Abstract
Purpose
To analyze prognostic factors associated with in-hospital cardiac arrest (CA) in children.
Methods
A prospective, multicenter, multinational, observational study was performed on pediatric in-hospital CA in 12 countries and included 502 children between 1 month and 18 years. The primary endpoint was survival at hospital discharge. Univariate and multivariate logistic regression analyses were performed to assess the influence of each factor on mortality.
Results
Return of spontaneous circulation was achieved in 69.5 % of patients; 39.2 % survived to hospital discharge and 88.9 % of survivors had good neurological outcome. The pre-arrest factors related to mortality were lower Human Development Index [odds ratio (OR) 2.32, 95 % confidence interval (CI) 1.28–4.21], oncohematologic disease (OR 3.33, 95 % CI 1.60–6.98), and treatment with inotropic drugs at the time of CA (OR 2.35, 95 % CI 1.55–3.56). CA and resuscitation factors related to mortality were CA due to neurological disease (OR 5.19, 95 % CI 1.49–18.73) and duration of cardiopulmonary resuscitation greater than 10 min (OR 4.00, 95 % CI 1.49–18.73). Factors related to survival were CA occurring in the pediatric intensive care unit (PICU) (OR 0.38, 95 % CI 0.16–0.86) and shockable rhythm (OR 0.26, 95 % CI 0.09–0.73).
Conclusions
In-hospital CA in children has a low survival but most of the survivors have a good neurological outcome. Some prognostic risk factors cannot be modified, making it important to focus efforts on improving hospital organization to care for children at risk of CA in the PICU and, in particular, in other hospital areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the advances in prevention, training in cardiopulmonary resuscitation (CPR), and early treatment of cardiac arrest (CA), mortality after CA in children remains very high [1–14]. Out-of-hospital and in-hospital CA in children can have different etiologies, resuscitation characteristics, prognosis, and clinical course [1–14].
There are few prospective studies that have analyzed the causes and risk factors that influence the prognosis of in-hospital CA in children. All of them have been performed in only one country (most with the same database of patients) and they have used different criteria of CA and resuscitation [4, 6–8, 10, 13]. Previous studies have shown that survival varies depending on the site of arrest, underlying disease, initial electrocardiographic (ECG) rhythm, and the duration of CPR [1–14].
However, there are no multicenter, multinational, prospective studies on CA in children that have included countries with distinct socioeconomic and healthcare levels. The objective of the present study was to analyze the factors affecting mortality and neurological outcome of in-hospital CA in children.
Patients and methods
An open, multicenter, prospective study was designed and information and an invitation to participate were sent to the pediatric departments and pediatric intensive care units (PICU) of hospitals of Latin American countries, Spain, Portugal, and Italy. The study was approved by local institutional review boards. Registration on the website http://www.pcrpediatrica.com was necessary to participate in the study.
A protocol was drawn up in accordance with the Utstein style guidelines [15, 16]. Children aged from 1 month to 18 years who suffered in-hospital CA between December 2007 and December 2009 were included. CA was defined as unresponsiveness, apnea, absence of signs of life, and absence of a palpable central pulse or bradycardia of less than 60 bpm with poor perfusion in infants, requiring external cardiac compressions and assisted ventilation.
All data were entered via a secure, encrypted website and were electronically submitted to the coordinating center. That center performed a review to ensure data quality, and site investigators were queried to complete missing data and resolve discrepancies.
The following variables were included: patient-related variables (age, sex, weight, cause of the arrest, existence of a previous arrest, family and personal background); and arrest and life support-related variables (type of arrest, hospital area where arrest occurred, monitored variables, assisted ventilation, vasoactive drugs administered before the arrest, time elapsed from onset of arrest to initiation of CPR maneuvers and procedures performed during resuscitation, initial ECG rhythm, total duration of CPR, hospital course, and clinical and neurological status at hospital discharge according to the Pediatric Cerebral Performance Category (PCPC) and Pediatric Overall Performance Category (POPC) scales [17]). Variable definitions were based on Utstein style guidelines [15, 16].
The Gross National Income (GNI), Human Development Index (HDI), and infant and under-5 mortality of each country were calculated from data published by the World Bank [18], World Heath Organization (WHO) [19], and Human Development Reports [20] during the study years. Countries were divided into low, medium, medium–high, and high GNI per capita using the Atlas conversion factor (GNI national currency to the US dollar/midyear population for year) [18]. The HDI is a composite index measuring average achievement in three basic dimensions of human development—a long and healthy life, knowledge, and a decent standard of living. Countries are classified as very high, high, medium, or low HDI. Infant mortality and mortality in children under 5 years were classified as low (<10/1,000 live births in the same year), medium (10–20/1,000 live births), and high (>20/1,000 live births) [19].
The primary endpoint was survival at hospital discharge. The secondary outcome measure was neurological status at hospital discharge; a good neurological status was defined as a PCPC score of 1 or 2 [17].
Statistical analyses were conducted using SPSS software version 18.1 (SPSS Inc, Chicago, IL, USA). Outcomes were compared between groups using the χ2 test or Fisher’s exact test for categorical variables. Univariate and multivariate logistic regression analyses were performed to assess the influence of each one of the factors on mortality. Two logistic regression models were constructed including variables available before and during the arrest. All individual factors with statistical significance in the univariate analysis and P < 0.1 were eligible for inclusion in the logistic regression model. Adjusted odds ratios (OR) and 95 % confidence intervals (CI) were calculated for each model. A P value less than 0.05 was considered significant.
Results
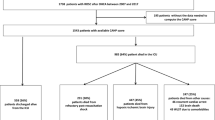
Forty-eight hospitals from 12 countries participated in the study. The analysis included 563 episodes of in-hospital CA in 502 patients. The flow diagram of the clinical course of patients is shown in Fig. 1. Return of spontaneous circulation (ROSC) was achieved in 349 patients (69.5 %), but 152 (30.3 %) patients died later in hospital. A total of 197 (39.2 %) survived to hospital discharge (Fig. 1).
Characteristics of countries, patients, and pre-arrest clinical state
The characteristics of the patients and the countries and their relationship with survival at hospital discharge (univariate analysis) are summarized in Table 1. As the three social indicators are almost identical we have only included the HDI score.
The mean age was 44.7 ± 58.5 months (range 1 month–18 years) and the mean weight was 15.2 ± 16.2 kg (range 1–93 kg). The majority of patients were boys and they presented a lower mortality than girls. Children weighing less than 10 kg presented a lower mortality, but in the multivariate analysis neither age nor weight were found to be significant risk factors for mortality.
Four hundred and three patients (80.3 %) had underlying diseases. In the multivariate regression analysis only children with oncohematologic diseases presented a higher mortality than the rest of children (Table 2).
Pre-arrest POPC and PCPC scores were available in 323 patients (64.3 %) and 96.7 % of those patients had a good pre-arrest neurological status (PCPC score 1 or 2). As the POPC and PCPC scores were nearly identical in all patients, only the PCPC scores are shown. The pre-arrest PCPC score was not related to survival in the multivariate analysis.
At the time of onset of CA, 76.1 % patients were being monitored, 55.2 % were on mechanical ventilation, and 40.4 % were receiving vasoactive drugs. No differences in mortality were detected on comparing monitored or ventilated patients with those not monitored or ventilated. In contrast, patients who were receiving vasoactive drugs at the time of CA had a significantly higher mortality than that those who were not receiving such treatments.
Patients from European countries had a significant lower mortality than those from Latin American countries. There was also a lower mortality among children from very high and high HDI countries than among those from medium HDI countries.
In the multivariate logistic regression analysis (Table 2) the factors related to mortality were lower HDI, oncohematologic disease, and treatment with inotropic drugs at the time of onset of CA.
Characteristics of cardiac arrest and resuscitation
Table 3 summarizes the characteristics of the CA and of resuscitation and the relationship with survival at hospital discharge (univariate analysis).
Cardiac and respiratory diseases and sepsis were predominant causes of CA. Mortality due to CA in patients with sepsis or neurological disease was higher than that of CA in patients with other underlying diseases.
CA occurred in the PICU in 50 % of cases, in the emergency department (ED) in 26.8 %, and in other hospital areas in 23.2 %. Mortality due to CA occurring in the ED was higher than that of CA occurring in any other hospital area.
An ECG was recorded at the onset of the arrest in 432 (86 %) patients. Asystole and bradycardia were the most frequent rhythms. Ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) was present only in 6 % of the cases. Mortality was higher in those patients who presented asystole than in those presenting any other rhythm.
Resuscitation was initiated in less than 4 min in most patients. This could explain why there were no differences in mortality according to the delay in the initiation of resuscitation efforts.
Analysis of the relationship between mortality and each one of the life support procedures performed revealed that mortality was higher in children who required epinephrine, bicarbonate administration, or volume expansion (Table 3). The non-ROSC and in-hospital death rates increased as the duration of CPR increased (P < 0.001) (Fig. 2).
Mortality among the 109 children with more than one episode of CA (63.3 %) was slightly higher than that of patients with only one episode of CA (60.5 %), P = 0.66.
Multivariate logistic regression analysis (Table 4) found that underlying neurological disease and duration of CPR more than 10 min were risk factors for mortality, whereas CA in the PICU and initial VT or VF rhythms were good prognostic factors.
Neurological outcome
The neurological status at hospital discharge was assessed in 120 patients (60.9 %), and 88.9 % of them had a normal neurological status or showed mild disability. Among 107 survivors who had both pre-arrest and discharge PCPC scores, 89.2 % had a good neurological outcome or no change from pre-arrest to hospital discharge.
Discussion
To our knowledge, this is the first prospective, multicenter, multinational study that describes the outcome of in-hospital CA in children according to the Utstein style guidelines and analyses its prognostic factors.
A large number of patients, though probably not all of whom suffered CA, were included from a wide range of different hospitals in several countries, and this has enabled us to obtain a representative sample of true in-hospital CA in children.
Sustained ROSC was achieved in 69.5 % patients. Secondary in-hospital mortality among the initial survivors of CA was 43.5 % and survival at hospital discharge was therefore 39.2 %. Our mortality figures are in a similar range to those of reported national single-center and multicenter studies in children [1–14, 21] (Table 5), although very different hospitals from several countries participated in the present study.
Continent, countries, and Human Development Index
In our study, children in European countries had a significantly lower mortality than those in Latin American countries. However, continent was not a significant risk factor for mortality in the multivariate logistic regression analysis. In contrast, patients in high HDI countries had a lower mortality than those in medium HDI countries, and this risk factor maintained its statistical significance in the multivariate analysis. In addition, the percentage of children who suffered CA in the ED in the medium HDI countries was higher than in the rest of countries. Although other factors could have influenced these results, the most important causes in our opinion are a lack of organization for in-hospital CA and a lack of intensive care beds in those countries, together with a scarcity of material resources and less preparedness of the teams to practice CPR. It is therefore essential that each country and hospital assesses its needs for PICUs and beds with monitoring and surveillance. The development of specific programs of in-hospital ‘chain of prevention’ [22] with rapid response teams to prevent CA in patients outside the PICU is necessary [23, 24]. These teams are more necessary and useful in hospitals with a lower PICU bed availability [25].
Age and sex
The number of boys suffering CA was higher than the number of girls, as has been found in other studies [1, 2, 11, 21]. Children weighing less than 10 kg presented a lower mortality than those over 10 kg, as has been reported by other authors [10, 21]. However, sex, age, and weight were not found to be significant risk factors in the multivariate study. It is possible that the etiology of CA could have influenced the results, as respiratory causes were more common in infants and oncohematologic diseases more common in children. However Meaney et al. [10] performed extensive comparisons of mortality in in-hospital CA between children of different age groups and they found that the survival advantage persisted even after controlling for all potentially confounding pre-arrest, arrest, and resuscitation variables.
Preexisting diseases, previous neurological status, and previous treatment
Preexisting conditions were present in many patients [3, 9, 12, 21] but only hematologic and oncologic diseases were identified as significant risk factors for mortality in the multivariate analysis. This finding has also been reported by other authors [11, 12, 21].
Pre-arrest neurological status was normal in most patients, and pre-arrest PCPC score was not associated with survival, as described by other authors [12].
Mortality was not higher among monitored patients on mechanical ventilation (most of them in the PICU), probably because the diagnosis of CA in these patients was rapid and they did not require additional respiratory maneuvers during resuscitation. On the other hand, children who were receiving inotropic drugs at the time of arrest did present a higher mortality, as has been reported in other studies in adults and children [6, 9, 11, 26]. This finding only indicates that these are the most severely ill patients, with major hemodynamic disturbances, and they therefore have a poorer prognosis even though they are in intensive care units and receive early and adequate resuscitation.
Characteristics of the cardiac arrest
Etiology of arrest
The most common causes of CA were respiratory and cardiac diseases, coinciding with the findings of other authors [7, 21]. However, in our study, sepsis was also a very frequent cause of CA, much more common than in other studies [7, 21]. Sepsis was more common in countries with a lower HDI, as found in a study in adults [25]. This finding is very important because sepsis was one of the poorest prognostic factors in CA, [6] and it highlights the importance of establishing measures for the early diagnosis and treatment of sepsis [27].
Site of arrest
While agreeing with other studies reporting that the majority of CAs occurred in the PICU [2, 4, 7, 8, 11, 12, 21], it is noteworthy that a higher percentage of children suffered CA in the ED in countries with a lower HDI. This is an important finding because CA in the ED had a higher mortality than CA occurring in other hospital areas [28]. This may be because emergency areas are probably less capable of monitoring and treating patients who have still not been adequately stabilized. In addition, it must be taken into account that in some countries with few PICU beds, critically ill children are treated in the ED until they have room in the PICU. This underlines the importance of having areas for stabilization and monitoring in pediatric emergency areas, with staff specifically trained to prevent and treat CA.
Rhythm
In our series, asystole was the most common initial documented cardiac rhythm in contrast to the findings of other recent studies in children, in which bradycardia was more frequent [7, 11, 21]. This suggests that the diagnosis of CA in many patients was delayed. Only 6 % of our patients presented shockable rhythms (VF and pulseless VT) initially, a percentage similar to other studies in children [2–4, 7, 11, 12]. Shockable rhythms achieved significantly higher survival rates in the multivariate analysis [2, 3, 11, 12, 21].
Time to initiation of cardiopulmonary resuscitation
The time from the arrest to the initiation of resuscitation is believed to be one of the main factors influencing survival after out-of-hospital CA [4, 29]. In the case of in-hospital CA the time to initiation of resuscitation is typically short [12, 21] and this fact could explain why there were no significant differences in prognosis according to the time to initiation of resuscitation in this study. However, this delay is one of the most difficult variables to record accurately and these results should be interpreted with caution.
Resuscitation maneuvers
Patients who required more advanced life support procedures and higher doses of epinephrine had higher mortality [13, 22]. However, the most important resuscitation predictor of mortality was the duration of life support measures [1–3, 11, 12]. In the multivariate study, a total life support time longer than 10 min was identified as a prognostic risk factor. This finding highlights the importance of implementing early resuscitation measures and could be an indicator of the need to establish resuscitation with extracorporeal membrane oxygenation in those hospitals in which this technique is available.
Clinical course
Patients who presented more than one episode of CA had a slightly higher mortality, as has been reported in other studies [1, 2, 12], although the difference did not reach statistical significance in our study.
The majority of patients who survived had a good neurological outcome although this could only be analyzed in 60 % of survivors. Survival without sequelae was comparable with figures reported in other studies in children [3–6, 8–10, 12, 14] (Table 5).
Our study has several limitations. It was a large, multicenter, observational study, but it included very different countries, hospitals, and investigators. One of the most important problems in multicenter studies is to ensure the validity of data. In our study two specific pediatric intensivists acted as data managers and reviewed each datum included and they checked for inconsistent and missing data. Although our study analyzed a significant number of patients, the figures from some hospitals and countries were low. Thus it was not possible to compare CA and resuscitation between countries and hospitals. Moreover, although we requested that all cases of CA be included, a selection bias could have occurred in two ways: the selection of cases with good results or else the most complicated cases with poorest outcomes. The heterogeneity and variability in data abstraction could potentially limit the validity of our results. Comparisons between countries and hospitals were not among the objectives of this study, nor did our data permit this [28]. The reality within each country or hospital can be very different, and it was not therefore possible to detect risk factors that could be used to improve prevention and CPR.
Furthermore, socioeconomic classifications must be interpreted with caution, particularly as a recent study has shown that HDI can misclassify some countries [30].
We conclude that the most important prognostic risk factors for mortality in in-hospital CA in children in this international multicenter study were the occurrence of CA in lower HDI countries, preexisting oncohematologic disease, CA occurring outside the PICU, CA caused by neurological disease, and a duration of CPR longer than 10 min. However, each hospital and country has different characteristics that may influence the outcome of CPR [28]. Some of these factors cannot be modified. It is therefore very important to focus efforts on improving not only the techniques and specific measures of CPR, but also the hospital organization to care for children at risk of CA both in the PICU and in other hospital areas, particularly in emergency departments.
References
Slonim AD, Patel KM, Ruttimann UE, Pollack MM (1997) Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med 25:1951–1955
Suominen P, Olkkola KT, Voipio V, Korpela R, Palo R, Räsänan J (2000) Utstein style reporting of-in hospital paediatric cardiopulmonary resuscitation. Resuscitation 45:17–25
Reis AG, Nadkarni V, Perondi MB, Grisi S, Berg RA (2002) A prospective investigation into the epidemiology of in-hospital pediatric cardiopulmonary resuscitation using the international Utstein reporting style. Pediatrics 109:200–209
López-Herce J, García C, Domínguez P, Carrillo A, Rodríguez-Núñez A, Calvo C, Delgado MA, The Spanish Study Group of Cardiopulmonary Arrest in Children (2004) Characteristics and outcome of cardiorespiratory arrest in children. Resuscitation 63:311–313
Guay J, Lortie L (2004) An evaluation of pediatric in-hospital advanced life support interventions using the pediatric Utstein guidelines: a review of 203 cardiorespiratory arrests. Can J Anaesth 51:373–378
Rodriguez-Núñez A, López-Herce J, García C, Carrillo A, Dominguez P, Calvo C, Delgado MA, The Spanish Study Group of Cardiopulmonary Arrest in Children (2006) Effectiveness and long-term outcome of cardiopulmonary resuscitation in paediatric intensive care units in Spain. Resuscitation 71:301–309
Tibballs J, Kinney S (2006) A prospective study of outcome of in-patient paediatric cardiopulmonary arrest. Resuscitation 71:310–318
Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, Berg RA, National Registry of Cardiopulmonary Resuscitation Investigators (2006) First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 295:96–98
De Mos N, van Litsenburg RR, McCrindle B, Bohn DJ, Parshuram CS (2006) Pediatric in-intensive-care-unit cardiac arrest: incidence, survival, and predictive factors. Crit Care Med 34:1209–1215
Meaney PA, Nadkarni VM, Cook EF, Testa M, Helfaer M, Kaye W, Larkin GL, Berg RA, National Registry of Cardiopulmonary Resuscitation Investigators (2006) Higher survival rates among younger patients after pediatric intensive care unit cardiac arrest. Pediatrics 118:2424–2433
Wu ET, Li MJ, Huang SC, Wang CC, Liu YP, Lu FL, Ko WJ, Wang MJ, Wang JK, Wu MH (2009) Survey of outcome of CPR in pediatric in-hospital cardiac arrest in a medical center in Taiwan. Resuscitation 80:443–448
Meert KL, Donaldson A, Nadkarni V, Tieves KS, Schleien CL, Brilli RJ, Clark RS, Shaffner DH, Levy F, Statler K, Dalton HJ, van der Jagt EW, Hackbarth R, Pretzlaff R, Hernan L, Dean JM, Moler FW (2009) Pediatric Emergency Care Applied Research Network. Multicenter cohort study of in-hospital pediatric cardiac arrest. Pediatr Crit Care Med 10:544–553
Olotu A, Ndiritu M, Ismael M, Mohammed S, Mithwani S, Maitland K, Newton CR (2009) Characteristics and outcome of cardiopulmonary resuscitation in hospitalised African children. Resuscitation 80:69–72
Berens RJ, Cassidy LD, Matchey J, Campbell D, Colpaert KD, Welch T, Lawson M, Peterson C, O’Flynn J, Dearth M, Tieves KS (2011) Probability of survival based on etiology of cardiopulmonary arrest in pediatric patients. Paediatr Anaesth 21:834–840
Cummins R, Chamberlain D, Hazinski MF, Nadkarni V, Kloek W, Kramer E (1997) Recommended guidelines for reviewing, reporting, and conducting research on in hospital resuscitation: the in-hospital “Utstein style”. Resuscitation 34:151–183
Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes (2004) Cardiac arrest and cardiopulmonary resuscitation outcomes reports: update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 110:3385–3397
Fiser DH, Long N, Roberson PK, Heffley G, Zolten K, Brodie-Fowler M (2000) Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit Care Med 28:2616–2620
The World Bank (2012). http://data.worldbank.org/about/country-classifications/country-and-lending-groups. Accessed date 10 Apr 2012
World Health Organization (2012) http://www.who.int/en/ Accessed date 10 Apr 2012
Human Development Reports (2012) http://hdr.undp.org/en/ Accessed date 10 Apr 2012
Moler FW, Meert K, Donaldson AE, Nadkarni V, Brilli RJ, Dalton HJ, Clark RS, Shaffner DH, Schleien CL, Statler K, Tieves KS, Hackbarth R, Pretzlaff R, van der Jagt EW, Levy F, Hernan L, Silverstein FS, Dean JM, Pediatric Emergency Care Applied Research Network (2009) In-hospital versus out-of-hospital pediatric cardiac arrest: a multicenter cohort study. Crit Care Med 37:2259–2267
Smith GB (2010) In-hospital cardiac arrest: is it time for an in-hospital ‘chain of prevention’? Resuscitation 81:1209–1211
Sharek PJ, Parast LM, Leong K, Coombs J, Earnest K, Sullivan J, Frankel LR, Roth SJ (2007) Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA 298:2267–2274
Tibballs J, Kinney S (2009) Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatr Crit Care Med 10:306–312
Suraseranivongse S, Chawaruechai T, Saengsung P, Komoltri C (2006) Outcome of cardiopulmonary resuscitation in a 2300-bed hospital in a developing country. Resuscitation 71:188–193
Tian J, Kaufman DA, Zarich S, Chan PS, Ong P, Amoateng-Adjepong Y, Manthous CA, American Heart Association National Registry for Cardiopulmonary Resuscitation Investigators (2010) Outcomes of critically ill patients who received cardiopulmonary resuscitation. Am J Respir Crit Care Med 182:501–506
Kissoon N, Carcillo JA, Espinosa V, Argent A, Devictor D, Madden M, Singhi S, van der Voort E, Latour J, Global Sepsis Initiative Vanguard Center Contributors. World Federation of Pediatric Intensive Care and Critical Care Societies (2011) Global Sepsis Initiative. Pediatr Crit Care Med 12:494–503
Donoghue AJ, Nadkarni VM, Elliott M, Durbin D, American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators (2006) Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the national registry of cardiopulmonary resuscitation. Pediatrics 118:995–1001
Sasson C, Rogers MA, Dahl J, Kellermann AL (2010) Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 3:63–81
Wolff H, Chong HG, Auffhammer M (2011) Classification, detection and consequences of data error: evidence from the Human Development Index. Econ J 121:843–870
Acknowledgments
This study was supported in part by grant RT02377 from the Science and Technology for Development (CYTED) Program and by grant PI081167 from Carlos III Institute of Health, Spain.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The investigators of the Iberoamerican Pediatric Cardiac Arrest Study are listed in the Appendix.
List of the investigators of the Iberoamerican Pediatric Cardiac Arrest Study
List of the investigators of the Iberoamerican Pediatric Cardiac Arrest Study
Network: Jesús López-Herce, Jimena del Castillo, Javier Urbano, Angel Carrillo, Jose María Bellón (Hospital General Universitario Gregorio Marañón, Madrid, Spain), Martha Matamoros, Roger Rodriguez, Allison Callejas, Douglas Carranza (Hospital Escuela, Tegucigalpa, Honduras), Sonia Cañadas, Pedro Dominguez (Hospital Valle de Hebrón, Barcelona, Spain), Ana Rodriguez Calvo, Lorenzo Marcos (Hospital Niño Jesús, Tucumán, Argentina), Corrado Cecchetti (Ospedale Bambinu Gesu, Roma, Italy), Marta Silva (Hospital San Joao, Porto, Portugal), Regina Grigolli Cesar (Irmandade da Santa Casa de Misericordia, Sao Paulo, Brasil), Javier Pilar Orive (Hospital de Cruces, Baracaldo, Spain), Ana María Nieva (Hospital de Niños Ricardo Gutiérrez, Buenos Aires, Argentina), Antonio Rodríguez-Nuñez (Hospital Clínico Universitario, Santiago de Compostela, Spain), Marta Parada (Hospital Pediatrico, Coimbra, Portugal), María Angeles García Teresa (Hospital Niño Jesús, Madrid, Spain), Di Prietro Pasquale (Ospedale Gaslini, Genova, Italy), Miguel Angel Delgado (Hospital Universitario La Paz, Madrid, Spain), Mauricio Fernández, Hospital Pablo Tobón Uribe, Medellín, Colombia), Roxana Flavia Jaén (Hospital Británico, Buenos Aires, Argentina), Juan Garbayo Solana (Hospital Reina Sofía, Córdoba, España), Raúl Borrego Domínguez (Hospital Virgen de la Salud, Toledo, Spain), Víctor Monreal (Hospital Roberto del Río, Santiago de Chile, Chile), Cristina Molinos (Hospital de Cabueñes, Asturias, Spain), Iolster Thomas (Hospital Universitario Austral, Buenos Aires, Argentina), Ricardo Iramaín (Hospital Nacional de Asunción, Asunción, Paraguay), Juan Carlos de Carlos (Hospital Son Dureta, Palma de Mallorca, Spain), Corsino Rey Galán (Hospital Central de Asturias, Oviedo, Spain), Olivia Pérez Quevedo (Hospital Materno Infantil de Las Palmas, Las Palmas de Gran Canaria, Spain), Adriana Koliski (Hospital da clinicas da UFPR, Curitiba, Brasil), Santiago Campos (Hospital SOLCA, Quito, Ecuador), Alfredo Reparaz (Complexo Hospitalario Universitario de Vigo, Vigo, Spain), Sivia Sánchez Pérez (Corporacion Parc Taul, Sabadell, Spain), Deolinda Matos (Hospital García de Orta, Almada, Portugal), Claudia Carolina Benaroya Hospital Regional Río Gallegos, Río Gallegos, Argentina), Lourdes Marroquín Yañez (Hospital Infantil de México Federico Gómez, México), Antonio de Francisco (Hospital Germans Trias i Pujol, Barcelona, Spain).
Rights and permissions
About this article
Cite this article
López-Herce, J., del Castillo, J., Matamoros, M. et al. Factors associated with mortality in pediatric in-hospital cardiac arrest: a prospective multicenter multinational observational study. Intensive Care Med 39, 309–318 (2013). https://doi.org/10.1007/s00134-012-2709-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2709-7