Abstract
Purpose
Our aim was to compare adaptive support ventilation with and without closed loop control by end tidal CO2 (ASVCO2, ASV) with pressure (PC) and volume control ventilation (VC) during simulated clinical scenarios [normal lungs (N), COPD, ARDS, brain injury (BI)].
Methods
A lung model was used to simulate representative compliance (mL/cmH2O): resistance (cmH2O/L/s) combinations, 45:5 for N and BI, 60:7.7 for COPD, 15:7.7 and 35:7.7 for ARDS. Two levels of PEEP (cmH2O) were used for each scenario, 12/16 for ARDS, and 5/10 for others. The CO2 productions of 2, 3, 4 and 5 mL/kg predicted body weight/min were simulated. Tidal volume was set to 6 mL/kg during VC and PC. Outcomes of interest were end tidal CO2 (etCO2) and plateau pressure (P Plat).
Results
EtCO2 levels in N and BI and COPD were similar for all modes. In ARDS, etCO2 was higher in ASVCO2 than in other modes (p < 0.001). Under all mechanical conditions ASVCO2 revealed a narrower range of etCO2. P Plat was similar for all modes in all scenarios but ARDS where P Plat in ASV and ASVCO2 were lower than in VC (p = 0.001). When P Plat was ≥28 cmH2O, P plat in ASV and ASVCO2 were lower than in VC and PC (p = 0.024).
Conclusion
All modes performed similarly in most cases. Minor differences observed were in favor of the closed loop modes. Overall, ASVCO2 maintained tighter CO2 control. The ASVCO2 had the greatest impact during ARDS allowing etCO2 to increase and protecting against hypocapnia evident with other modes while ensuring lower P plat and tidal volumes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adaptive support ventilation (ASV) is a form of pressure targeted closed loop ventilation, designed to optimize the relationship between tidal volume and respiratory frequency based on lung mechanics as predicted by Otis [1]. Adaptive support ventilation provides a ventilatory pattern that minimizes the work of breathing (WOB) and auto positive end expiratory pressure (autoPEEP or intrinsic PEEP) while limiting peak airway pressure. ASV automatically determines the tidal volume (V T) and respiratory rate (RR) that best maintains the peak pressure below the target level and minimal WOB [2].
Recently we demonstrated in a lung model that ASV was better able to maintain plateau pressures (P Plat) <28 cmH2O than a fixed tidal volume of 6 mL/kg during volume controlled ventilation (VC) [3]. In that evaluation ASV varied V T between 2.9 and 9.0 mL/kg, however, when V T fell below its lower limit of 4.3 mL/kg the ventilator alarmed notifying us of the marked reduction. The algorithm used by the ASV mode considered lung mechanics in its adjustment; no reference to gas exchange was incorporated. Recently, a new algorithm for ASV has added closed loop control of etCO2 in parallel to the current closed loop control by lung mechanics (ASVCO2).
In this study, our aim was to compare the performance of ASV and ASVCO2 to that of pressure control ventilation (PC) and VC during simulated normal lungs, ARDS, COPD, and brain injury scenarios and to compare the ability of all modes to maintain P Plat below a set target as respiratory mechanics and CO2 production varied. Our hypothesis was that ASVCO2 would maintain etCO2 within a normal range predefined for specific conditions compared to levels achieved using other ventilator modalities, delivering clinically acceptable tidal volumes whilst avoiding clinically significant hypocapnia or hypercapnia across a range of respiratory mechanics, PEEP, minute ventilation and CO2 production levels. Further, that ASVCO2 will achieve this outcome with peak pressure plateaus less than a target pressure of 28 cmH2O. This pressure was chosen based on the recommended maximum plateau pressure in the ARDSnet protocol [4].
Materials and methods
Experimental setup
The Michigan Instruments Dual Adult Training/Test Lung (Model 1600 Michigan Instruments Inc., MI, USA) with CO2 titrated into one of the test lung chambers was utilized throughout the study. The Galileo Ventilator (Galileo) (Hamilton Medical, Bonaduz, Switzerland) was used for ASV, VC and PC modes and a modified Hamilton G5 Ventilator (G5) (Hamilton Medical, Bonaduz, Switzerland) was used for ASVCO2. Disease specific algorithms in the G5 were used for the specific simulated lung mechanics scenarios. These algorithms included ‘Normal Lungs’, ‘ARDS’, ‘COPD’, and ‘Brain Injury’ states. One chamber of the Michigan Instruments test lung was passively ventilated during all modes. The Hamilton Medical standard adult circuit was used with both ventilators. The study was conducted without the inclusion of an active humidifier to avoid water contamination in the lung model. The lung model was directly connected to the circuit wye; no endotracheal tube was included.
Ventilation strategies
In all ventilator modes inspiratory time was set at 0.8 s. The target minute volume (MV) was set either to 100, 150 or 200 % of predicted healthy normal MV of 0.1 L/kg predicted body weight (PBW) [5] for a 70 kg PBW individual during ASV, VC and PC (Table 1). The flow waveform in VC was square and peak flow was set to insure that active delivery of the V T occurred over the entire inspiratory time. In PC, the ventilating pressure was set to result in a V T of 6 mL/kg. ASV determined the respiratory rate and tidal volume based on its algorithms. The pressure limit alarm was set at 38 cmH2O (10 cmH2O higher than the desired peak pressure) in ASV and ASVCO2 to insure that peak pressure was maintained ≤28 cmH2O. The ventilators maintained a 10 cmH2O window of pressure above the target pressure where alarms were activated if pressure exceeds the target level.
Lung model settings
Measurements were obtained during simulation of four different clinical scenarios for mechanical ventilation including the normal lung, ARDS, COPD and brain injury. For each scenario, combinations of lung model compliance, resistance, target minute volume, PEEP, and CO2 production rate were applied as defined in Table 1. Compliance and resistance settings were based on typical lung mechanics reported in normal lung conditions, patients with severe ARDS/acute lung injury and with COPD [4, 6–11]. For VC, PC and ASV, this approach resulted in 16 unique testing conditions for the normal lung and COPD, and 32 unique testing conditions for the ARDS scenarios. During ASVCO2, MV was auto-adjusted by the ventilator according to the scenario-specific algorithm and the etCO2. Therefore, in this mode, there were eight unique testing modes for the normal lung and COPD, and 16 unique combinations for the ARDS scenarios. For the brain injury scenario, ventilatory settings and conditions were those of a normal lung. Therefore, simulations were only performed for eight unique conditions during ASVCO2 using the brain-injury algorithm.
Variables evaluated
The following variables were recorded during all modes of ventilation: P Plat, RR, V T, MV, etCO2 and autoPEEP. RR, V T, and MV, all were obtained directly from the ventilator display. The P Plat was assumed equal to end inspiratory pressure during ASV, ASVCO2 and PC and determined by establishing a >1.0 s end inspiratory pause during VC for a single breath after steady state was established. The P Plat was obtained directly from the ventilator display. AutoPEEP was read directly off the ventilator and verified by observing the lung model end expiratory pressure. The primary performance variable used to compare modes was etCO2 and the secondary performance variables were the number of test scenarios in which the P Plat was >28 cmH2O, the V T was outside of the 4–8 mL/kg range and the development of autoPEEP.
Data analysis and statistics
Data were expressed as median (25–75th percentile) or mean (±SD). Statistical analyses were performed with the Kruskal–Wallis or ANOVA tests depending on the data distribution using SPSS software (Statistical Package for the Social Sciences, version 15.0; SPSS Inc.; Chicago, IL). Post hoc analyses were performed using Bonferoni correction. The test of homogeneity of variances (Levene’s test) was used to compare group variances. A p value < 0.05 was considered statistically significant.
Results
Normal lung and brain injury scenarios
In normal lung (N) and brain injury (BI) settings, V T in ASV and ASVCO2 were higher than in VC and PC (p < 0.001) (Table 2). P Plat, etCO2 (both variables presented in figures—online resources 1 and 2) and RR (Table 3) were similar for all modes, but the etCO2 levels in ASVCO2 demonstrated a narrower distribution (interquartile range: 3 for N and 1.75 for BI settings, p ≤ 0.01) compared to the greater variance in other modes (interquartile ranges: 22.75, 22, 21.75 for ASV, VC, PC) (Online resources 1 and 2). No P Plat ≥28 cmH2O were detected and PEEP did not affect results.
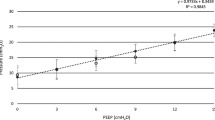
ARDS scenarios
In ASVCO2 etCO2 was higher than in other modes (p < 0.001) (Fig. 1). V T was higher in VC than in PC (p < 0.001) (Table 2). P Plat was higher in low compliance than high compliance within each ventilation mode (p < 0.01) (Fig. 1). In low compliance, P Plat was significantly higher in VC and PC when compared to ASVCO2 and ASV (p < 0.001). Across all evaluations, RR was similar in all modes, however, for ASVCO2 and ASV modes (Table 3), RR in low compliance scenarios was higher than RR in high compliance scenarios (p < 0.001).
End tidal CO2 (a) and plateau pressure (b) levels in ARDS settings. ARDS acute respiratory distress syndrome, ASVCO 2 adaptive support ventilation with closed loop CO2 control, ASV adaptive support ventilation, VC volume control ventilation, PC pressure control ventilation et CO 2 end tidal carbon dioxide, P Plat plateau pressure. a *p < 0.05 versus etCO2 in ASV, VC, PC, # p < 0.05 versus etCO2 in VC, PC. b *p < 0.05 versus P Plat in ASVCO2, ASV, # p < 0.05 versus P Plat in ASV
ARDS scenarios where P Plat ≥ 28 cmH2O
When P Plat was ≥28 cmH2O etCO2 in ASVCO2 was higher than in VC and PC (p < 0.001) (Fig. 2). The V T in VC was higher than V T in other ventilation modes (p < 0.05) (Table 2). In low compliance, V T in ASV and ASVCO2 were lower than V T in VC and PC (p < 0.001) and V T in VC was lower than in PC (p < 0.001) (Table 2). P Plat in ASV and ASVCO2 were lower than in PC (p < 0.05) (Fig. 2). In addition, P Plat in ASV was lower than in VC (p < 0.05). P Plat in ASVCO2 also trended to be lower than in VC but this was not a statistically significant difference (p = 0.055). With low compliance, P Plat in ASVCO2 was the lowest and P Plat in VC was the highest (p < 0.01). The RR (breaths/min) was higher in ASV when compared to VC and PC (p = 0.008) (Table 3). For ASVCO2 and ASV modes, RR in low compliance was higher than RR in high compliance. In low compliance, RR in ASV was higher than both VC and PC (p < 0.001). In high compliance, RR in ASVCO2 was lower than both VC and PC (p = 0.002).
End tidal CO2 (a) and plateau pressure (b) levels in ARDS settings where plateau pressures were equal or greater than 28 cmH2O. ARDS acute respiratory distress syndrome, ASVCO 2 adaptive support ventilation with closed loop CO2 control, ASV adaptive support ventilation, VC volume control ventilation, PC pressure control ventilation, etCO 2 end tidal carbon dioxide, P Plat plateau pressure. a # p < 0.05 versus etCO2 in VC, PC. b *p < 0.05 versus P Plat in ASV, # p < 0.05 versus P Plat in ASV and ASVCO2, ∞ p < 0.05 versus P Plat in other modes
COPD scenarios
In all ventilation modes etCO2 were similar, although etCO2 in ASVCO2 tended to be higher than in other modes (Fig. 3). The V T in ASV and ASVCO2 were higher than VC and PC (p < 0.001) (Table 2). The V T in ASV and ASVCO2 were higher than VC and PC for both PEEP levels (Table 2). The P Plat was similar for all modes. No P Plat ≥28 cmH2O were detected in any scenario (Fig. 3). The RR in ASVCO2 were lower than in VC and PC (p = 0.003) (Table 3).
End tidal CO2 (a) and plateau pressure (b) levels were similar across all ventilation modes in COPD settings. COPD chronic obstructive pulmonary disease, ASVCO 2 adaptive support ventilation with closed loop CO2 control, ASV adaptive support ventilation, VC volume control ventilation, PC pressure control ventilation, etCO 2 end tidal carbon dioxide, P Plat plateau pressure. *p < 0.05 versus P Plat in ASV and ASVCO2. # p < 0.05 versus P Plat in PC
AutoPEEP levels were similar among all modes not exceeding 0.5 cmH2O in COPD, 1 cmH2O in normal and brain injury and 2 cmH2O in ARDS scenarios.
Discussion
Our findings can be summarized as follows: (1) In normal lung and brain injury, ASV, ASVCO2, VC and PC performed similarly. (2) In COPD scenarios, V T were higher and RR lower in ASV and ASVCO2 compared to VC and PC. (3) In ARDS scenarios, etCO2 in ASVCO2 was higher than in other modes and V T and P Plat were lower than other modes. (4) The ASVCO2 performed as expected but seemed to only have a major effect when compared specifically to ASV in ARDS scenarios.
The new algorithm for adaptive support ventilation (ASVCO2; currently available as IntelliVent® in Europe) is designed to keep etCO2 in a defined range by adjusting target MV based on input from the user and measured parameters [12]. Total RR and etCO2 are measured and patient gender, height, type of lung disease, the presence of brain injury, severity of lung injury and pressure limit are set by the user. Based on these factors, a target MV is calculated by the CO2 controller. Using the minimal work of breathing principle (Otis Equation) [1], a target V T and RR are then determined by the ASV controller. Acceptable etCO2 ranges depend on patient’s lung disease state, calculated as 2 × [Pinsp(cmH2O) + PEEP(cmH2O)] and treatment options. That is, if the patient has severe lung injury, permissive hypercapnia is allowed; if the patient is at the weaning stage limits are increased by 5 mmHg; if the patient has chronic hypercapnia, ranges are shifted by +10 mmHg; if the patient has brain injury the limits are 33 mmHg (minimum) and 38 mmHg (maximum) regardless of the lung conditions. The key to the optimal performance of this algorithm is does the etCO2 accurately reflect PaCO2 in the specific patient? This must be determined in clinical trials. In addition, very low V T in ARDS can lead to progressive atelectasis, as a result, careful adjustment of applied PEEP to stabilize the lung and avoid tidal recruitment is required.
To our knowledge, this study is the first to evaluate performance of the ASVCO2 algorithm in different disease settings and to compare it with ASV, PC and VC. In normal lungs with or without brain injury, all modes performed similarly. The brain injury algorithm [12] ensures strict low normocapnia while limiting airway pressures but did not alter the ventilatory parameters compared with other modes due to the normal lung settings. We cannot, however, predict the combined effects of head injury plus ARDS. The manufacturer indicates the brain injury algorithm overrides all other disease algorithms.
In COPD scenarios, ASVCO2 kept the etCO2 level at 47 ± 3.8 mmHg while other modes averaged around 39–42 mmHg with larger standard deviations (12–14 mmHg). Although this tendency did not show a statistically significant difference, it may be of importance when considered for clinical use in patients with chronic hypercapnia. As P Plat remained similar in all modes, V T was higher in ASV and ASVCO2. This finding for ASV was consistent with previous laboratory and observational clinical studies [13–16], howeve, the maximum tidal volume we found was 8.1 mL/kg for ASVCO2 and 8.25 mL/kg for ASV as opposed to much higher values (10–22 mL/kg) observed in previous studies [15, 16]. Large V T in COPD were attributed to the longer expiratory time constant. In our study, the V Ts were very similar to those of normal lungs (C: 45 mL/cmH2O, R: 5 cmH2O/L/s). This finding is partly because we used only one set of lung mechanics for COPD (C: 60 mL/cmH2O, R: 7.7 cmH2O/L/s).
In ARDS scenarios, the ASVCO2 algorithm resulted in permissive hypercapnia as recommended by many to maintain a lung protective ventilation strategy [4, 6, 17–19]. Permissive hypercapnia although not a desired outcome during ventilatory support does allow a decrease in V T and P Plat as well as a shifting of the oxyhemoglobin dissociation curve to the right unloading more oxygen to the tissue. In addition, at least laboratory data indicates cell survival is enhanced during hypercarbia versus normocarbia [20]. Most importantly it does not cause any adverse response provided it is achieved gradually and the patient does not have significant heart or kidney disease or a metabolic acidosis [4, 6, 17–19]. Overall, tidal volumes in all modes were comparable to the NIH ARDSnet protocol [4] (4–8 mL/kg) except for the few scenarios where the P Plat exceeded 28 cmH2O. Theoretically, the lower limit for tidal volume in ASV and ASVCO2 is 4.4 mL/kg which equals two times the anatomical dead space (2.2 mL/kg), however when the P Plat limit was reached (28 cmH2O) V T decreased further. Since we used a lung model and not a live animal model or patients, we were unable to evaluate the effect that proper setting of PEEP would have on the operation of ASVCO2 or ASV. If the lung was recruited and PEEP set to avoid derecruitment, it is reasonable to expect that compliance would improve and the decrease in V T may have been minimized [21]. Proper PEEP adjustment would also minimize the increase in P Plat noted in VC and PC.
P Plat were significantly higher in PC and VC than in ASVCO2 and ASV with ARDS. In cases where the P Plat was ≥28 cmH2O, V T in ASVCO2 and ASV ranged between 3.2 and 6.5 mL/kg (median: 4.2) and 3.4–7.3 mL/kg (median: 4.4), respectively. The number of scenarios where the V T was lower than 4 mL/kg was 4 (50 %) in ASVCO2 and 8 (50 %) in ASV (Table 4). In these settings alarms identified the low V T. The overriding goal of ASVCO2 or ASV in ARDS is to minimize the development of lung injury (volutrauma or barotrauma) [4, 22]. This goal is accomplished by attempting to maintain ventilation within the ARDSnet defined tidal volume and P Plat targets [4]. As described in the ARDSnet protocol as P Plat increases the tidal volume needs to be decreased.
The findings of this study highlight the potential benefit of closed loop ventilatory control. This potential benefit may be directly related to the ability of ASVCO2 and ASV to allow variability in MV, RR and V T which normally occurs as lung mechanics changes. We may discover soon that this variability may be one of the most important benefits of these types of modes of ventilation [23].
Limitations
There are a number of limitations to the current study: (1) this is a simulation study, thus the data obtained from this study can not be directly extrapolated to patients. However the use of a simulator allowed us to precisely define the lung mechanics for each disease setting and identify the precise responses for each ventilation mode and algorithm. (2) A one compartment lung model was used which does not reflect the complexities of a multi-compartmental lung. (3) As only passive ventilation was simulated, we can not predict how these modes will work during active ventilation. (4) The complete range of lung mechanism settings in COPD and ARDS was not evaluated; there are many different C:R combinations for these specific conditions. As a result we cannot be sure how these algorithms will respond under all possible scenarios. (5) In ASVCO2 the CO2 algorithm overrides lung mechanics. The impact of this in brain injury and COPD or ARDS is not defined by this study. (6) We did not directly measure P Plat during ASVCO2, ASV and PC but used the end inspiratory pressure as a reflection of P Plat. In scenarios where flow did not return to zero at the end of the breath, P Plat. was overestimated. However, in most scenarios flow was close to zero at the termination of these pressure targeted breaths. (7) The lung model was directly connected to the wye connection of the circuit without an endotracheal tube. Therefore the resistance of an endotracheal tube may have affected the delivery of the tidal volume in PC, ASV and ASVCO2 modes.
Conclusion
ASVCO2, ASV, PC and VC performed similarly in most cases. The minor differences observed were in favor of the closed loop mechanisms. Overall, ASVCO2 maintained tighter CO2 control in all scenarios. ASVCO2 had the greatest impact during ARDS; ASVCO2 allows etCO2 to increase, resulting in greater hypercapnia and lower V T and plateau pressure than ASV, VC or PC.
References
Otis AB (1954) The work of breathing. Physiol Rev 34:449–458
Thompson BT, Hayden D, Matthay MA, Brower R, Parsons PE (2001) Clinicians’ approaches to mechanical ventilation in acute lung injury and ARDS. Chest 120:1622–1627
Sulemanji D, Marchese A, Garbarini P, Wysocki M, Kacmarek RM (2009) Adaptive support ventilation; an appropriate mechanical ventilation strategy for the acute respiratory distress syndrome? Anesthesiology 111:863–870
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Eng J Med 342:1301–1308
Johannigman JA, Muskat P, Barnes S, Davis K, Branson RD (2008) Autonomous control of ventilation. J Trauma 64:S302–S320
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective ventilation strategy on mortality in the acute respiratory distress syndrome. N Eng J Med 338:347–354
Bernasconi M, Ploysongsang Y, Gottfried SB, Milc-Emily C, Rossi A (1998) Respiratory compliance and resistance in mechanically ventilated patients with acute respiratory failure. Intensive Care Med 14:547–553
Kallet RH, Hemphill J, Dicker RA, Alonso JA, Campbell AR, MacKersie RC, Katz JA (2007) The spontaneous breathing pattern and work of breathing of patients with acute respiratory distress syndrome and acute lung injury. Resp Care 52:989–995
Nunes S, Balta P, Takala J (2006) Changes in respiratory mechanics and gas exchange during the acute respiratory distress syndrome. Acta Anesthesiol Scand 50:80–91
Yang SC, Yang SP (2002) Effects of inspiratory flow waveforms on lung mechanics, gas exchange, and respiratory metabolism in COPD patients during mechanical ventilation. Chest 122:2096–2104
Tsukino M, Nishimura K, Ikeda A, Koyama H, Mishima M, Izumi T (1996) Physiologic factors that determine the health related quality of life in patients with COPD. Chest 110:896–903
Hamilton Medical AG (2009) Detail specifications ventilation controller, Switzerland, Doc No: E40015, version: 1.16: 7–14
Arnal JM, Wysocki M, Nafati C, Donati S, Granier I, Corno G, Durand-Gasselin J (2008) Automatic selection of breathing pattern using adaptive support ventilation. Intensive Care Med 34:75–81
Cassina T, Chiolero R, Mauri R, Revelly JP (2003) Clinical experience with adaptive support ventilation for fast-track cardiac surgery. J Cardiothorac Vasc Anesth 17:571–575
Veelo DP, Dongelmans DA, Binnekade JM, Paulus F, Schultz MJ (2010) Adaptive support ventilation: evaluating the size of delivered tidal volumes. Int J Artif Organs 33:302–309
Iotti GA, Polito A, Belliato M, Pasero D, Beduneanu G, Wysocki M, Brunner J, Braschi A, Brochard L, Mancebo J, Ranieri VM, Richard JC, Slutsky AS (2010) Adaptive support ventilation versus conventional ventilation for total ventilatory support in acute respiratory failure. Intensive Care Med 36:1371–1379
Hickling KG, Walsh J, Henderson S, Jackson R (1994) Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med 22:1568–1578
Bidani A, Tzouanakis AE, Cardenas VJ Jr, Zwischenberger JB (1994) Permissive hypercapnia in acute respiratory failure. JAMA 272:957–962
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med 34:17–60
Laffey JG, Honan D, Hopkins N, Hyvelin JM, Boylan JF, McLoughlin P (2004) Hypercapnic acidosis attenuates endotoxin-induced acute lung injury. Am J Respir Crit Care Med 169:46–56
Suarez-Sipmann F, Bohm SH, Tusman G, Pesch T, Thamm O, Reismann H, Reske A, Magnusson A, Hedenstierna G (2007) Use of dynamic compliance for open lung positive end expiratory pressure titration in an experimental study. Crit Care Med 35:214–221
Dreyfuss D, Saumon G (1992) Barotrauma is volutrauma, but which volume is the one responsible? Intensive Care Med 18:139–141
Kacmarek RM, Villar J (2011) When it comes to ventilation noisy is better than quiet and variability is healthier than constant! Crit Care Med 39:898–899
Acknowledgments
Funding in part for this study was provided by Hamilton Medical.
Conflicts of interest
Dr. Kacmarek has received research grants from Covidien and Hamilton Medical, an honorarium for lecturing from Maquet and Hamilton, and is a consultant for Newport Medical, KCI and Bayer. Dr. Wysocki is a full time employee of Hamilton Medical.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sulemanji, D.S., Marchese, A., Wysocki, M. et al. Adaptive support ventilation with and without end-tidal CO2 closed loop control versus conventional ventilation. Intensive Care Med 39, 703–710 (2013). https://doi.org/10.1007/s00134-012-2742-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2742-6