Abstract
Objectives
To test the performance of PIM2 in French-speaking (FS) paediatric intensive care units (PICUs) and its relative performance when recalibrated using data from FS and Great Britain (GB) PICUs of different size.
Methods
Consecutive admissions to 15 FS (n = 5,602) and 31 GB PICUs (n = 20,693) from June 2006 to October 2007 were included. The recalibrated PIM2 were applied to PICUs of different size within the FS and GB PICUs and between the two groups. PICU size was defined using number of admissions/month. Discrimination and calibration were evaluated using the area under the ROC curve (AUC) and the goodness-of-fit test, respectively. Logistic regression, funnel plots and standardized W scores were performed in the two groups and between different PICU sizes.
Results
In FS PICUs, the original PIM2 had good discrimination (AUC = 0.85) and moderate calibration (p = 0.07). The recalibrated PIM2 scores had good calibration in FS (p = 0.33) and moderate calibration in GB (p = 0.06). Calibration was poor when the recalibrated FS PIM2 was applied to GB (p = 0.02) but good when the GB recalibration was applied to the FS (p = 0.36). Using the original PIM2 coefficients, calibration was poor in large units in both groups but improved following recalibration. There were no effects of PICU size on risk-adjusted mortality in GB and a significant effect in the FS PICUs with a minimum risk-adjusted mortality at about 35 admissions/month.
Conclusion
The PIM2 score was valid in the FS population. The recalibration based on GB data could be applied to FS PICUs. Such recalibration may facilitate comparisons between countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prognostic models for groups of children admitted to paediatric intensive care units (PICUs) are now standard components of the methodology used in intensive care quality assurance and research [1–4]. Indeed, they are integrated in databases of paediatric networks [5–7]. Two predictive scoring systems have been proposed for critically ill children: the pediatric risk of mortality (PRISM and PRISM III) and the paediatric index of mortality (PIM and PIM2) [8, 9]. PIM2 was initially validated in 20,787 critically ill children from 14 large PICUs in Australia, New Zealand and the UK and was validated after recalibration in the UK demonstrating satisfactory performance [10]. This score has never, however, been studied in a prospective multicentre study in France.
Prognostic scoring systems that are developed in one country require recalibration (i.e. adapted coefficients) before being used to provide risk-adjusted outcomes of PICU mortality for units within a new health care setting [10]. Local recalibration has been reported to improve the performance of adult scoring systems in individual countries or regions [11–13]. Nevertheless, some authors have suggested that recalibration can compromise the ideal of comparisons between different geographic zones [13, 14]. Thus, the impact of the recalibration between two European countries on the performance of the score, in order to enable some comparisons, has never been evaluated.
Structural and process factors might explain variations in outcomes [15, 16]. The effect of volume of patients on quality of paediatric intensive care has been a subject of debate in North America [17] as three out of four studies found higher volume units had lower mortality [15, 18–20]. A better understanding of this relationship is needed to develop effective regionalization and referral policies for critically ill children [15, 18]. The performance of a unit for its case mix can be compared with the expected performance of a reference group of providers for a similar case mix [21]. Before any comparison of performance between PICUs of different size is conducted, it is important that the risk-adjusted mortality is accurately predicted.
The first objective of this study was to test the performance of the PIM2 score in French-speaking (FS) PICUs and the relative performance of the PIM2 score when recalibrated using data from FS countries and Great Britain (GB). The second objective was to compare the performance of large, medium and small sized units in FS and GB PICUs.
Methods
All the 33 neonatal and PICUs (NPICUs)/PICUs and two PICUs affiliated to the Groupe Francophone de Réanimation et Urgences Pediatriques (GFRUP) were invited to participate on a voluntary basis: 17 agreed, and 15 (13 NPICUs/PICUs and two PICUs) provided the information requested (14 in France and one in Belgium). All consecutive children admitted to these PICUs between 21 June 2006 and 31 October 2007 were included. Children with a history of prematurity and hospitalized after birth were included. Those over 18 years and newborns who were premature (<37 weeks gestation) and admitted at birth were excluded.
Although the period of data collection varied between units, for each unit all patients admitted consecutively during the study period were included.
During the same period, 31 PICUs in GB from the PICANet database were analysed in order to perform comparative analysis. The selection process and data collection methods have been previously published [10]. Information were prospectively collected for each admission (demographic details, PIM2 score, outcome at PICU discharge (death, alive)). Children were excluded from the analysis if they were aged over 18 years, or less than 2 years and born prematurely (<37 weeks gestation).
Legal considerations
Data collected from routine practice were used in this FS observational study. The two databases were declared to and approved by the French and English authorities (see electronic supplementary material, ESM).
Data collection and management
Clinical data were prospectively recorded on a standardised case-report form. Previously trained physicians (one per centre) entered data into a Web-based database respecting confidentiality requirements (Epiconcept™, Paris, France) (see ESM).
Statistical analysis
Design of analyses
Outcome was vital status at PICU discharge. Validation of the PIM2 score was evaluated with the original published coefficients (FS-PIM2 and GB-PIM2 scores respectively). In each data set, a random sample of half of the population was selected to provide a development data set. Re-estimation of coefficients (recalibration) was conducted in this development set: individual component variables of the PIM2 score (independent variables) were entered into a logistic regression using the PICU discharge as dependent variable. These two steps were repeated 5,000 times (bootstrap procedure). Bootstrapping is a method employed to resample from the original data to create replicate data sets, from which the variability of the quantities of interest can be assessed. The aim is to create alternative versions of data that “we might have seen” [22]. From the 5,000 coefficients obtained, the best model was selected using the mean coefficients of each independent variable. Final coefficients of the recalibrated model were applied on the data set of each country, and two models named ‘GB-Rec-PIM2’ score and ‘FS-Rec-PIM2’ score were provided (Fig. 1, ESM). A cross-recalibration was performed as follows: coefficients of the recalibrated FS model were applied to the GB data set (model named ‘GB-RecFS coeff-PIM2’ score) and coefficients of the recalibrated GB model were applied to the FS data set (model named ‘FS-RecGB coeff-PIM2’ score) (Fig. 1, ESM).
This analysis was stratified by PICU level of activity. To define small, medium or large units, an equal number of PICUs in each group taking into account the number of admissions per month (admissions per year) was determined from the FS data set; the defined cut-offs were less than 20 (240), 20–35 (240–420) and greater than 35 (420), close to the two cut-offs mentioned in the study by Wolfler et al. [14].
Calibration, discrimination and performance
Calibration: In order to compare observed with expected mortality and to estimate the calibration of the PIM2 score, a Hosmer–Lemeshow goodness-of-fit test was performed using the logit of the PIM2 score following logistic regression [23] (see ESM).
Discrimination: Area under the receiver operating characteristic curve (AUC) and standard error were calculated to estimate the discrimination of the scores (see ESM).
Funnel plots: Funnels plots of PICU mortality ratios by number of admissions along with corresponding 99.8 % control limits were produced. Funnel plots are a variation on control charts that identify PICUs with unexpectedly high (above upper control limit) or low (below the lower control limit) mortality (see ESM).
Standardized W score: The standardized W score (Ws) produced the number of excess or lack of survivors per 100 patients compared with the prediction [24, 25]. The standard error (SE) of Ws is also calculated to provide the 95 % confidence interval (CI) [24] (see ESM).
Logistic regression: A logistic regression was used to study size effect, with size as categorical or continuous variable (see ESM). Statistical analyses were performed using STATAv10 statistical software (StataCorp LP 2004, Texas, USA).
Results
Among the 15 FS PICUs, no PICUs were exclusively devoted to cardiac surgery. Fourteen PICUs were devoted to medical, trauma and post-operative care (including cardiac surgery). One PICU admitted only medical patients. Among 5,651 patients, we excluded two patients older than 18 and 47 patients with incomplete data. Thus, 5,602 patients (414 died, mortality rate 7.39 %) were included. Primary category of illness on admission was congenital disease (33 %), infection (24 %), trauma (8 %), chemical injury (2 %), drug (0.1 %), cancer (3 %), diabetes (1 %), allergic immunologic disease (2 %) and other/undetermined (21 %). For GB PICUS, data are available on the PICANet website [26]. In GB PICUs 20,693 patients (1,014 died, mortality rate 4.90 %) were included. Characteristics and comparisons between the two populations are given in Table 1.
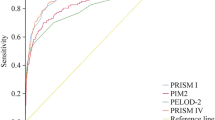
In FS PICUs, the FS-PIM2 score had a good discriminatory power (AUC 0.85; 95 % CI 0.83–0.87) and a moderate calibration (p = 0.07). The FS-Rec-PIM2 score had a good calibration (p = 0.33) and the GB-Rec-PIM2 had a moderate calibration (p = 0.06) (Table 2). The GB-RecFS coeff-PIM2 score displayed lack of fit and therefore poor calibration (p = 0.02), whereas the FS-RecGB coeff-PIM2 score displayed good calibration (p = 0.36) (Table 2).
In the GB data set, calibration plots showed that the GB-PIM2 tended to overestimate risk in low-risk mortality patients by less than 1 % in GB and 4 % in FS using the original and recalibrated equations (Fig. 2a, b for GB and Fig. 2c, d for FS PICUs, in ESM).
PICU size
Using the original PIM2 coefficients, calibration was good in small and medium units (p = 0.25 and p = 0.78 in FS and p = 0.99 and p = 0.25 in GB respectively) and poor in large units (p = 0.03 in FS and p = 0.001 in GB). In both groups, recalibrated and cross-recalibrated PIM2 scores provided good discriminatory power and calibration in small, median and large units (Table 2).
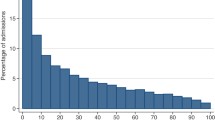
Funnel plots of crude mortality ratios by number of admissions for each unit indicated that three FS and seven GB PICUs had unadjusted mortality ratios that were lower or higher than expected (Fig. 1). Funnel plots using the original PIM2 score indicated that no PICU in France and only two PICUs in GB had adjusted mortality ratios that were lower than expected (Fig. 1). Funnel plots using the recalibrated PIM2 score indicated that no PICU in FS and only one PICU in GB had an adjusted mortality ratio that was lower than expected (Fig. 1). In the GB data set, one PICU had an observed mortality ratio equal to zero (no patient died in this PICU during the study period) and so this PICU was out of the lower limit of agreement in the three analyses (Fig. 1).
Funnels plots of GB and FS PICUs using crude mortality ratio, original PIM2 score mortality ratio and recalibrated PIM2 score mortality ratio. The mortality ratio then is plotted on the y-axis against the number of admissions to the PICU on the x-axis. To satisfy the condition that if the distribution of the mortality ratios is random there exists an ~5 % chance of a unit falling outside the control limits, then the upper and lower control limits must represent not 95 % confidence intervals but 99.7 % (confidence intervals around a mortality ratio of 1 by number of admissions [41]. *Crude mortality ratio: observed PICU mortality/whole population mortality. **Original PIM2 mortality ratio: observed PICU mortality/original PIM2 expected mortality (respectively FS PIM2 score and GB PIM2 score). ***Recalibrated PIM2 mortality ratio: observed PICU mortality/recalibrated PIM2 expected mortality (respectively FS-Rec-PIM2 score and GB-Rec-PIM2 score). PIM paediatric index of mortality, GB Great Britain, FS French speaking
Using the original PIM2 score, the standardized Ws scores demonstrated fewer survivors per 100 cases in small and large FS PICUs, whereas the standardized Ws scores demonstrated an excess of survivors per 100 cases in medium and large GB PICUs (Table 3). With the recalibrated PIM2 scores, the standardized Ws scores did not demonstrate a lack or excess of survivors in small, medium and large PICUs in either group (Table 3).
Odds ratios of PICUs size (small PICUs as reference) were not significant in both groups after adjustment for original and recalibrated PIM2 scores respectively (Table 3).
In the English data neither linear nor quadratic models showed any significant effect. In contrast with the French data a linear model showed no significant effect, but a quadratic model did (overall chi2 = 8.6, 2 df, p = 0.014) (Fig. 3a, b, ESM). The parameters indicated a minimum risk-adjusted mortality at about 35 admissions/month in the FS PICUs (Fig. 3a, ESM).
Discussion
First, this study has shown that the PIM2 score was valid in the FS population and that the recalibration based on GB data could be applied to FS PICUs. Second, for the recalibrated PIM2 score, the volume of patients showed no effect in GB but did in the FS PICUs, with a minimum risk-adjusted mortality at about 35 admissions per month.
The PIM2 score was chosen because it is free and is very simple to collect. Moreover, several studies have showed that the PIM2 score had a good performance in different countries with [3, 10, 27] or without [14, 28] recalibration. In our study, and considering only the FS data set, the performance of the PIM2 score was good with and without recalibration.
Because of diversity in case mix, structure, organization, staffing and management between different countries [8, 29], region-specific or country-specific equations have been proposed in order to compare ICUs on a similar level [30]. Usually, discrimination and calibration of prognostic scoring systems are good in the population used for the development and for the internal validation. However, in almost all cases, when these scoring systems are applied to a new population, calibration deteriorates although discrimination hardly changes [13]. Recalibration had a large impact on the performance of the models, improving in particular its calibration [31]. We have used the same recalibrated PIM2 score to make the comparison between these two different countries. Conversely, “there is a ‘risk’ to risk adjustment” because different models will not always agree on the identity of outlier performing institutions and on ranking the institutions [31]. The PIM2 score was initially developed from a study in Australia, New Zealand and UK, without recalibration between these three countries [9]. Furthermore, cross comparisons between different countries with recalibrated severity scoring systems had never been evaluated. In our study, the recalibrated PIM2 score in the GB data set could be applied to the FS data set, but not vice versa. Hypotheses to explain this result might be the larger population of the GB data set and the inclusion of all GB PICUs which cover a wider range of individuals or risks. Recalibration based on the GB data set and applied to FS and GB PICUs data sets have shown that case mixes from two countries can be considered as case mixes from two regions (states) in the same country. Indeed, differences in case mix between PICUs in the same country have been previously reported. Outcome description of 20 PICUs in the USA showed a significant variation among centres in mortality rate (from 1.4 to 21.3 %) or mean PRISM III score (from 2.42 to 11.18) [32]. Moreover, the annual report of the Australian and New Zealand Paediatric Intensive Care Registry in 2009 described mortality rates from 1 to 9 % and mechanical ventilation percentages from 7.5 to 100 % (three centres with no ventilated patients excluded) [33].
Definitions of the size of units vary between paediatric studies: small and large units were determined by the population median of six or fewer beds and more than six beds [17, 19], institutions’ volume as medium (mean 45.6 patients/month), low (mean 26.8 patients/month) and high (mean 72.6 patients/month) [20]. In another study, cut-offs were not defined but there was a slight increase in mortality rates among PICUs with very high annual admission volumes (about 1,500 admissions per year) [18]. In the study by Wolfler et al., all PICUs were paediatric (mean number of children per year per unit 181) and most PICUs were small (4–6 beds) and had no more than 200–400 admissions per year [14]. Using a comparable definition of size, we did not observe any differences between centres on discrimination and calibration. In our study, the funnel plots for the recalibrated PIM2 indicated that the adjusted mortality rate for all units in France and the UK was consistent. These results were observed with the PIM, PIM2, PRISM and PRISM III scores in 26 PICUs in the UK [10]. The relation between SMR and FS PICU volume suggested a reversed J-shaped relationship. Such a relationship was previously observed in data from North America PICUs, with a lowest theoretical threshold of 1,250 annual admissions, more than observed in our study (420 admissions per year) [18]. A recent study in Australia and New Zealand PICUs used a modified plot of risk-adjusted mortality ratio versus unit mean length of stay: two units were designated as inefficient and one unit was considered to be effective at the expense of high resource use [34].
Strengths and limitations
The two databases were of different size. It is possible that the different sample sizes between the two countries explain this result. The GB sample was larger than the FS sample and the probability that the GB sample included patients similar to those of the FS sample is more important than the opposite scenario. Thus, the result of the recalibration based on GB data applied to FS PICUs could be better. Nevertheless, the FS data set included more than 5,000 patients and, thus, the power of the statistical analysis seems acceptable. The case mix was different between these two countries. Infant mortality rate is lower in France than in the UK (3.6/1,000 versus 4.7/1,000) [35], but in the present study, crude mortality was higher in the FS database. Such differences have previously been observed: crude mortality in PICUs was lower in Australia (4.1%) than in the UK (8.2 %) [9], whereas the infant mortality rate (4.4/1,000 versus 4.7/1,000 respectively) is about the same in these two countries [35]. In the study by Brady et al. optimized models were assessed by random allocation of PICUs (stratified by annual admission number) into development and validation samples in a 2:1 ratio [10]. In our study, a randomization by patient and a bootstrap procedure were applied on half of each data set to decrease the potential inflation of the new predictive equation applied to the entire data set. The bootstrap methods can be used to assess the strength of evidence that an identified variable is an important predictor [36]. For the Hosmer–Lemeshow goodness of fit test, we used degrees of freedom equal to the number of groups [37]. The use of degrees of freedom equal to number of groups minus 2 gave the same results (data not shown) except for the original FS-PIM 2 and GB-Rec-PIM2 scores which were not calibrated (p = 0.03 and p = 0.02 respectively). The relationship between volume and outcome is influenced by few variables, such as length of stay, nursing workload and number of premature infants cared for in NPICU, which were not taken into account in our analysis [34, 38]. Finally, in the FS data set only the voluntary PICUs were included, whereas Glance [39] has proposed that all ICUs participate in a national ICU-outcome database as was the case for the GB data set. Universal participation would eliminate the possibility of selection bias, in contrast to voluntary participation that may result in a non-representative group of ICUs [39].
Conclusion
This study has demonstrated that PIM2 was valid in the FS PICUs. Also, the same recalibration could be applied to two different countries. Calibration of scoring systems should be reassessed periodically to ensure their continued validity. Nowadays, severity scoring systems have to be applied to monitor outcome and, thus, improve the quality of paediatric intensive care networks [40]. If a European paediatric intensive care registry is established, the results of this study support the possibility that a single, appropriately calibrated, risk adjustment model could be used for quality improvement and research within Europe and for comparative analyses between European countries.
References
Lacroix J, Cotting J (2005) Severity of illness and organ dysfunction scoring in children. Pediatr Crit Care Med 6:S126–S134
Martinot A, Leteurtre S, Grandbastien B, Duhamel A, Leclerc F (1997) Characteristics of patients and use of resource in French pediatric intensive care units. Arch Pediatr 4:730–736
Slater A, Shann F (2004) The suitability of the pediatric index of mortality (PIM), PIM2, the pediatric risk of mortality (PRISM), and PRISM III for monitoring the quality of pediatric intensive care in Australia and New Zealand. Pediatr Crit Care Med 5:447–454
Wunsch H, Rowan KM, Angus DC (2007) International comparisons in critical care: a necessity and challenge. Curr Opin Crit Care 13:725–731
LaRovere JM, Jeffries HE, Sachdeva RC, Rice TB, Wetzel RC, Cooper DS, Bird GL, Ghanayem NS, Checchia PA, Chang AC, Wessel DL (2008) Databases for assessing the outcomes of the treatment of patients with congenital and paediatric cardiac disease: the perspective of critical care. Cardiol Young 18(Suppl 2):130–136
Parslow RC, Tasker RC, Draper ES, Parry GJ, Jones S, Chater T, Thiru K, McKinney PA (2009) Epidemiology of critically ill children in England and Wales: incidence, mortality, deprivation and ethnicity. Arch Dis Child 94:210–215
Slater A, Shann F, McEniery J (2003) The ANZPIC registry diagnostic codes: a system for coding reasons for admitting children to intensive care. Intensive Care Med 29:271–277
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated pediatric risk of mortality score. Crit Care Med 24:743–752
Slater A, Shann F, Pearson G (2003) PIM2: a revised version of the paediatric index of mortality. Intensive Care Med 29:278–285
Brady AR, Harrison D, Black S, Jones S, Rowan K, Pearson G, Ratcliffe J, Parry GJ (2006) Assessment and optimization of mortality prediction tools for admissions to pediatric intensive care in the United Kingdom. Pediatrics 117:e733–e742
Chase JG, Shaw GM (2012) How standard is the “S” in SMR? Intensive Care Med 38:1–3
Minne L, Eslami S, de Keizer N, de Jonge E, de Rooij SE, Abu-Hanna A (2012) Effect of changes over time in the performance of a customized SAPS-II model on the quality of care assessment. Intensive Care Med 38:40–46
Vincent JL, Moreno R (2010) Clinical review: scoring systems in the critically ill. Crit Care 14:207
Wolfler A, Silvani P, Musicco M, Salvo I (2007) Pediatric index of mortality 2 score in Italy: a multicenter, prospective, observational study. Intensive Care Med 33:1407–1413
Tilford JM, Simpson PM, Green JW, Lensing S, Fiser DH (2000) Volume-outcome relationships in pediatric intensive care units. Pediatrics 106:289–294
Cogo PE, Poole D, Codazzi D, Boniotti C, Capretta A, Langer M, Luciani D, Rossi C, Bertolini G (2010) Outcome of children admitted to adult intensive care units in Italy between 2003 and 2007. Intensive Care Med 36:1403–1409
Pollack MM (2007) Pediatric intensive care quality factors. J Trauma 63:S143–S145
Marcin JP, Song J, Leigh JP (2005) The impact of pediatric intensive care unit volume on mortality: a hierarchical instrumental variable analysis. Pediatr Crit Care Med 6:136–141
Pollack MM, Cuerdon TT, Patel KM, Ruttimann UE, Getson PR, Levetown M (1994) Impact of quality-of-care factors on pediatric intensive care unit mortality. JAMA 272:941–946
Ruttimann UE, Patel KM, Pollack MM (2000) Relevance of diagnostic diversity and patient volumes for quality and length of stay in pediatric intensive care units. Pediatr Crit Care Med 1:133–139
Shahian DM, Normand SL (2008) Comparison of “risk-adjusted” hospital outcomes. Circulation 117:1955–1963
Cevenini G, Barbini P (2010) A bootstrap approach for assessing the uncertainty of outcome probabilities when using a scoring system. BMC Med Inform Decis Mak 10:45
Lemeshow S, Hosmer DW Jr (1982) A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol 115:92–106
Hollis S, Yates DW, Woodford M, Foster P (1995) Standardized comparison of performance indicators in trauma: a new approach to case-mix variation. J Trauma 38:763–766
Glance LG, Osler T, Shinozaki T (2000) Effect of varying the case mix on the standardized mortality ratio and W statistic: a simulation study. Chest 117:1112–1117
Ashley A, Draper E, Fleming T, Lamming C, McKinney P, McShane P, Parslow R, Skinner S, Thiru K (2009) National Report of the Paediatric Intensive Care Audit Network 2006–2008. Leeds. http://www.picanet.org.uk/Documents/General/Annual%20report_2009/PICANet%20National%20Report%202006%20-%202008_new.pdf. Accessed 12 Nov 2011
Eulmesekian PG, Perez A, Minces PG, Ferrero H (2007) Validation of pediatric index of mortality 2 (PIM2) in a single pediatric intensive care unit of Argentina. Pediatr Crit Care Med 8:54–57
Imamura T, Nakagawa S, Goldman RD, Fujiwara T (2012) Validation of pediatric index of mortality 2 (PIM2) in a single pediatric intensive care unit in Japan. Intensive Care Med 38:649–654
Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J, Gottesman R, Joffe A, Pfenninger J, Hubert P, Lacroix J, Leclerc F (2003) Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 362:192–197
Metnitz B, Schaden E, Moreno R, Le Gall JR, Bauer P, Metnitz PG (2009) Austrian validation and customization of the SAPS 3 admission score. Intensive Care Med 35:616–622
Bakhshi-Raiez F, Peek N, Bosman RJ, de Jonge E, de Keizer NF (2007) The impact of different prognostic models and their customization on institutional comparison of intensive care units. Crit Care Med 35:2553–2560
Gregory CJ, Nasrollahzadeh F, Dharmar M, Parsapour K, Marcin JP (2008) Comparison of critically ill and injured children transferred from referring hospitals versus in-house admissions. Pediatrics 121:e906–e911
Alexander J, Tregea S, Slater A (2010) Report of the Australian and New Zealand Paediatric Intensive Care Registry 2009. Available at http://www.anzics.com.au/core/anzpicr?start=2. Accessed 10 Sept 2011
Straney LD, Clements A, Alexander J, Slater A (2010) Measuring efficiency in Australian and New Zealand paediatric intensive care units. Intensive Care Med 36:1410–1416
Haub C (2010) 2010 world population data sheet. Population Reference Bureau, Washington, DC. http://www.prb.org/pdf10/10wpds_eng.pdf. Accessed 4 May 2011
Beyene J, Atenafu EG, Hamid JS, To T, Sung L (2009) Determining relative importance of variables in developing and validating predictive models. BMC Med Res Methodol 9:64
Murphy-Filkins R, Teres D, Lemeshow S, Hosmer DW (1996) Effect of changing patient mix on the performance of an intensive care unit severity-of-illness model: how to distinguish a general from a specialty intensive care unit. Crit Care Med 24:1968–1973
Metnitz B, Metnitz PG, Bauer P, Valentin A (2009) Patient volume affects outcome in critically ill patients. Wien Klin Wochenschr 121:34–40
Glance LG, Szalados JE (2002) Benchmarking in critical care: the road ahead. Chest 121:326–328
Macrae D (2009) Conducting clinical trials in pediatrics. Crit Care Med 37:S136–S139
Spiegelhalter D (2002) Funnel plots for institutional comparison. Qual Saf Health Care 11:390–391
Acknowledgments
The authors thank Phil McShane (Paediatric Epidemiology Group, Centre for Epidemiology and Biostatistics, University of Leeds, Leeds, UK) for his help in the statistical analysis. French database: Grant from the French ministry of Health. UK database: PICANet is funded by the National Clinical Audit and Patient Outcomes Programme via Healthcare Quality Improvement Partnership (HQIP), Health Commission Wales Specialised Services, NHS Lothian/National Service Division NHS Scotland, the Royal Belfast Hospital for Sick Children, Our Lady’s Children’s Hospital, Crumlin, Children’s University Hospital, Temple Street and The Harley Street Clinic, London.
Conflicts of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Groupe Francophone de Réanimation et Urgences Pédiatriques (GFRUP): The members of the GFRUP who participated in this study are listed in the Appendix.
Paediatric Intensive Care Audit Network (PICANet): We are grateful to all the audit clerks, secretaries, nurses and doctors who support and contribute to PICANet from their own PICUs, the Paediatric Intensive Care Society, the Paediatric Intensive Care Society Study Group, the PICANet Steering Group and the PICANet Clinical Advisory Group.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2012_2580_MOESM1_ESM.doc
Fig.1 Description of the study’s design.PIM paediatric index of mortality, PICU paediatric intensive care unit. Fig. 2 Calibration plots in GB and FS PICUs. Plots show the observed risk by expected risk in deciles of expected risk using a log scale. The Hosmer–Lemeshow test indicated lack of fit for GB PIM2 score (p = 0.0011), moderate fit for FS PIM2 score (p = 0.07) and GB-Rec-PIM2 score (p = 0.06) and adequate fit for FS-Rec-PIM2 (p = 0.33).PIM paediatric index of mortality.Fig. 3 Relationship between admission per month and standardized mortality ratio in the FS (a) and GB (b) PICUs. Supplementary material 1 (DOC 285 kb)
Appendix
Appendix
Members of the GFRUP who participated D. Biarent (Bruxelles, Belgium), T. Blanc (Rouen, France), S. Cantagrel (Tours, France), R. Cremer (Lille, France), S. Dauger (Paris, France), P. Desprez (Strasbourg, France), M. Dobrzynski (Brest, France), G. Emériaud (Grenoble, France), P. Hubert (Paris, France), C. Milesi (Montpellier, France), S. Renolleau (Paris, France), M. Roque-Gineste (Toulouse, France), O. Noizet-Yverneau (Reims, France), D. Stamm (Lyon, France), I. Wroblewski (Besançon, France).
Participating French-speaking hospitals Data were collected in the French NPICU/PICUs of the following centres: American Memorial Hospital, CHU de Reims, France; Hôpital Charles Nicolle, CHU de Rouen, France; Hôpital Arnaud de Villeneuve, CHU de Montpellier, France; Hôpital Clocheville, CHU de Tours, France; Hôpital des enfants, CHU de Toulouse, France; Hôpital Hautepierre, CHU de Strasbourg, France; Hôpital Jeanne de Flandre, CHU de Lille, France; Hôpital Femme Mère-enfant, Hospices Civils de Lyon, France; Hôpital Morvan, CHU de Brest, France; Hôpital Necker, Assistance Publique-Hôpitaux de Paris, France; Hôpital Nord, CHU de Grenoble, France; Hôpital Reine Fabiola, Bruxelles, Belgium; Hôpital Robert Debré, Assistance Publique-Hôpitaux de Paris, France; Hôpital Saint Pierre, CHU de Besançon, France; Hôpital Trousseau, Assistance Publique-Hôpitaux de Paris, France.
Participating NHS trusts and hospitals
Addenbrooke’s NHS Trust: Addenbrooke’s Hospital
Bart’s and the London NHS Trust: Bart’s and The Royal London
Birmingham Children’s Hospital NHS Trust: Diana, Princess of Wales Children’s Hospital
Brighton & Sussex University Hospitals NHS Trust: Royal Alexandra Hospital for Sick Children
Cardiff and Vale NHS Trust: University Hospital of Wales
Central Manchester and Manchester Children’s University Hospitals NHS Trust: Royal Manchester Children’s Hospital
Children’s University Hospital, Temple Street, Dublin
Great Ormond Street Hospital for Children NHS Trust: Great Ormond Street Hospital for Sick Children
Guy’s & St. Thomas’ Hospital NHS Trust: Evelina Children’s Hospital
Hull & East Yorkshire Hospitals NHS Trust: Hull Royal Infirmary
King’s College Hospital NHS Trust: King’s College Hospital
Leeds Teaching Hospitals NHS Trust: Leeds General Infirmary, St. James University Hospital
Our Lady’s Children’s Hospital, Crumlin, Dublin
Newcastle upon Tyne Hospitals NHS Trust: Great Northern Children’s Hospital (formerly Newcastle General Hospital and the Royal Victoria Infirmary). Freeman Hospital
Oxford Radcliffe Hospitals NHS Trust: John Radcliffe Hospital
Queen’s Medical Centre Nottingham University NHS Trust: Queen’s Medical Centre
Royal Brompton and Harefield NHS Trust: Royal Brompton Hospital
Royal Liverpool Children’s NHS Trust: Alder Hey Hospital
Royal Group of Hospitals and Dental Hospital HSS Trust, Belfast Hospital for Sick Children
Sheffield Children’s NHS Trust: Sheffield Children’s Hospital
Southampton University Hospitals NHS: Trust Southampton General Hospital
South Tees Hospitals NHS Trust: James Cook University Hospital
St. George’s Healthcare NHS Trust: St. George’s Hospital
St. Mary’s NHS Trust: St. Mary’s Hospital
The Harley Street Clinic, London
The Lewisham Hospitals NHS Trust: University Hospital, Lewisham (to July 2010)
University Hospitals Bristol NHS Foundation Trust: Bristol Royal Hospital for Children
University Hospitals of Leicester NHS Trust: Leicester Glenfield Hospital, Leicester Royal Infirmary
University Hospital of North Staffordshire NHS Trust: Stoke on Trent City General
Rights and permissions
About this article
Cite this article
Leteurtre, S., Grandbastien, B., Leclerc, F. et al. International comparison of the performance of the paediatric index of mortality (PIM) 2 score in two national data sets. Intensive Care Med 38, 1372–1380 (2012). https://doi.org/10.1007/s00134-012-2580-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2580-6