Abstract
Purpose
The D allele of the insertion/deletion (I/D) polymorphism of a 287-bp sequence in the angiotensin-converting enzyme (ACE) gene has been associated with an increased activity of this enzyme. Its role in susceptibility to acute respiratory distress syndrome (ARDS) has not been well defined. We hypothesized that ACE I/D genotype in pediatrics is associated with ARDS and plasma levels of angiotensin II.
Methods
Prospective case–control study in patients under 15 years of age from a mixed Chilean population. Sixty patients with ARDS and 60 controls were included. Association between ACE genotype and ARDS was evaluated as the primary outcome; mortality and severe hypoxemia were examined as secondary outcomes. Plasma angiotensin-II concentration was measured by immunoassay at admission.
Results
Frequency of ACE I/D genotype was similar in ARDS and control groups (p = 0.18). In the ARDS group, severe hypoxemia was less frequent in D allele carriers (p < 0.05). Plasma angiotensin-II levels were associated with genotype in the ARDS group, but not controls, being higher in D allele carriers (p = 0.016).
Conclusion
These data do not support the association between ACE I/D genotype and ARDS, although severe hypoxemia was less frequent in D allele carriers. ACE I/D polymorphism modified angiotensin-II levels in pediatric ARDS, but its pathogenic role is not well understood and needs to be addressed in future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute respiratory distress syndrome (ARDS) is the most severe form of respiratory failure. It is considered the final path for many lung insults, but the exact mechanisms implicated in its development are not completely understood. Eventually, any acute lung insult may result in respiratory failure, but only a small percentage of subjects, even when exposed to the same insult, develop ARDS [1, 2]. On this basis, genetic factors have been associated with increased risk of developing ARDS. Angiotensin-converting enzyme (ACE) is involved in intravascular volume and systemic blood pressure regulation [3]. Experimental data suggest that an increase in ACE activity could be deleterious to patients with ARDS. High levels of ACE and angiotensin (AT) II, its main biological effector, have been associated with increased inflammatory response and impaired lung parenchyma remodeling [4–8]. There has been a growing interest in ACE polymorphisms and risk of ARDS. The D allele of the insertion (I)/deletion (D) polymorphism, a 287-bp fragment in intron 16 of the ACE gene, has been associated with higher plasma and tissue activity of this enzyme in Caucasian populations [9, 10], although there are differences in others ethnic groups [11]. The D allele has been associated with an increased risk of developing ARDS in critically ill adults [12, 13], but this association has not been found in other studies [14]. In children, there is only one study that found no significant difference in D allele frequency between patients with and without acute hypoxic respiratory failure [15].
We hypothesized that the presence of the D allele would increase susceptibility to ARDS in pediatric patients and be associated with higher plasma angiotensin-II concentrations.
Methods
Patients, definitions, and data collection
Approval was obtained from the Ethics Research Committee at Servicio de Salud Metropolitano Suroriente. Written informed consent was obtained from parents or legal guardians according to the Declaration of Helsinki’s guidelines. This was a case–control study of pediatric patients with ARDS. Patients were prospectively recruited from a mixed Chilean population consulting at a single center (Hospital Padre Hurtado’s Pediatric Service) during the period from 1 March 2008 to 31 July 2009. Inclusion criteria were age up to 15 years and admission due to pulmonary disease. The case group included all patients admitted to the Critical Care Area who met the inclusion criteria of the American-European Consensus Conference (AECC) on ARDS [16]. The control group included patients admitted to the general ward with pneumonia, not fulfilling ARDS criteria, and for whom the attending physician had requested a blood sample analysis during their hospital stay. Exclusion criteria were presence of congenital cardiac disease, chronic respiratory failure at the time of developing ARDS, immunodeficiency, malignancies, systemic immunosuppressive drug therapy other than corticosteroids, ACE inhibitors use, persistent pulmonary hypertension of the newborn, and corrected gestational age less than 34 weeks at birth. To assess severity in the case group, pediatric index of mortality 2 (PIM2) [17], pediatric logistic organ dysfunction (PELOD) [18], and lung injury score (LIS) [19] were recorded during the first 24 h after ARDS was diagnosed. Severe hypoxemia was defined as persistent PaO2/FiO2 less than 100 mmHg for at least 12 h. Sixty-day mortality and days on mechanical ventilation were recorded as well.
Blood sampling
After informed consent was obtained, blood samples were collected for DNA extraction and plasma storage.
ACE genotyping
Patients were genotyped for the I/D polymorphism using a three-primer method [20] yielding amplification products of 65 bp (I allele) and 84 bp (D allele). The DD genotype was confirmed by a second polymerase chain reaction (PCR), because the D allele is preferentially amplified in heterozygous samples. All DD genotype samples were negative for I allele-specific PCR. Staff involved in patient care and management was blinded to patient genotype throughout the study and personnel involved in genotyping were blinded to case–control status.
Angiotensin-II assay
For AT-II detection in plasma, a commercial AT-II enzyme immunoassay kit from SPI-Bio (Montigny le Bretonneux, France) was used [21]. Total AT-II values were directly calculated on the internal calibration curve and corrected according the original volume of plasma extracted. Personnel involved in AT-II measurement were also blinded to clinical data, genotype, and case–control status.
Data and statistical analysis
Estimated sample size was 60 patients per group to observe a difference of greater than 30% in the allelic frequencies with an α error of 0.05 and a β error no greater than 0.2, based on a known 0.43 D allele frequency among healthy adult Chileans [22]. The chi-square (χ 2) test was used to compare the observed frequency of each allele and genotype with the expected frequency for a population in Hardy–Weinberg equilibrium and to compare the frequency of alleles and genotypes between the ARDS group and the control group. To evaluate the recessive or dominant effect of the D allele, we independently compared the frequency of D allele carriers (DD and ID) and I allele carriers (II and ID) with homozygous subjects. Secondary outcomes were assessed with χ 2 test, odds ratio (OR), and 95% confidence intervals (CI). Continuous data were evaluated with Anderson–Darling test for normality and Kruskall–Wallis or Student’s t test were applied as required. Statistical analysis was performed with the Stata® program (Statacorp, Texas, USA). For all tests statistical significance was set at a p value of less than 0.05.
Results
A total of 60 cases and 60 controls were enrolled and genotyped. Both groups were comparable in their demographic characteristics (Table 1).
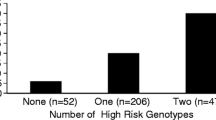
Primary outcome: association between genotype and ARDS
D allele frequency was 0.37 in the overall group, similar to that previously reported in a Chilean population [22]. There was no difference in the frequency of D allele which was 0.31 in controls and 0.43 in the ARDS group (p = 0.08, OR 1.87, 95% CI 0.84–4.18). The genotype distribution in control and ARDS groups was not different (p = 0.18) (Table 2, top). We found no evidence of statistically significant difference among controls and ARDS subjects with D allele carriers (DD/ID vs. II, p = 0.19) and I allele carriers (DD vs. ID/II, p = 0.09). Subgroup analysis comparing pneumonia-ARDS and controls did not show difference in genotype distribution and allele frequencies (Table 2, bottom).
Secondary outcomes
Among subjects with ARDS, there was no significant association between ACE genotype and PIM2, PELOD, or LIS scores and days on mechanical ventilation (Table 3). Severe hypoxemia was present in 17% of cases. The I allele was associated with severe hypoxemia (OR 5.33, 95% CI 1.65–20.04) (Table 4).
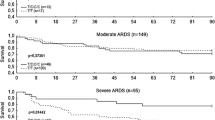
Angiotensin II
Plasma AT-II levels were 229 (157–319) pg/ml in controls and 134 (18–353) pg/ml in ARDS patients (p = 0.15). Subjects homozygous for I allele had lower AT-II plasma levels in the ARDS group than in controls (29 [6–171] and 200 [30–291] pg/ml, respectively; p = 0.048). No differences in AT-II levels were found between cases and controls in other genotypes. In analysis within groups, D allele presence was associated with higher AT-II levels in both control and ARDS groups (Fig. 1). There was no significant association between plasma AT-II levels and secondary outcomes (data not shown).
Discussion
Our data do not support an association between the ACE I/D polymorphism and the presence of pediatric ARDS. The D allele frequency was similar in ARDS and control groups. The D allele was associated with increased plasma AT-II levels in cases and controls, but paradoxically with less severe hypoxemia in patients with ARDS.
The D allele has been previously associated with alveolar-capillary interface dysfunction phenotypes [13]. Recent studies in critically ill adults have found a significant association between DD genotype and ARDS prevalence compared to the general intensive care unit (ICU) population and also higher mortality rates [12, 23]. Nevertheless, as in many genetic association studies, there are conflicting data from other negative results [14]. ACE I/D polymorphism has been studied in many diseases in children but only one study, that by Plunkett et al. [15], looked at its association with respiratory failure. It was limited to Caucasian populations and concluded that the D allele does not predispose children to acute hypoxemic respiratory failure (AHRF). Patients included in that study were heterogeneous, 54% had infection, and most were admitted for conditions other than pneumonia (encephalitis/meningitis, bronchiolitis, and bacterial septic shock). Also, primary outcome was infrequent, only 14% (n = 30) had AHRF and 6% (n = 13) had ARDS. Our case definition was children fulfilling AECC criteria for ARDS, focusing on patients with severe lung dysfunction. AECC criteria have a poor correlation with specific histological findings of ARDS (i.e., diffuse alveolar damage), but at present no better diagnostic test is available, and these criteria are routinely used in clinical practice and in patient selection for clinical trials [24]. Given the socioeconomic characteristics of our population, all but one of the cases and all the controls had an infectious etiology. Despite our different design, case definition, etiologies, and ethnic background, our results are in accordance with Plunkett et al. in reaffirming the lack of association between ACE I/D genotype and pediatric ARDS.
On the basis of secondary outcomes, surprisingly we found that D allele carriers had less severe hypoxemia. As mentioned before, D allele has been associated with increased ACE activity in plasma [10]. But ACE is also present in endothelial cells of lung capillaries as well as other vascular beds, such as the kidneys, brain, heart, and skeletal muscle. Experimental data support that tissue ACE activity may be more important than plasma levels in ALI/ARDS pathogenesis [25, 26]. To date ACE I/D polymorphism association with ACE activity in lung tissue and endothelium has not been studied in humans. In addition, severe hypoxemia and lung dysfunction were not addressed in previous studies of ACE I/D genotype and ARDS, reporting almost exclusively mortality [12, 14, 23]. Two of them found association between D allele presence and higher mortality [12, 23]. We found no significant association between genotype and mortality of patients with ARDS, which is not surprising because this study was not powered to examine this. It is important to note that clinical studies have reported this discrepancy between severe hypoxemia and mortality. Hypoxemia itself is the cause of death in only 9–27% in different series of patients with ARDS, and multiorgan failure is the major cause of the remaining deaths [24, 27, 28]. Mortality was 9% in the ARDS group, similar to other pediatric studies [29, 30] and with mortality predicted by PIM2 and PELOD scores. Currently, we do not have enough clinical information to relate specific ACE polymorphisms to a given prognosis for pediatric ARDS. A cohort study will be required to determine this.
Another significant finding is the association between ACE genotype and AT-II plasma levels at admission. As in previous studies, we found a wide distribution of plasma AT-II in all genotypes and both groups, control and ARDS. We measured AT-II as a surrogate of ACE plasmatic activity, being the most important biological effector of the renin–angiotensin system (RAS) in pulmonary circulation. AT-II has been shown to be involved in the development of pulmonary edema, increasing vascular tone and vascular permeability [31, 32]. Several authors described a reduction in ACE plasma level in patients with ARDS [33–36], reflecting lung damage severity (decreased synthesis) and impairment of systemic release of the enzyme [25]. We found lower AT-II plasma levels at admission in subjects with ACE II genotype, being more strikingly reduced in ARDS patients. The former result may be due to a lower ACE activity determined by the ACE I/D polymorphism genotype (genetic factor) and the latter due to an additive effect of the disease.
As pointed out by many authors, conclusions from studies in critically ill adults cannot be extrapolated to the pediatric population, not only because of the underlying pathophysiologic differences between adults and children, but also because ARDS triggering insults in the former are usually extrapulmonary, such as sepsis and trauma, whereas in children direct pulmonary insult, such as pneumonia, are the main causes of ALI/ARDS cases [37]. In extrapulmonary ARDS, systemic RAS activation leading to increased vascular permeability may play a major role, contrary to primary ARDS in which ACE local activity and AT-II nonvascular effects (induction of coagulation, apoptosis, and fibrosis pathway, generation of reactive oxygen species, chemotaxis of neutrophils, among others) may be more important. Also, the role of AT-II in ARDS may not be limited to the acute phase. Locally activation of RAS and AT-II production may be involved in the fibroproliferative phase of the disease due to profibrotic properties [32]. Reaffirming this hypothesis, a study in preterm infants associated the D allele of the ACE gene with increased risk and severity of pulmonary sequela after a neonatal ARDS [38].
This study has some limitations. The ACE I/D polymorphism has only been demonstrated to be functional in Caucasians [10]. Data linking this polymorphism and ACE activity in other ethnic groups are either lacking or suggest the polymorphism is nonfunctional [32]. As this polymorphism lies within an intron, it is unlikely to be a functional variant itself, but rather in linkage disequilibrium with a functional variant either within the ACE gene or in a neighboring region of the chromosome [39], or alternatively, it may have a regulatory function. Also, the current view of RAS is a complex network of enzymes and substrates, including ACE 2 (homologue enzyme of ACE that acts on different peptide substrates) and other intermediate substrates with synergism or antagonism with AT-II [31, 32]. The final effect of AT-II is related to a balance between all of these components and is not possible to correlate values with a single effect in vivo. Additionally, AT-II was measured only at admission, so it was not possible to analyze its tendency over time. Power and sample size were not calculated to find differences in mortality.
In conclusion, these data do not support association between ACE I/D genotype and pediatric ARDS, although severe hypoxemia was less frequent in D allele carriers. ACE I/D polymorphism modified AT-II levels in pediatric ARDS, but its pathogenic role is not well understood and needs to be addressed in future trials.
References
Hudson LD, Milberg JA, Anardi D, Maunder RJ (1995) Clinical risks for development of the acute respiratory distress syndrome. Am J Respir Crit Care Med 151:293–301
Fowler AA, Hamman RF, Good JT, Benson KN, Baird M, Eberle DJ, Petty TL, Hyers TM (1983) Adult respiratory distress syndrome: risk with common predispositions. Ann Intern Med 98:593–597
Erdos EG, Skidgel RA (1987) The angiotensin I-converting enzyme. Lab Invest 56:345–348
Kiely DG, Cargill RI, Lipworth BJ (1995) Acute hypoxic pulmonary vasoconstriction in man is attenuated by type I angiotensin II receptor blockade. Cardiovasc Res 30:875–880
Dimmeler S, Rippmann V, Weiland U, Haendeler J, Zeiher AM (1997) Angiotensin II induces apoptosis of human endothelial cells. Protective effect of nitric oxide. Circ Res 81:970–976
Marshall RP, McAnulty RJ, Laurent GJ (2000) Angiotensin II is mitogenic for human lung fibroblasts via activation of the type 1 receptor. Am J Respir Crit Care Med 161:1999–2004
Uhal BD, Gidea C, Bargout R, Bifero A, Ibarra-Sunga O, Papp M, Flynn K, Filippatos G (1998) Captopril inhibits apoptosis in human lung epithelial cells: a potential antifibrotic mechanism. Am J Physiol 275:1013–1017
Marshall RP, Gohlke P, Chambers RC, Howell DC, Bottoms SE, Unger T, McAnulty RJ, Laurent GJ (2004) Angiotensin II and the fibroproliferative response to acute lung injury. Am J Physiol Lung Cell Mol Physiol 286:156–164
Tiret L, Rigat B, Visvikis S, Breda C, Corvol P, Cambien F, Soubrier F (1992) Evidence, from combined segregation and linkage analysis, that a variant of the angiotensin I-converting enzyme (ACE) gene controls plasma ACE levels. Am J Hum Genet 51:197–205
Rigat B, Hubert C, Alhenc-Gelas F, Cambien F, Corvol P, Soubrier F (1990) An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest 86:1343–1346
Bloem LJ, Manatunga AK, Pratt JH (1996) Racial difference in the relationship of an angiotensin converting enzyme gene polymorphism to serum angiotensin I-converting enzyme activity. Hypertension 27:62–66
Marshall RP, Webb S, Bellingan GJ, Montgomery HE, Chaudhari B, McAnulty RJ, Humphries SE, Hill MR, Laurent GJ (2002) Angiotensin converting enzyme insertion/deletion polymorphism is associated with susceptibility and outcome in acute respiratory distress syndrome. Am J Respir Crit Care Med 166:646–650
Yende S, Quasney MW, Tolley EA, Wunderink RG (2004) Clinical relevance of angiotensin-converting enzyme gene polymorphisms to predict risk of mechanical ventilation after coronary artery bypass graft surgery. Crit Care Med 32:922–927
Villar J, Flores C, Perez-Mendez L, Maca-Meyer N, Espinosa E, Blanco J, Sanguesa R, Muriel A, Tejera P, Muros M, Slutsky AS (2008) Angiotensin converting enzyme insertion/deletion polymorphism is not associated with susceptibility and outcome in sepsis and acute respiratory distress syndrome. Intensive Care Med 34:488–495
Plunkett A, Agbeko RS, Li K, Humphries SE, Klein NJ, Peters MJ (2008) Angiotensin-converting enzyme D allele does not influence susceptibility to acute hypoxic respiratory failure in children. Intensive Care Med 34:2279–2283
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Slater A, Shann F, Pearson G (1999) PIM 2: a revised version of the paediatric index of mortality. Intensive Care Med 29:278–285
Leteurtre S, Martinot A, Duhamel A, Gauvin F, Grandbastien B, Nam TV, Proulx F, Lacroix J, Leclerc F (1999) Development of a pediatric multiple organ dysfunction score: use of two strategies. Med Decis Making 19:399–410
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138:720–723
O’Dell SD, Humphries SE, Day IN (1995) Rapid methods for population-scale analysis for gene polymorphisms: the ACE gene as an example. Br Heart J 73:368–371
Volland H, Pradelles P, Ronco P, Azizi M, Simon D, Créminon C, Grassi J (1999) A solid-phase immobilized epitope immunoassay (SPIE-IA) permitting very sensitive and specific measurement of angiotensin II in plasma. J Immunol Methods 228:37–47
Jalil JE, Piddo AM, Cordova S, Chamorro G, Braun S, Jalil R, Vega J, Jadue PL, Lavandero S, Lastra P (1999) Prevalence of the angiotensin I converting enzyme insertion/deletion polymorphism, plasma angiotensin converting enzyme activity, and left ventricular mass in a normotensive Chilean population. Am J Hypertens 12:697–704
Jerng JS, Yu CJ, Wang HC, Chen KY, Cheng SL, Yang PC (2006) Polymorphism of the angiotensin-converting enzyme gene affects the outcome of acute respiratory distress syndrome. Crit Care Med 34:1001–1006
Esteban A, Fernández-Segoviano P, Frutos-Vivar F, Aramburu JA, Nájera L, Ferguson ND, Alía I, Gordo F, Ríos F (2004) Comparison of clinical criteria for the acute respiratory distress syndrome with autopsy findings. Ann Intern Med 141:440–445
Orfanos S, Armaganidis A, Glynos C, Psevdi E, Kaltsas P, Sarafidou P, Catravas J, Dafni U, Langleben D, Roussos C (2000) Pulmonary capillary endothelium-bound angiotensin-converting enzyme activity in acute lung injury. Circulation 102:20112018
Jiang JS, Wang LF, Chou HC, Chen CM (2007) Angiotensin-converting enzyme inhibitor captopril attenuates ventilator-induced lung injury in rats. J Appl Physiol 102:2098–2103
Arroliga AC, Ghamra ZW, Pérez-Trepichio A, Pérez-Trepichio P, Komara JJ Jr, Smith A, Wiedemann HP (2002) Incidence of ARDS in an adult population of Northeast Ohio. Chest 121:1972–1976
Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP (2005) Causes and timing of death in patients with ARDS. Chest 128:525–532
Wolfler A, Calderoni E, Ottonello G, Conti G, Baroncini S, Santuz P, Vitale P, Salvo I, Study Group SISPE (2011) Daily practice of mechanical ventilation in Italian pediatric intensive care units: a prospective survey. Pediatr Crit Care Med 12:141–146
Curley MA, Hibberd PL, Fineman LD, Wypij D, Shih MC, Thompson JE, Grant MJ, Barr FE, Cvijanovich NZ, Sorce L, Luckett PM, Matthay MA, Arnold JH (2005) Effect of prone positioning on clinical outcomes in children with acute lung injury: a randomized controlled trial. JAMA 294:229–237
Victorino GP, Newton CR, Curran B (2002) Effect of angiotensin II on microvascular permeability. J Surg Res 104:77–81
Imai Y, Kuba K, Penninger JM (2007) Angiotensin-converting enzyme 2 in acute respiratory distress syndrome. Cell Mol Life Sci 64:2006–2012
Casey L, Krieger B, Kohler J, Rice C, Oparil S, Szidon P (1981) Decreased serum angiotensin converting enzyme in adult respiratory distress syndrome associated with sepsis: a preliminary report. Crit Care Med 9:651–654
Fourrier F, Chopin C, Wallaert B, Wattre P, Mangalaboyi J, Durocher A, Dubois D, Wattel F (1983) Angiotensin-converting enzyme in human adult respiratory distress syndrome. Chest 83:593–597
Fourrier F, Chopin C, Wallaert B, Mazurier C, Mangalaboyi J, Durocher A (1985) Compared evolution of plasma fibronectin and angiotensin-converting enzyme levels in septic ARDS. Chest 87:191–195
Idell S, Kueppers F, Lippmann M, Rosen H, Niederman M, Fein A (1987) Angiotensin converting enzyme in bronchoalveolar lavage in ARDS. Chest 91:5256
Rodriguez Martinez CE, Guzman MC, Castillo JM, Sossa MP, Ojeda P (2006) Evaluation of clinical criteria for the acute respiratory distress syndrome in pediatric patients. Pediatr Crit Care Med 7:335–339
Kazzi SN, Quasney MW (2005) Deletion allele of angiotensin-converting enzyme is associated with increased risk and severity of bronchopulmonary dysplasia. J Pediatr 147:818–822
Zhu X, McKenzie CA, Forrester T, Nickerson DA, Broeckel U, Schunkert H, Doering A, Jacob HJ, Cooper RS, Rieder MJ (2000) Localization of a small genomic region associated with elevated ACE. Am J Hum Genet 67:1144–1153
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cruces, P., Díaz, F., Puga, A. et al. Angiotensin-converting enzyme insertion/deletion polymorphism is associated with severe hypoxemia in pediatric ARDS. Intensive Care Med 38, 113–119 (2012). https://doi.org/10.1007/s00134-011-2381-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2381-3