in 32 of the 63 (51 %) patients with microbiological documentation and 12 of the 38 (32 %) patients without microbiological documentation. The betalactam spectrum was narrowed in 22 (35 %) patients with microbiological documentation and 1 (3 %) patient without microbiological documentation. In 26 patients, the antibiotic directed against MRSA was discontinued. All de-escalation were performed within the first 12 days (Fig. 1). Of note, de-escalation of antifungal and antiviral agents was always concomitant to that of antibiotics. The severity of organ failures at ICU admission was similar in the de-escalation group and the non-de-escalation group (Table 1). The time elapsed between the severe sepsis onset and its ICU management was longer in the de-escalation group, compared to the non-de-escalation group but the difference did not reach statistical significance [2 (0–7) vs. 1 (0–3) days, p = 0.057] (Table 2). In 30 (30 %) patients, de-escalation was performed during neutropenia. The rate of escalation after de-escalation was 5 % (Electronic Supplementary Material Table 3).
Using a multivariate analysis, the characteristics of antimicrobial treatment independently associated with de-escalation were adequation of the empirical antimicrobial treatment used in ICU [OR = 10.8 (95 % CI 1.20–96)] for adequate documented treatment versus appropriate empirical treatment), and compliance with guidelines regarding the empirical anti-pseudomonal betalactam used in ICU [OR = 10.8 (95 % CI 1.3–89.5)] (Electronic Supplementary Material Table 4).
The ICU mortality rate was 23 %. The 23 deaths included 6 patients undergoing de-escalation during neutropenia, 2 patients undergoing de-escalation after neutropenia recovery, and 15 patients in the non-de-escalation group (p = 0.57). De-escalation was not associated with the hazard of death within the first 30 days [HR = 0.51 (95 % CI 0.20–1.33)], nor within the 1-year post-ICU-discharge [HR = 1.06 (95 % CI 0.54–2.08)] (Electronic supplementary material Fig. 2). Among patients discharged alive, median duration of antibiotherapy in ICU was 9 days [4–12] in the de-escalation group versus 5 days [3–8] in the non-de-escalation group (p = 0.005). In the de-escalation group, cancer status and G-CSF use were not associated with ICU death. During the ICU stay, 7 (22 %) out of 32 patients in the no-remission group died, compared to 1 (8 %) out of 12 patients in the remission group (p = 0.15). Five (17 %) out of 29 patients treated with GCS-F and 3 (20 %) out of 15 patients not treated with G-CSF died (p = 1).
Discussion
To our knowledge, this study is the first evaluation of de-escalation in neutropenic cancer patients requiring ICU. As expected, the empirical antimicrobial treatment was de-escalated in about 40 % of this population. In ICU, an adequate empirical antimicrobial treatment and the compliance to guidelines regarding the first anti-pseudomonal betalactam agent are critical for initiating the process of de-escalation. De-escalation did not affect the patient outcomes.
In the hematological patients with sepsis and neutropenia, the empirical choice of antimicrobials remains a matter of debate [23]. Two approaches are opposed to each other. The escalation approach consists of avoiding the use of broad-spectrum antibiotics. In this strategy, the treatment is escalated in the patient with clinical worsening or after the identification of a resistant pathogen. This strategy reduces toxicity, selection pressure, and cost. However, the delayed use of an effective treatment can negatively impact the outcomes [24, 25]. In contrast, de-escalation consists of the empirical use of broad-spectrum antibiotics. This strategy is efficient in covering all possible pathogens [2], but it exposes broad-spectrum antibiotics to overuse [24, 26]. Previous studies showed the safety of de-escalation in patients with septic shock, although no randomized clinical trials are available [4].
In our series, the empirical antimicrobial treatment was de-escaladed in 44 % of the neutropenic patients. No apparent effect on mortality was observed. Initial organ failures did not affect the strategy, suggesting that the decision was not guided by the patient severity. The rate of de-escalation did not differ from that reported in non-neutropenic patients [5–7, 27]. Importantly, our study was conducted in ICU. It is important to underline that our patients were continuously monitored. Thus, our results cannot be extrapolated to conventional wards. One should note that 5 % of patients required escalation after de-escalation failure [5, 28]. In a cancer ICU, de-escalation seems feasible and safe.
The neutropenic patients are at high risk of complications, due to altered immune response [29, 30]. Guidelines suggest continuing antimicrobial treatment until neutropenia recovery. They recommend the changing of antibiotics on the basis of microbiological results [11, 12]. There are no data supporting this statement [11, 12]. In our study, 68 % of patients underwent de-escalation during neutropenia. We did not find a deleterious impact of de-escalation on the survival of this specific subgroup. Future studies are required to confirm this finding. In our study, the duration of treatment was increased in the de-escalation group, compared to the non-de-escalation group. Of importance, in the de-escalated patients, treatment was never interrupted before neutropenia recovery. In critically ill neutropenic cancer patients, recovering from neutropenia during the ICU stay is a critical step; before this time, supportive care including antimicrobial treatment is usually maintained [30].
The administration of an adequate empirical antimicrobial treatment was associated with de-escalation. In line with a previous study [1], this finding underlines the need to collect blood samples and specimens from the suspected sources of infection before the antibiotic onset [31]. In cancer patients, a standardized diagnostic approach has been associated with improved outcomes [18, 32]. Using both invasive and non-invasive procedures, this strategy resulted in a microbiological documentation in up to 60 % of patients [18, 32]. Elsewhere, the identification of pathogens has been associated with decreased mortality [33]. In agreement with previous findings, this strategy was associated with a relatively low rate of positive blood culture [18].
The second factor associated with de-escalation was the compliance to guidelines regarding the choice of the antipseudomonal agent [12]. The use of ceftazidime and ticarcillin/clavulanate was not associated with de-escalation. Of note, international guidelines recommend the avoidance of ceftazidime for empirical monotherapy of fever and neutropenia [12]. In contrast, the empirical use of carbapenem was significantly associated with a high rate of de-escalation. This suggests that a guidelines strategy based on an empirical broad-spectrum antimicrobial treatment followed by de-escalation is feasible in neutropenic patients [4].
In the 38 patients without microbiological documentation, the uses of antipseudomonal belactams, anti-MRSA antibiotics, and combined antibiotics were inappropriate in 7 (18 %), 15 (39 %), and 17 (45 %) patients, respectively. Thus, only 8 (21 %) of these patients received an antimicrobial treatment in compliance with the guidelines. In the septic neutropenic patients, initial antimicrobial treatment using combined antibiotics or anti-MRSA drugs remains a matter of debate [20]. In the wards of our institution, anti-MRSA drugs were largely used although MRSA were rarely identified. In ICU, in disagreement with the guidelines, the use of these antibiotics was often interrupted, based on our local ecology and the removal of invasive devices [20]. Surprisingly, we observed a high rate of patients receiving antifungals in the de-escalation group. One possible explanation is that, in those patients, the delay between the onset of sepsis and its ICU management was longer than in the non-de-escalated patients. Thus, an antifungal treatment was prior introduced as the guidelines recommend [11, 34]. Of note, antifungal treatment was interrupted in 50 % of de-escalated patients.
Our results show that de-escalation did not impact short-term mortality. Several factors can affect the relationship between de-escalation and mortality: early ICU discharge, adequacy of empirical antimicrobial therapy, and timing of antibiotic administration. In our opinion, de-escalation may probably not alter short-term mortality. Indeed, no study has reported significant differences between two adequate antimicrobial treatment in patients with septic shock [35].
Several limitations should be acknowledged. De-escalation was left to the discretion of the senior physician. This represents a confusing factor, limiting the application of this strategy. However, our rate of de-escalation was similar to that reported in previous studies [5–7, 27]. The identification of co-pathogens such as yeasts and viruses has not been reported elsewhere. The actual impact of those pathogens on the de-escalated patient outcomes remains unclear. Finally, our study cannot document the relationship between a potential time-varying confounder such as the evolution of organ failure during ICU and de-escalation.
In conclusion, for the first time, we show that, in ICU, de-escalation is frequently performed in neutropenic cancer patients with severe sepsis. This approach appears not to affect the outcomes. Future studies are required to confirm these preliminary findings.
References
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Kollef MH, Micek ST (2005) Strategies to prevent antimicrobial resistance in the intensive care unit. Crit Care Med 33:1845–1853
Shorr AF (2009) Review of studies of the impact on Gram-negative bacterial resistance on outcomes in the intensive care unit. Crit Care Med 37:1463–1469
Leone M, Bourgoin A, Cambon S, Dubuc M, Albanese J, Martin C (2003) Empirical antimicrobial therapy of septic shock patients: adequacy and impact on the outcome. Crit Care Med 31:462–467
Leone M, Garcin F, Bouvenot J et al (2007) Ventilator-associated pneumonia: breaking the vicious circle of antibiotic overuse. Crit Care Med 35:379–385
Rello J, Vidaur L, Sandiumenge A et al (2004) De-escalation therapy in ventilator-associated pneumonia. Crit Care Med 32:2183–2190
Heenen S, Jacobs F, Vincent JL (2012) Antibiotic strategies in severe nosocomial sepsis: why do we not de-escalate more often? Crit Care Med 40:1404–1409
Talpaz M, Shah NP, Kantarjian H et al (2006) Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 354:2531–2541
Vanneman M, Dranoff G (2012) Combining immunotherapy and targeted therapies in cancer treatment. Nat Rev Cancer 12:237–251
Song JU, Suh GY, Park HY et al (2012) Early intervention on the outcomes in critically ill cancer patients admitted to intensive care units. Intensive Care Med 38:1505–1513
Legrand M, Max A, Schlemmer B, Azoulay E, Gachot B (2011) The strategy of antibiotic use in critically ill neutropenic patients. Ann Intensive Care 1:22
Freifeld AG, Bow EJ, Sepkowitz KA et al (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of America. Clin Infect Dis 52:427–431
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Bernard GR, Artigas A, Brigham KL et al (1994) The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) Prognosis in acute organ-system failure. Ann Surg 202:685–693
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/north American multicenter study. JAMA 270:2957–2963
Vincent JL, de Mendonça A, Cantraine F et al (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Azoulay E, Mokart D, Lambert J et al (2010) Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med 182:1038–1046
Azoulay E, Schlemmer B (2006) Diagnostic strategy in cancer patients with acute respiratory failure. Intensive Care Med 32:808–822
Meunier F, Lukan C (2008) The first European conference on infections in leukaemia—ECIL1: a current perspective. Eur J Cancer 44:2112–2117
Buchheidt D, Bohme A, Cornely OA et al (2003) Diagnosis and treatment of documented infections in neutropenic patients–recommendations of the infectious diseases working party (AGIHO) of the German society of hematology and oncology (DGHO). Ann Hematol 82(Suppl 2):S127–S132
Harbarth S, Garbino J, Pugin J, Romand JA, Lew D, Pittet D (2003) Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med 115:529–535
Mikulska M, Akova M, Averbuch D, Klyasova G, Livemore D, Orasch C et al. 4th European Conference on Infections in Leukemia. http://www.ebmt.org/Contents/Resources/Library/ECIL/Documents/ECIL4%202011%20Bacterial%20resistance%20in%20Haematology.pdf. 14-2-2012
Trecarichi EM, Tumbarello M, Spanu T et al (2009) Incidence and clinical impact of extended-spectrum-beta-lactamase (ESBL) production and fluoroquinolone resistance in bloodstream infections caused by Escherichia coli in patients with hematological malignancies. J Infect 58:299–307
Tumbarello M, Spanu T, Sanguinetti M et al (2006) Bloodstream infections caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae: risk factors, molecular epidemiology, and clinical outcome. Antimicrob Agents Chemother 50:498–504
Safdar A, Rolston KV (2007) Stenotrophomonas maltophilia: changing spectrum of a serious bacterial pathogen in patients with cancer. Clin Infect Dis 45:1602–1609
Kollef MH (2006) Providing appropriate antimicrobial therapy in the intensive care unit: surveillance vs. de-escalation. Crit Care Med 34:903–905
Morel J, Casoetto J, Jospe R et al (2010) De-escalation as part of a global strategy of empiric antibiotherapy management. A retrospective study in a medico-surgical intensive care unit. Crit Care 14:R225
Karvunidis T, Chvojka J, Lysak D et al (2012) Septic shock and chemotherapy-induced cytopenia: effects on microcirculation. Intensive Care Med 38:1336–1344
Mokart D, van Craenenbroeck T, Lambert J et al (2012) Prognosis of acute respiratory distress syndrome in neutropenic cancer patients. Eur Respir J 40:169–176
Xu XJ, Tang YM, Liao C et al (2013) Inflammatory cytokine measurement quickly discriminates gram-negative from gram-positive bacteremia in pediatric hematology/oncology patients with septic shock. Intensive Care Med 39:319–326
Depuydt P, Benoit D, Vogelaers D et al (2006) Outcome in bacteremia associated with nosocomial pneumonia and the impact of pathogen prediction by tracheal surveillance cultures. Intensive Care Med 32:1773–1781
Azoulay E, Mokart D, Rabbat A et al (2008) Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data. Crit Care Med 36:100–107
Burghi G, Lemiale V, Seguin A et al (2011) Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med 37:1605–1612
Silva BN, Andriolo RB, Atallah AN, Salomao R (2013) De-escalation of antimicrobial treatment for adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst Rev 3:CD007934
Acknowledgments
The study was funded by the Department of Anesthesiology and Critical Care of Paoli-Calmettes Institute.
Conflicts of interest
M. L. has received consultancy fees from LFB Biomédicaments and honoraria from Fresenius Kabi and Novartis for lectures. D. M., A. S., L. C. C., J. P. B., M. F., G. S., P. B., S. D., N. V.,C. S., and J. L. B. declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mokart, D., Slehofer, G., Lambert, J. et al. De-escalation of antimicrobial treatment in neutropenic patients with severe sepsis: results from an observational study. Intensive Care Med 40, 41–49 (2014). https://doi.org/10.1007/s00134-013-3148-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3148-9