Abstract
Purpose
We aimed to evaluate post-resuscitation care, implementation of therapeutic hypothermia (TH) and outcomes of intensive care unit (ICU)-treated out-of-hospital cardiac arrest (OHCA) patients in Finland.
Methods
We included all adult OHCA patients admitted to 21 ICUs in Finland from March 1, 2010 to February 28, 2011 in this prospective observational study. Patients were followed (mortality and neurological outcome evaluated by Cerebral Performance Categories, CPC) within 1 year after cardiac arrest.
Results
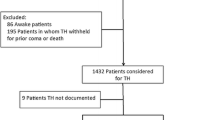
This study included 548 patients treated after OHCA. Of those, 311 patients (56.8 %) had a shockable initial rhythm (incidence of 7.4/100,000/year) and 237 patients (43.2 %) had a non-shockable rhythm (incidence of 5.6/100,000/year). At ICU admission, 504 (92 %) patients were unconscious. TH was given to 241/281 (85.8 %) unconscious patients resuscitated from shockable rhythms, with unfavourable 1-year neurological outcome (CPC 3–4–5) in 42.0 % with TH versus 77.5 % without TH (p < 0.001). TH was given to 70/223 (31.4 %) unconscious patients resuscitated from non-shockable rhythms, with 1-year CPC of 3–4–5 in 80.6 % (54/70) with TH versus 84.0 % (126/153) without TH (p = 0.56). This lack of difference remained after adjustment for propensity to receive TH in patients with non-shockable rhythms.
Conclusions
One-year unfavourable neurological outcome of patients with shockable rhythms after TH was lower than in previous randomized controlled trials. However, our results do not support use of TH in patients with non-shockable rhythms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Therapeutic hypothermia (TH) has been shown to improve outcome of patients resuscitated from out-of-hospital cardiac arrest (OHCA) caused by ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) [1, 2]. Thus, TH is the main therapeutic intervention of post-resuscitation care, with a strong recommendation based on evidence in OHCA patients resuscitated from VF/VT [3]. Previous retrospective studies have reported large variations in the degree of implementation of TH [4–7]. In Finland the degree of implementation of TH was 28 % in 2006 in all cardiac arrest patients, and 33 % in OHCA patients treated in ICU [6].
To date, no randomized controlled trials (RCT) on TH in patients resuscitated from non-shockable rhythms are available, and thus its possible effects on outcome are not known [8, 9]. Regardless of insufficient evidence, TH has been recommended for all OHCA patients chosen for active intensive care [3, 10]. However, neither the clinical implementation of this recommendation, nor the outcome of these patients treated with TH is known. Furthermore, as the incidence of out-of-hospital ventricular fibrillation (VF) has been decreasing during the past years also in Finland [11, 12], the use of TH in patients resuscitated from non-shockable rhythms may have increased.
Accordingly, in this nationwide prospective cohort study we aimed to evaluate post-resuscitation care, the use and implementation of TH and outcome of all adult OHCA patients admitted to Finnish intensive care units (ICUs). Our secondary aim was to determine the population-based incidence of OHCA.
Methods
Participating ICUs
All 22 Finnish ICUs treating OHCA patients were asked to participate in this study. In total 21, all five university hospitals with 7 ICUs, and 14 out of 15 central hospital ICUs consented to participate in this study. Approximately 98 % of the Finnish adult population (4.3 million www.stat.fi) live in the referral areas of these ICUs. All these ICUs belong to the Finnish Intensive Care Consortium (FICC).
Patients, sample size and treatment
The study protocol was approved by the Ethics Committee of each participating hospital. Inclusion criteria for the study were: (1) OHCA, (2) successful resuscitation, (3) age over 18 years and (4) post-resuscitation care in one of the participating ICUs.
Based on the national FICC database, there are 17,000 ICU admissions including approximately 800 cardiac arrest patients per year. We estimated that, of those 800 patients, 600 would be OHCA patients, which would provide an adequate sample size for a precise [95 % confidence interval (CI) ±1/100,000] assessment of the population-based incidence of OHCA, and comparison between incidences of OHCA with shockable and non-shockable rhythms. With this sample size, we assumed to include 300 OHCA-VF patients treated with TH. The proportions of OHCA patients with non-shockable rhythm treated and not treated with TH were not possible to predict. Thus, a study period of 1 year was set, from March 1, 2010 to February 28, 2011.
In this observational prospective study no recommendations for treatment of post-resuscitation syndrome [13, 14] and post-resuscitation care were given. National and European Resuscitation Councils (ERC) guidelines of post-resuscitation care [15, 16], national handbook of intensive care [17] and local ICUs’ standard operational protocols were used according to the decisions by the treating physicians. According to the Finnish intensive care handbook [17], TH is indicated only if: (1) cardiac arrest is witnessed, (2) initial rhythm is VF or VT and (3) patient is unconscious at hospital or ICU admission. Recent Scandinavian [10] and also the latest guidelines of the ERC 2010 [3] have recommended that TH should be considered also for patients from non-shockable rhythms if active treatment is chosen in the ICU.
Techniques of induction or maintenance of TH were not restricted. The majority of Finnish ICUs use endovascular cooling devices. We collected reasons if TH was not used in patients resuscitated from shockable rhythms.
Data collection
We collected data of study patients prospectively by using Internet-based case report forms (CRFs). We obtained pre-existing diagnoses of diabetes, coronary artery disease, hypertension, pacemaker, previous coronary artery bypass surgery (CABG), chronic heart failure or renal failure from the patients’ medical history. The aetiology of CA was determined according to Utstein criteria [18]. The FICC database was used for data collection and follow-up, including demographic data, haemodynamic data, Simplified Acute Physiology Score (SAPS) II, Acute Physiology and Chronic Health Evaluation (APACHE) II score, Therapeutic Intervention Scoring System (TISS) points, length of stay (LOS) in ICU and hospital mortality. Ninety-day mortality was collected from Statistics Finland. One specialist in neurology (M.T.) was blinded to treatment in ICU and aetiology of CA before she contacted alive patients by phone 1 year after cardiac arrest and used a structured interview to determine neurological outcome according to Pittsburgh Cerebral Performance Categories (CPC) [19]. Good neurological outcome was defined as CPC 1–2, and poor neurological outcome as CPC 3–4–5. A comprehensive list of data acquired from the FICC database and the CRF are presented as Electronic Supplementary Material (ESM) (Appendix 1).
Incidence calculation
We used patient logs of each ICU to crosscheck the number of patients, to separate OHCA patients from in-hospital cardiac arrest patients and to combine data of patients treated in more than one ICU during the same hospitalization. The number of the adult population (≥18 years), 4,290,980 at the end of year 2010, was obtained from Statistics Finland. The adult population of the hospital district of one non-participating ICU was excluded from the whole Finnish adult population. The total reference population for the incidence calculations was 4,205,407 at 31/12/2010.
Statistical analysis
We present continuous data as median values with interquartile ranges (IQR, 25–75 %) and categorical data as numbers and percentages. We compared groups using non-parametric Mann–Whitney U test for continuous data and Fisher’s exact test for proportions, when applicable. Patients who were awake at ICU admission were included in incidence calculations but excluded from further mortality analysis, as TH was not considered as treatment for non-comatose patients after OHCA.
First, we calculated the unadjusted risk ratio differences (RD) for favourable outcome (CPC 1–2) for both shockable and non-shockable groups according to the use of TH. Second, we performed an additional propensity analysis in patients with non-shockable rhythms to compare those treated with and without TH. We included age, coronary artery disease (yes/no), initial rhythm [asystole or pulseless electrical activity (PEA)], time to return of spontaneous circulation (ROSC), witnessed cardiac arrest (yes/no), bystander cardiopulmonary resuscitation (CPR) (yes/no) and inclusion site as variables in the backwards logistic regression analysis to evaluate independent factors predicting TH. We calculated a propensity score for TH for each patient and then categorized the patients into five groups according to the probability of TH. Thereafter, we performed a backwards logistic regression analysis to scrutinize independent factors associated with unfavourable outcome (CPC 3–4–5). We included the propensity score for TH, all the same pre-hospital variables as in a previous analysis for propensity score, APACHE II and use of TH in the analysis.
We considered p value <0.05 as significant and used SPSS 19.0 (SPSS Inc., Chicago, IL) for all statistical analysis.
Results
Study patients and incidence of OHCA
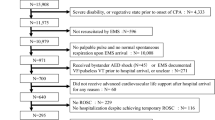
During the 1-year study period there were 17,540 admissions to the participating ICUs, among which cardiac arrest was recorded as the cause for ICU admission 829 (4.7 %) times. Of those 829 admissions, 572 (69.0 %) were OHCA patients. The final analysis comprised 504 unconscious adult OHCA patients (Fig. 1). The population-based incidence of OHCA treated in ICU was 13/100,000/year. A total of 311 patients (56.8 %) had a shockable initial rhythm (VF/VT), with incidence of 7.4/100,000/year. A total of 237 (43.2 %) patients presented with non-shockable rhythms (asystole or PEA), corresponding to incidence of 5.6/100,000/year. Initial rhythms and use of TH are shown in Fig. 1. Across participating hospitals, use of TH varied between 36 and 100 % of all unconscious OHCA patients (between 60 and 100 % with OHCA-VF) and hospital mortality varied between 18 and 71 % for individual ICUs. We found no correlation between the number of treated patients in ICU and hospital mortality.
Demographic, treatment and outcome data
Of 548 OHCA patients, 504 (92.0 %) were unconscious at ICU admission. These patients were included in final outcome analysis. The demographic, treatment and outcome data of all patients are summarized in Table 1, for patients with shockable rhythm in Table 2 and with non-shockable rhythm in Table 3. The length of stay (LOS) in the ICU was significantly longer in the TH group than in the non-TH group, for both shockable and non-shockable rhythms (3.2 versus 1.5 days, p < 0.001; Tables 2, 3).
Implementation of hypothermia
TH was induced in 311 unconscious patients, 241/281 (85.8 %) patients resuscitated from shockable rhythms (VF/VT) and 70/223 (31.4 %) patients from non-shockable rhythms (asystole/PEA). Hypothermia induction and maintenance was conducted with endovascular cooling devices in 247 (79.4 %) and surface cooling devices in 58 (18.6 %) cases. Five patients were cooled with other surface cooling methods and one patient with only ice-cold intravenous fluids. Ice-cold intravenous fluids were also used in 50 (16.1 %) patients as a start of induction in the pre-hospital setting or as an additional method to cooling devices. The target temperature was set to 33 °C in 300 (97 %) patients, and temperature of 32–34 °C was achieved in 111 (70–180) min from the start of hypothermia induction. The time for targeted temperature maintenance was 24 h in 231 (74.3 %) patients (range 0–47 h). The median (IQR) rewarming time from hypothermia to normal temperature was 9 (6–12) h.
Forty unconscious patients resuscitated from shockable rhythms (VF/VT) were treated without TH. Reasons for withholding TH are listed in the ESM (Table 4).
Outcome of unconscious patients with shockable rhythms (VF or VT)
Of 281 patients, 131 (46.6 %) had unfavourable neurological outcome (CPC 3–4–5) at 1 year (100 of 241 in TH and 31 of 40 in non-TH). The risk difference in unfavourable neurologic outcome (CPC 3–4–5) at 1 year was -35 % [95 % CI −50 to −21 %] (risk: 100 of 238 with TH versus 31 of 40 without TH).
Outcome of unconscious patients with non-shockable rhythms (asystole or PEA)
Of 223 patients, 180 (80.7 %) had unfavourable neurological outcome (CPC 3–4–5) at 1 year (54 of 70 in TH and 126 of 153 in non-TH). The unadjusted risk difference in unfavourable neurologic outcome (CPC 3–4–5) at 1 year was 54 of 67 with TH versus 126 of 150 without TH: difference −3 % [95 % CI −15 to +8 %]. Outcome data of all unconscious patients are shown in Fig. 2.
On backwards logistic regression analysis, unknown initial rhythm (p = 0.04) and absence of bystander CPR (p = 0.04) were the only variables negatively associated with use of TH. A propensity score adjusted mortality analysis revealed no difference in unfavourable neurological outcome (CPC 3–4–5) at 12 months in patients with non-shockable rhythms with or without TH [p = 0.819, odds ratio (OR) 1.16, 95 % CI 0.326–4.121]. On backwards logistic regression analysis, only higher APACHE II score (p = 0.002) and higher age (p = 0.008), but not site (p = 0.343), use of TH (p = 0.516), time to ROSC (p = 0.779), witnessed arrest (p = 0.332) or bystander CPR (p = 0.512), were independently associated with unfavourable CPC 3–4–5. ICU LOS and time of mechanical ventilation were both longer in patients treated with TH (p < 0.001).
Discussion
In this nationwide prospective cohort study we found that TH for OHCA patients resuscitated from VF/VT is well implemented in Finland. The neurological outcome at 1 year of TH-treated OHCA patients with shockable rhythm (58 % CPC 1–2) was equal to or better than in most previous studies [1, 2, 9, 20–22].
The overall incidence for OHCA has been reported to be 37/100,000/year in Europe [23]. The incidence of shockable rhythms (VF/VT) has been lower than non-shockable (asystole/PEA) rhythms in previous OHCA studies [11, 12, 23–25]. There is a large variation in the incidence of resuscitation attempts and successfully resuscitated OHCA patients between European countries, mainly because of differently structured emergency medical service (EMS) systems and different ways of reporting cardiac arrests [23, 26]. The population-based incidence of ICU-treated OHCA has not been calculated in previous studies. We found that the incidence of ICU-treated OHCA was 13/100,000/year in Finland. However, in the present study the incidence of ICU-treated patients with shockable rhythms (VF/VT) was 7.4/100,000/year and higher than that of non-shockable rhythms (asystole/PEA).
Hospital mortality of comatose OHCA patients resuscitated from shockable rhythms was 34 %, which was comparable to previous studies [21, 27, 28]. The majority (53 %) of these patients achieved good neurological recovery at 1 year (CPC 1–2). A high proportion (86 %) of unconscious patients in this OHCA group were treated with TH, and decisions to withhold TH were based on clinical grounds according to the current guidelines. This patient selection probably has a beneficial effect on outcome, and it may be one reason for the lower hospital mortality (28.6 %) in TH-treated patients with shockable rhythms compared with previous studies [1, 2, 9, 22]. Overall, TH is well implemented in post-resuscitation care in Finland [29].
Unexpectedly, TH was used in one-third of OHCA patients resuscitated from non-shockable rhythms. This is in disagreement with the national guidelines [30] but in broad agreement with the current international guidelines [3, 10]. Some Finnish intensivists had already decided to follow the most recent international guidelines, and thus they treated all OHCA patients admitted to ICU with TH, while most clinicians followed the previous guidelines and treated only OHCA patients with shockable rhythms with TH.
Although the hospital mortality and long-term survival of asystole or PEA patients are clearly worse than VF/VT patients, substantial proportions of these patients survive [31]. In this study almost a third of the patients survived to hospital discharge, and after 1 year 17 % achieved good neurological outcome (CPC 1–2). TH is a post-reperfusion intervention that might still improve neurological recovery in this patient group. It is irrelevant for the brain whether ischaemia and reperfusion result from a shockable or non-shockable rhythm. Ischaemic brain damage starts in a few minutes after cardiac arrest, and early started CPR is beneficial to outcome [32, 33]. Non-shockable rhythms often result from different and often serious clinical reasons. However, some patients develop asystole or PEA also after deterioration of VF over time. Obviously, patients with non-shockable initial rhythms represent a different patient population than patients with shockable rhythms. No RCT has focussed on this patient population, and therefore evidence of effect of TH in non-shockable rhythms in terms of better survival and better neurological performance is lacking.
We found no benefit of therapeutic hypothermia for the patients with non-shockable rhythms in crude or propensity-score-adjusted analyses, parallel to other cohort studies [9, 34, 35]. The recent study by Lundbye and colleagues [36] suggesting a benefit of TH in non-VF patients was retrospective and included also in-hospital cardiac arrests. Our results are in agreement with two recent studies [9, 37] concluding no benefit of TH in non-VF patients and a meta-analysis [38] concluding that TH is not associated with a significant difference in neurological outcome. Factors such as time to ROSC and bystander CPR seem to be more important among survivors from non-shockable rhythms than TH [39, 40]. In this study we found that only APACHE II and age were associated with unfavourable neurological outcome at 12 months in these patients. Our study does not support use of TH in patients resuscitated from non-shockable rhythms, because use of TH significantly increased ICU LOS and, therefore, overall costs of ICU/hospital treatment without any detected outcome benefit. Thus, an adequately powered RCT focussing on these patients is needed to scrutinize the possible benefit before wider use of TH in these patients.
In this study the number of OHCA patients treated in different ICUs varied from 2 to 74 patients/year. Similarly, the use of TH varied between 2 and 70 patients, corresponding to 32–100 % of all OHCA patients in each ICU. Hospital mortality varied between 18 and 71 % for individual ICUs. Of note, we found no correlation between ICU size or number of treated patients, and neurological outcome. Large variation of mortality and use of TH may be explained by differences in distances to hospital, patient selection and ICU resources across Finland. The decreasing incidence of VF [11] may paradoxically have increased the use of available TH in patients with non-shockable rhythms and diminished the number of patients with shockable rhythms.
To the best of our knowledge this study is the largest prospective multicentre cohort study in patients resuscitated from OHCA and treated with TH. Neurological outcome results were even better than in randomized controlled trials for VF/VT patients. However, there are some important limitations to our study. First, we cannot rule out that some patients who were successfully resuscitated were not treated in the ICUs. However, we performed a systematic follow-up in two university hospital areas covering approximately 40 % of the Finnish population. Based on these additional data from these two geographical jurisdictions, and the 98 % coverage of Finnish ICUs in the study, we consider our population representative. Second, due to the observational design, the use of TH in non-shockable patients was decided by the treating physician and not by randomization. Thus, patients treated with or without TH may have been different. Some patients were not admitted to ICUs, and even if admitted only those with a reasonable possibility of favourable outcome may have been treated with TH. Third, the sample size was not planned to detect any differences in outcome between TH- and non-TH-treated patients in the non-shockable group. However, based on the upper CI of the risk difference between those treated and not treated with TH, our findings suggest <15 % risk reduction with TH. Fourth, despite the propensity score matched analysis, there might have been some unknown confounding factors between the groups, and a bias is always possible in an observational study.
Conclusions
We conclude that TH in OHCA patients from shockable rhythms is widely implemented in Finland. Hospital and 90-day mortality and 1-year unfavourable neurological outcome of patients from shockable rhythms after TH were lower than in previous randomized controlled trials. However, our results do not support the use of TH in patients with non-shockable rhythms.
References
Hypothermia after Cardiac Arrest Study Group (2002) Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 346:549–556
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K (2002) Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 346:557–563
Nolan JP, Soar J, Zideman DA et al (2010) European resuscitation council guidelines for resuscitation 2010 section 1 executive summary. Resuscitation 81:1219–1276
Binks AC, Murphy RE, Prout RE et al (2010) Therapeutic hypothermia after cardiac arrest - implementation in UK intensive care units. Anaesthesia 65:260–265
Kremens K, Seevaratnam A, Fine J, Wakefield DB, Berman L (2011) Implementation of therapeutic hypothermia after cardiac arrest–a telephone survey of Connecticut hospitals. Conn Med 75:203–206
Oksanen T, Pettilä V, Hynynen M, Varpula T, Intensium Consortium study group (2007) Therapeutic hypothermia after cardiac arrest: implementation and outcome in Finnish intensive care units. Acta Anaesthesiol Scand 51:866–871
Wolfrum S, Radke PW, Pischon T, Willich SN, Schunkert H, Kurowski V (2007) Mild therapeutic hypothermia after cardiac arrest—a nationwide survey on the implementation of the ILCOR guidelines in German intensive care units. Resuscitation 72:207–213
Walters JH, Morley PT, Nolan JP (2011) The role of hypothermia in post-cardiac arrest patients with return of spontaneous circulation: a systematic review. Resuscitation 82:508–516
Dumas F, Grimaldi D, Zuber B et al (2011) Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients? Insights from a large registry. Circulation 123:877–886
Castren M, Silfvast T, Rubertsson S et al (2009) Scandinavian clinical practice guidelines for therapeutic hypothermia and post-resuscitation care after cardiac arrest. Acta Anaesthesiol Scand 53:280–288
Väyrynen T, Boyd J, Sorsa M, Määttä T, Kuisma M (2011) Long-term changes in the incidence of out-of-hospital ventricular fibrillation. Resuscitation 82:825–829
Kuisma M, Repo J, Alaspää A (2001) The incidence of out-of-hospital ventricular fibrillation in Helsinki, Finland, from 1994 to 1999. Lancet 358:473–474
Negovsky VA (1988) Postresuscitation disease. Crit Care Med 16:942–946
Nolan JP, Neumar RW, Adrie C et al (2008) Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A scientific statement from the international liaison committee on resuscitation; the American heart association emergency cardiovascular care committee; the council on cardiovascular surgery and anesthesia; the council on cardiopulmonary, perioperative, and critical care; the council on clinical cardiology; the council on stroke. Resuscitation 79(3):350–379
Castrén M, Nurmi J, Ikola K et al (2011) Resuscitation: Current Care guideline Summary. Working group appointed by the Finnish Medical Society Duodecim, the Finnish Resuscitation Council, the Finnish Society of Anaesthesiologists and the Finnish Red Cross. Helsinki: Finnish Medical Society Duodecim 127:1061–1063. Available on line at: http://www.kaypahoito.fi
Nolan JP, Deakin CD, Soar J, Böttiger BW, Smith G (2005) European resuscitation council guidelines for resuscitation 2005: section 4. adult advanced life support. Resuscitation 671(Supplement 1):S39–S86
Perttilä J, Hovilehto S (2010) Elvytetyn viilennyshoito. Ala-Kokko T, Perttilä J, Pettilä V, Ruokonen E et al. Tehohoito-opas. Kustannus Oy Duodecim, In
Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D (2004) Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American heart association, European resuscitation council, Australian resuscitation council, New Zealand resuscitation council, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation councils of Southern Africa). Circulation 110:3385–3397
Cummins RO, Chamberlain DA, Abramson NS, Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, Bossaert L, Delooz HH, Dick WF, Eisenberg MS et al (1991) Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style: a statement for health professionals from a task force of the American heart association, the European resuscitation council, the heart and stroke foundation of Canada, and the Australian resuscitation council. Circulation 84:960–975
Ferreira I, Schutte M, Oosterloo E, Dekker W, Mooi BW, Dambrink JH, van’t Hof AW (2009) Therapeutic mild hypothermia improves outcome after out-of-hospital cardiac arrest. Neth Heart J 17:378–384
Holzer M, Bernard SA, Hachimi-Idrissi S, Roine RO, Sterz F, Mullner M, Collaborative Group on Induced Hypothermia for Neuroprotection After Cardiac Arrest (2005) Hypothermia for neuroprotection after cardiac arrest: systematic review and individual patient data meta-analysis. Crit Care Med 33:414–418
Nielsen N, Hovdenes J, Nilsson F, Rubertsson S, Stammet P, Sunde K, Valsson F, Wanscher M, Friberg H (2009) Hypothermia Network. Outcome, timing and adverse events in therapeutic hypothermia after out-of-hospital cardiac arrest. Acta Anaesthesiol Scand 53:926–934
Atwood C, Eisenberg MS, Herlitz J, Rea TD (2005) Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation 67:75–80
Berdowski J, Berg RA, Tijssen JG, Koster RW (2010) Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 81:1479–1487
Nichol G, Thomas E, Callaway CW et al (2008) Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 300:1423–1431
Grasner JT, Herlitz J, Koster RW, Rosell-Ortiz F, Stamatakis L, Bossaert L (2011) Quality management in resuscitation–towards a European cardiac arrest registry (EuReCa). Resuscitation 82:989–994
Bro-Jeppesen J, Kjaergaard J, Horsted TI, Wanscher MC, Nielsen SL, Rasmussen LS, Hassager C (2009) The impact of therapeutic hypothermia on neurological function and quality of life after cardiac arrest. Resuscitation 80:171–176
Sunde K, Pytte M, Jacobsen D et al (2007) Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation 73:29–39
Reinikainen M, Oksanen T, Leppänen P, Torppa T, Niskanen M, Kurola J (2012) Mortality in out-of-hospital cardiac arrest patients has decreased in the era of therapeutic hypothermia. Acta Anaesthesiol Scand 56:110–115
Castren M, Silfvast T, Kurola J, Ikola K et al (2006) Resuscitation: Current Care guideline in Finnish. Working group appointed by the Finnish Medical Society Duodecim, the Finnish Resuscitation council, the Finnish society of Anaesthesiologists and the Finnishs Red Cross. Helsinki: Finnish Medical Society Duodecim
Dumas F, Rea TD (2012) Long-term prognosis following resuscitation from out-of-hospital cardiac arrest: role of aetiology and presenting arrest rhythm. Resuscitation 83:1001–1005
Adrie C, Cariou A, Mourvillier B et al (2006) Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur Heart J 27:2840–2845
Lund-Kordahl I, Olasveengen TM, Lorem T, Samdal M, Wik L, Sunde K (2010) Improving outcome after out-of-hospital cardiac arrest by strengthening weak links of the local Chain of Survival; quality of advanced life support and post-resuscitation care. Resuscitation 81:422–426
Martinell L, Larsson M, Bang A, Karlsson T, Lindqvist J, Thoren AB, Herlitz J (2010) Survival in out-of-hospital cardiac arrest before and after use of advanced postresuscitation care: a survey focusing on incidence, patient characteristics, survival, and estimated cerebral function after postresuscitation care. Am J Emerg Med 28:543–551
Oddo M, Ribordy V, Feihl F, Rossetti AO, Schaller MD, Chiolero R, Liaudet L (2008) Early predictors of outcome in comatose survivors of ventricular fibrillation and non-ventricular fibrillation cardiac arrest treated with hypothermia: a prospective study. Crit Care Med 36:2296–2301
Lundbye JB, Rai M, Ramu B, Hosseini-Khalili A, Li D, Slim HB, Bhavnani SP, Nair SU, Kluger J (2012) Therapeutic hypothermia is associated with improved neurologic outcome and survival in cardiac arrest survivors of non-shockable rhythms. Resuscitation 83:202–207
Storm C, Nee J, Roser M, Jörres A, Hasper D (2012) Mild hypothermia treatment in patients resuscitated from non-shockable cardiac arrest. Emerg Med J 29:100–103
Kim YM, Yim HW, Jeong SH, Klem ML, Callaway CW (2012) Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms? A systematic review and meta-analysis of randomized and non-randomized studies. Resuscitation 83:188–196
Sasson C, Rogers MA, Dahl J, Kellermann AL (2010) Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circulation Cardio Qual Outcom 3:63–81
Väyrynen T, Kuisma M, Määttä T, Boyd J (2008) Who survives from out-of-hospital pulseless electrical activity? Resuscitation 76:207–213
Acknowledgments
The authors acknowledge all the participants of the FINNRESUSCI study, especially the study doctors and nurses in the participating ICUs. We also thank Tieto Ltd, Helsinki for processing the database of the Finnish Intensive Care Consortium.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Preliminary results of this study were presented at the ESICM Annual Congress, Berlin, Germany 2011.
The members of the FINNRESUSCI Study Group are presented in the “Appendix”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The FINNRESUSCI Study Group: Participating hospitals, investigators (Inv.) and study nurses (SN.) in the FINNRESUSCI study.
Satakunta Central Hospital, Dr. Vesa Lund (Inv.), Päivi Tuominen, Satu Johansson, Pauliina Perkola, Elina Kumpulainen (SN.); East Savo Central Hospital, Dr. Markku Suvela (Inv.), Sari Hirvonen, Sirpa Kauppinen (SN.); Central Finland Central Hospital, Dr. Raili Laru-Sompa (Inv.), Mikko Reilama (SN.); South Savo Central Hospital, Dr. Heikki Laine (Inv.), Pekka Kettunen, Iina Smolander (SN.); North Carelia Central Hospital, Dr. Matti Reinikainen (Inv.), Tero Surakka (SN.); Seinäjoki Central Hospital, Dr. Kari Saarinen (Inv.), Pauliina Lähdeaho, Johanna Soini (SN.); South Carelia Central Hospi-tal, Dr. Seppo Hovilehto (Inv.); Päijät-Häme Central Hospital, Dr. Pekka Loisa (Inv.), Alli Parviainen, Pirjo Tuomi (SN.); Vaasa Central Hospital, Dr. Simo-Pekka Koivisto, Dr. Raku Hautamäki (Inv.); Kanta-Häme Central Hospital, Dr. Ari Alaspää (Inv.), Tarja Heikkilä (SN.); Lappi Central Hospital, Dr. Outi Kiviniemi (Inv.), Esa Lintula (SN.); Keski-Pohjanmaa Central Hospital, Dr. Tadeusz Kaminski (Inv.), Jane Roiko (SN.); Kymenlaakso Central Hospital, Dr. Seija Alila, Dr. Jussi Pentti (Inv.), Reija Koskinen (SN.); Länsi-Pohja´s Central Hospital, Dr. Jorma Heikkinen (Inv.) Helsinki University Hospital, Jorvi Hospital, Dr. Jukka Vaahersalo, Dr. Tuomas Oksanen, Dr. Tero Varpula (Inv.), Anne Eronen, Teemu Hult, Taina Nieminen (SN.); Meilahti Hospital Medical ICU, Dr. Tom Bäcklund (Inv.), Leevi Kauhanen (SN.); Meilahti Hospital ICU, Dr. Kirsi-Maija Kaukonen, Dr. Ville Pettilä (Inv.), Leena Pettilä, Sari Sutinen (SN.); Turku University Hospital, Dr. Juha Perttilä, Dr. Keijo Leivo, Dr. Juha Grönlund (Inv.); Tampere University Hospital, Dr. Sanna Hoppu, Dr. Jyrki Tenhunen, Dr. Sari Karlsson (Inv.), Atte Kukkurainen, Simo Varila, Samuli Kortelainen, Minna-Liisa Peltola (SN.); Kuopio University Hospital, Dr. Pamela Hiltunen, Dr. Jouni Kurola, Dr. Esko Ruokonen (Inv.), Elina Halonen, Saija Rissanen, Sari Rahikainen (SN.); Oulu University Hospital, Dr. Risto Ahola, Dr. Tero Ala-Kokko (Inv.), Sinikka Sälkiö (SN.)
Rights and permissions
About this article
Cite this article
Vaahersalo, J., Hiltunen, P., Tiainen, M. et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med 39, 826–837 (2013). https://doi.org/10.1007/s00134-013-2868-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2868-1