Abstract
Introduction
Acute kidney injury (AKI) is a common and serious complication increasing morbidity and mortality from all causes of hospital admission. We have previously shown that AKI decreases midazolam metabolism, a substrate of the cytochrome P450 3A (CYP3A) enzymes and our primary aim was to determine if this effect is dependent on the severity of AKI. We also present preliminary data on the functional impact of different genotypes of CYP3A.
Methods
Critically ill patients at risk of AKI and admitted to a general intensive care unit were categorised after initial resuscitation according to the RIFLE criteria for AKI. Midazolam (1mg) was administered and the serum concentration of midazolam measured at 4 h. Samples were taken for CYP3A genotyping.
Results
Seventy-three patients were assigned to categories R, I and F of the RIFLE criteria or C (controls). Midazolam concentrations (ng mL−1) increased significantly (p = 0.002) as the severity of AKI worsened [control 3.1 (1.4–5.9), risk 4.7 (1.3–10.3), injury 3.9 (2.0–11.1) and failure 6.8 (2.2–113.6)] and were predicted by the duration of AKI (p = 0.000) and γ-glutamyl transferase (p = 0.005) concentrations. Increasing BMI negatively predicted the midazolam concentration (p = 0.001). Preliminary data suggest this effect is diminished if the patient expresses functional CYP3A5.
Conclusion
Increasing severity and duration of AKI are associated with decreased midazolam elimination. We propose that this is caused by impaired CYP3A activity secondary to AKI. The exact mechanism remains to be elucidated. This may have important implications for our drug treatment of critically ill patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a common and important problem for hospital patients and is associated with increased risk of death [1, 2]. Recent retrospective analysis of outcome from AKI in all hospital admissions revealed that an acute increase in creatinine (>26 μmol L−1), even if recovered to normal and regardless of underlying cause for admission, was associated with poor outcome compared to patients with normal renal function or indeed patients admitted with chronic kidney disease (CKD) [3]. With the development of consensus criteria [4, 5] for the description of AKI, there is increasing recognition of cross-talk between kidneys and other organs including cardiorenal, neurorenal, respiratory-renal and heptaorenal interactions [6–9]. In a recent pilot study, we presented preliminary data to suggest that AKI may impair the hepatic metabolism of midazolam, but we were unable to relate this to the severity of AKI [10]. A similar phenomenon has been described for CKD [11–14].
The pharmacokinetics and pharmacodynamics of drugs administered to critically ill patients are often unpredictable and complex, and efficacy and toxicity of drugs may be dose-critical. However, most dosing regimens are based on data extrapolated from studies in normal individuals or those experiencing chronic disease states or are based on empirical principles. The effects of acute organ failures are not fully understood, and the impact of AKI on hepatic drug metabolism remains to be characterized.
The cytochrome P450 3A (CYP3A) enzymes are the most abundantly expressed subfamily of cytochrome P450 enzymes. The human CYP3A gene locus comprises four functional genes, CYP3A4, CYP3A5, CYP3A7 and CYP3A43, and two pseudogenes [15]. Only CYP3A4 and CYP3A5 are functionally relevant in adults and are responsible for metabolism of >50% of all drugs [16]. They differ in terms of substrate intrinsic clearance and regioselectivity [17]. The majority of activity of these enzymes occurs in the liver although they are also expressed in intestinal mucosa, lung and kidney. Intestinal CYP3A activity has a marked effect on the bioavailability of orally administered drugs, but following intravenous administration, the main determinant of drug metabolism is hepatic CYP3A enzyme content [18].
All adults express CYP3A4. Many single nucleotide polymorphisms (SNP) exist in the CYP3A4 gene, but all are present at low frequency (<1–2%) and do not relate to drug metabolism phenotype [19]. In contrast, individuals are either functional expressers or non-expressers of CYP3A5. The most frequent SNP is an A > G substitution within intron 3, known as CYP3A5*3 (6986 A > G). The substitution leads to improperly spliced CYP3A5 mRNA and a non-functional protein truncated at amino acid 102 [17]. Individuals with at least one wild-type allele (CYP3A5*1) are expressers and CYP3A5*3/*3 homozygotes are non-expressers of CYP3A5. When expressed, CYP3A5 represents >50% of total CYP3A activity [17]. The frequency of the allele CYP3A5*3 is 87% in Caucasians and 28% in African Americans [20] and accounts for differences in metabolism of CYP3A substrates observed among ethnic groups. Renal transplant recipients heterozygous or homozygous for CYP3A5*1 have a twofold lower dose-normalized blood concentration of tacrolimus than patients homozygous for CYP3A5*3 [21].
Measuring the the total systemic clearance of midazolam is an established in vivo method of probing CYP3A enzyme activity, and a single point determination of midazolam concentration 4 h after intravenous administration has been shown to be a safe and accurate representation of total midazolam exposure in healthy volunteers and critically ill patients [10, 15]. Our primary aim was to test the hypothesis that worsening AKI decreases the hepatic metabolism of midazolam by CYP3A enzymes. A secondary aim was to define the role of the CYP3A5 genotype on inhibition of hepatic drug metabolism in AKI.
Methods
Critically ill patients were enrolled from the general critical care unit of a London university hospital over a 1 year period (May 2008–May 2009). The unit admits 1,400 patients per year, including for elective surgery and emergency admissions (medical and surgical).
Approval for the study was granted by the Research Ethics Committee. Written assent for the patient to participate was obtained from a next of kin, in accordance with advice received from the Research Ethics Committee in relation to the Mental Capacity Act of 2006 (UK).
Patients
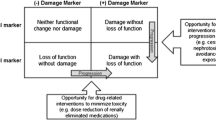
All patients requiring >48 h admission to the general intensive care unit (GICU) were reviewed and were considered at immediate risk of AKI if they had either a urine output <0.5 mL kg−1 h−1 or a serum creatinine >110 μmol L−1 (Fig. 1). Patients then underwent a 24 h period of resuscitation by clinicians not involved in the study, before allocation to one of the RIFLE criteria: risk (R), injury (I) and failure (F) at the start of the 4 h study period [4]. Seventeen patients did not fulfil any of the RIFLE criteria after resuscitation and were designated controls.
Exclusion criteria were (1) acute or chronic liver disease, (2) immediate requirement for renal replacement therapy, (3) renal transplantation, (4) pregnancy, (5) prior use of benzodiazepines (during current hospital admission) or (6) administration of major inhibitors (amiodarone, macrolide antibiotics, imidazole compounds) or inducers (rifampicin, phenytoin, dexamethasone) of CYP3A enzymes.
Length of time of AKI was estimated based on the time since baseline serum creatinine and/or normal urine output (if the patient was in hospital prior to AKI), or as time since admission to hospital, if admitted as an emergency.
Data collection
Patient length and weight were recorded and body mass index (BMI) and body surface area (BSA) calculated [22]. Baseline serum creatinine concentrations were established using the following methods: (1) from hospital admission blood tests if admitted prior to developing AKI, (2) from results recorded in the notes or by the patient’s general practitioner (GP) within the previous year, (3) if a previous result was unavailable and if renal function recovered to within normal range following the ICU stay, this value was used as the baseline. Using these methods a baseline creatinine measurement was obtained for all patients.
4 h study period
All patients had blood tests during the 4 h study period for renal biochemistry (urea, creatinine), serum electrolytes, alkaline phosphatase (ALP), alanine transaminase (ALT), gamma-glutamyl transferase (γ-GT), albumin, bilirubin and haematology including the international normalised ratio (INR) and a full blood count. Arterial blood was analysed for pH, partial pressure of oxygen (PaO2) and bicarbonate (HCO3 −) concentration. An ethylenediaminetetraacetic acid (EDTA) sample was taken for genotyping of CYP3A5.
Intravenous midazolam (1 mg) was given at time zero (T0) and two blood samples collected 4 h later (T4) for analysis of midazolam concentration and for repeat serum creatinine, urea and albumin.
Urine was collected for 4 h and a sample sent for spot albumin and creatinine concentrations. The 4 h creatinine clearance (4CrCl) (mL min−1) was calculated as U × V/P [U urine creatinine concentration (mg mL−1), V urine flow (mL min−1) and P plasma creatinine concentration (mg mL−1)]. 4CrCl was adjusted to the average BSA (1.73 m2).
Midazolam assay
Total serum midazolam concentration was determined by high performance liquid chromatography with tandem mass spectrometry (HPLC/MS/MS) using a Sciex API 4000™ (AME Bioscience, Norway). This is a standard method, based on one previously published [23] with in-house modifications such that deuterate midazolam is used as internal standard to give a much superior assay. Sample size was 100 μL, and the lower limit of quantitation (LLOQ) was set to 0.25 ng mL−1. The limit of detection (LOD) was 0.05 ng mL−1.
Urine creatinine was quantified by the Jaffe reaction and urine albumin by a turbidimetric assay.
Genotype at the CYP3A56986 A > G (CYP3A5*1/*3) SNP was determined by real-time PCR with fluorescently labelled hybridisation probes and melt curve analysis on a Roche Lightcycler 1.0 [21].
Power for this study was calculated from previous data published by this group [10]. Assuming a difference in midazolam concentration of 1.5 ng mL−1 between groups and using a standard deviation of 2.1, 15 patients per RIFLE criterion were required to achieve a power of 80% with a significance level (α, two-sided) of 0.05 for the primary aim.
Statistical analysis
All statistical analysis was done using SPSS® (v16.0). Changes with RIFLE criteria for non-parametric data were tested for significance using the Kruskal-Wallis test, and a two-tailed P value <0.05 was considered significant. A backward-selected linear multiple regression was employed to look for predictors of midazolam concentration.
Funding
Funding was obtained from the St George’s Research Fund.
Results
After excluding patients requiring urgent renal replacement therapy, 166 critically ill patients were considered at risk of AKI. Of these, 93 were excluded for the following reasons: (1) prescribed exclusion medications, (2) exposure to midazolam, or (3) permission was refused. In total 73 patients were studied, including 56 patients with AKI after initial resuscitation and 17 critically ill patients without AKI.
Patient characteristics
A summary of patient demographics is given in Table 1. Significant co-morbidities are listed and the Charlson co-mobidity score calculated. Patients who developed AKI were more likely to have an increased serum creatinine at baseline or a history of chronic renal impairment. There were no other significant differences between RIFLE categories.
Clinical variables on admission to the study are summarized in Table 2. The total Sequential Organ Failure Assessment (SOFA) score increased as renal function worsened but was entirely attributable to the deteriorating score for the renal component (Table 2).
Nineteen of 73 patients were genetically predicted to express functional CYP3A5 (heterozygous or homozygous for the CYP3A5*1 allele). All black (genetically sub-Saharan African) patients expressed at least one CYP3A5*1 allele compared to 18% of Caucasian patients. Ethnic groups were evenly distributed across the RIFLE criteria (Table 1).
Findings at T4
The renal and hepatic indices at T4 are shown (Table 3). There were no significant differences in pH, serum albumin, ALT, γ-GT, INR or bilirubin. ALP did increase significantly with worsening RIFLE criteria (P = 0.034).
Midazolam concentrations increased with the severity of AKI (Kruskal-Wallis, P = 0.002, Table 3). There were two major outliers who may have skewed the results in favour of the hypothesis with midazolam concentrations of 60.47 and 113.61 ng mL−1. Without these results the statistical significance persists (Fig. 2, P = 0.009).
The raw midazolam data were skewed, and in order to determine the predictive value of variables, the data were normalized by log10 transformation. The relationships between the log-transformed midazolam concentrations and predicting variables were tested using Pearson correlations, and significant results were entered into a backward-selected stepwise linear regression analysis. These included length of time with AKI, serum urea, serum creatinine, serum albumin, BMI, ALP and γ-GT. The results are summarized in Table 4. Length of time with AKI was the strongest predictor of the midazolam concentration. BMI was a negative predictor of midazolam concentration.
Figure 3 illustrates the increase in midazolam concentration as the RIFLE criteria worsen from controls to failure with patients classified by genotype.
Boxplot (median, interquartile range, minimum and maximum) of midazolam concentrations according to the RIFLE criteria and patient CYP3A genotype, excluding the two outliers in the F group. CYP3A5 genotypes: dotted squares CYP3A5*3/*3 (GG), hatched squares CYP3A5*1/*3 (AG), checked squares CYP3A5*1/*1 (AA). The single horizontal bars in the risk and injury categories represent single patients with CYP3A5*1/*1 genotype
Discussion
Acute kidney injury may reduce the hepatic metabolism of midazolam in critically ill patients who do not have underlying liver disease. Midazolam concentrations increased with worsening RIFLE category, and the length of time with AKI was predictive of this effect. We have hypothesised that AKI decreases the hepatic metabolism of midazolam via inhibition (functional or expressive) of the CYP3A4 and 5 enzymes, and our data are supportive of this. However, there are limitations to our method and coincidental hepatic impairment cannot be excluded as a cause.
Two patients had extremely high midazolam concentrations (60.47 and 113.61 ng mL−1). Both patients had severe renal dysfunction over a prolonged period, and an alternative explanation for the midazolam concentrations was not found. However, such results may skew the data and distort interpretation. Statistics were performed excluding these outliers, and the results and conclusions were not changed (data not presented).
Patients who had raised baseline serum creatinine concentrations were more likely to develop AKI. This is in keeping with previous observations that people with pre-existing CKD, however mild, are more at risk of developing AKI when critically ill [24].
Serum midazolam concentrations in vivo are determined by the dose administered, its volume of distribution (V d) and its elimination. It has been shown previously that renal impairment significantly increases the half-life of both midazolam and its metabolites [25] although the authors were unable to explain the mechanism by which the midazolam half-life was affected. We measured total midazolam concentration, using the UK standard. This method is calibrated with deuterate midazolam thus allowing low concentrations of midazolam to be detected with accuracy, minimising the required dose for midazolam but limiting our ability to detect metabolites.
Midazolam is highly protein bound (94–96%) predominantly to albumin, with little redistribution within red blood cells [26] and has a V d of 1.2–2.7 L kg−1, independently determined by adipose tissue, pH and plasma albumin concentrations [27]. None of these parameters differed significantly between RIFLE groups. Although we did not measure V d, critical illness, including AKI, would be expected to increase the V d for midazolam (decreased serum albumin and decreased pH) [28] thus decreasing the expected serum total midazolam concentration at T4. This is in opposition to our hypothesis, but nevertheless, we observed an increase in T4 serum midazolam with worsening AKI despite potential changes in V d. Indeed, it is possible this study underestimates the true magnitude of effect.
The BMI was significantly but negatively associated with serum midazolam concentrations in keeping with its effect on V d. We considered varying the dose of midazolam according to an assessment of adiposity, but two considerations made this impractical. First, assessing the amount of adipose tissue is difficult and imprecise [29, 30], and secondly, the dose of midazolam, for ethical and safety reasons, must be small and unlikely to cause clinical effect. This restricts dose variability according to the limits and accuracy of the method of detection.
In our study, serum urea concentration did not predict the midazolam concentration, but in patients with CKD, erythromycin (an alternative probe of CYP3A4 activity) elimination was decreased as urea increased [31]. The most likely reason for our study’s failure to find a relationship with urea is the complex perturbations of urea observed in critically ill patients. Urea concentrations depend on co-existing pathology (e.g. gastrointestinal haemorrhage and liver disease), hydration status and nutritional status making it a crude marker of poor renal perfusion.
Multivariate analysis showed that the duration of AKI was an important predictor of midazolam concentration although this cannot be separated from the severity of AKI, and the relative importance of each remains uncertain. However, if time is an important consideration it may provide a clue to the underlying mechanism, perhaps implying a change in gene expression and production of the enzyme rather than direct inhibition of the enzyme activity. This would be in keeping with data from CKD studies [13].
Serum alkaline phosphatase concentrations were significantly increased as the RIFLE criteria worsened, and γ-GT concentrations were predictive of midazolam concentrations. It is possible that coincidental liver impairment is the cause of the observed altered midazolam metabolism. However, patients with known acute or chronic liver disease were excluded, and the other important data are not supportive of severe liver dysfunction (e.g. INR, lactate, ALT). These tests however do lack both specificity and sensitivity for assessing liver metabolic and synthetic function in critically ill patients [32]. Alternatively, AKI may impact more widely on hepatic enzyme systems, in addition to CYP450 enzymes, than we have previously supposed. This warrants further investigation.
One confounding factor we were unable to address fully was the potential effect of hepatic blood flow. An ideal drug probe of CYP3A has an extraction ratio <0.3 and thus is unaffected by hepatic blood flow. Midazolam has an extraction ratio of between 0.33 and 0.95 (mean 0.55) [26]. Measuring liver blood flow is challenging in critically ill patients, the available methods being either indirect and imprecise, or invasive and complex [33]. In healthy volunteers, the relationship between midazolam clearance and blood flow has been investigated using the ‘MEG-X’ method (the appearance of monoethylglycinexylidide, a metabolite of lignocaine). Under normal conditions the clearance of lignocaine and midazolam is correlated, but in the presence of a CYP3A4 inhibitor, this correlation is lost [34]. In 36 patients we measured cardiac output and found no difference between categories of AKI, but whether this can be related to liver blood flow is uncertain. In sepsis, however, hepatic blood flow has been shown to change little, even in patients with raised cardiac output [35]. Overall there is a lack of extensive studies of hepatic blood flow in critically ill patients.
Midazolam as a drug probe has two major advantages: first it is metabolized exclusively by CYP3A, and second, it has a good safety profile at a dose which provides detectable samples. Erythromycin is the most established alternative probe [36] but its use has two problems. First, it demands a steady state of background carbon dioxide (CO2) production and elimination, and expired CO2 is highly variable in critically ill patients, affected by both underlying pathology and medical interventions [37]. Second, erythromycin elimination is affected by P-glycoprotein (pgp) activity, and this has been shown to be decreased in chronic renal impairment [38] whereas midazolam is unaffected by pgp. Alfentanil is another potential alternative; however the doses required are not insignificant for critically ill patients [39].
Although underpowered to make firm conclusions, our data do provide preliminary evidence enabling us to hypothesize that patients who have a CYP3A*1 allele, i.e. who express functional CYP3A5, metabolize midazolam faster than patients with the CYP3A5*3/*3 genotype, partially protecting them from the impact of AKI on CYP function.
The importance of these changes in enzyme activity, either through the effects of AKI or as a consequence of genotype variations, remains unknown in critically ill patients. However, in renal transplant patients, the administration of fluconazole (a potent CYP3A inhibitor) decreases tacrolimus metabolism. This effect is diminished in patients who express the CYP3A5*1 allele thus demanding less change to the dose of tacrolimus [40], and it is easy to envisage similarly important situations in the critically ill. The list of CYP3A substrates is large, and our evidence suggests that not only should we be considering patients’ genotype but also their renal function when dosing drugs eliminated by the liver. Understanding more about the effects of a patient’s illness on drug metabolism in combination with genotype may allow more efficient, individualized therapy.
References
James MT, Wald R, Bell CM, Tonelli M, Hemmelgarn BR, Waikar SS, Chertow GM (2010) Weekend hospital admission, acute kidney injury, and mortality. J Am Soc Nephrol 21:845–851
Kolhe NV, Stevens PE, Crowe AV, Lipkin GW, Harrison DA (2008) Case mix, outcome and activity for patients with severe acute kidney injury during the first 24 hours after admission to an adult, general critical care unit: application of predictive models from a secondary analysis of the ICNARC Case Mix Programme database. Crit Care 12(Suppl 1):S2
Tian J, Barrantes F, Amoateng-Adjepong Y, Manthous CA (2009) Rapid reversal of acute kidney injury and hospital outcomes: a retrospective cohort study. Am J Kidney Dis 53:974–981
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8:R204–R212
Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, Metnitz PG (2009) Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med 35:1692–1702
Kociol R, Rogers J, Shaw A (2009) Organ cross talk in the critically ill: the heart and kidney. Blood Purif 27:311–320
Ricci Z, Ronco C (2010) Pulmonary/renal interaction. Curr Opin Crit Care 16:13–18
Hoste EA, De Waele JJ (2005) Physiologic consequences of acute renal failure on the critically ill. Crit Care Clin 21:251–260
Ronco C (2010) Cardiorenal syndromes: definition and classification. Contrib Nephrol 164:33–38
Kirwan CJ, Lee T, Holt DW, Grounds RM, MacPhee IA, Philips BJ (2009) Using midazolam to monitor changes in hepatic drug metabolism in critically ill patients. Intensive Care Med 35:1271–1275
Dowling TC, Briglia AE, Fink JC, Hanes DS, Light PD, Stackiewicz L, Karyekar CS, Eddington ND, Weir MR, Henrich WL (2003) Characterization of hepatic cytochrome p4503A activity in patients with end-stage renal disease. Clin Pharmacol Ther 73:427–434
Dreisbach AW, Lertora JJ (2003) The effect of chronic renal failure on hepatic drug metabolism and drug disposition. Semin Dial 16:45–50
Michaud J, Dube P, Naud J, Leblond FA, Desbiens K, Bonnardeaux A, Pichette V (2005) Effects of serum from patients with chronic renal failure on rat hepatic cytochrome P450. Br J Pharmacol 144:1067–1077
Guevin C, Michaud J, Naud J, Leblond FA, Pichette V (2002) Down-regulation of hepatic cytochrome p450 in chronic renal failure: role of uremic mediators. Br J Pharmacol 137:1039–1046
Finta C, Zaphiropoulos PG (2000) The human cytochrome P450 3A locus. Gene evolution by capture of downstream exons. Gene 260:13–23
Paulussen A, Lavrijsen K, Bohets H, Hendrickx J, Verhasselt P, Luyten W, Konings F, Armstrong M (2000) Two linked mutations in transcriptional regulatory elements of the CYP3A5 gene constitute the major genetic determinant of polymorphic activity in humans. Pharmacogenetics 10:415–424
Fisher MB, Paine MF, Strelevitz TJ, Wrighton SA (2001) The role of hepatic and extrahepatic UDP-glucuronosyltransferases in human drug metabolism. Drug Metab Rev 33:273–297
Paine MF, Khalighi M, Fisher JM, Shen DD, Kunze KL, Marsh CL, Perkins JD, Thummel KE (1997) Characterization of interintestinal and intraintestinal variations in human CYP3A-dependent metabolism. J Pharmacol Exp Ther 283:1552–1562
Ball SE, Scatina J, Kao J, Ferron GM, Fruncillo R, Mayer P, Weinryb I, Guida M, Hopkins PJ, Warner N, Hall J (1999) Population distribution and effects on drug metabolism of a genetic variant in the 5’ promoter region of CYP3A4. Clin Pharmacol Ther 66:288–294
Floyd MD, Gervasini G, Masica AL, Mayo G, George AL Jr, Bhat K, Kim RB, Wilkinson GR (2003) Genotype-phenotype associations for common CYP3A4 and CYP3A5 variants in the basal and induced metabolism of midazolam in European- and African-American men and women. Pharmacogenetics 13:595–606
Fredericks S, Moreton M, MacPhee IA, Mohamed M, Marlowe S, Jorga A, Johnston A, Carter ND, Holt DW (2005) Genotyping cytochrome P450 3A5 using the Light Cycler. Ann Clin Biochem 42:376–381
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317:1098
Wandel C, Witte JS, Hall JM, Stein CM, Wood AJ, Wilkinson GR (2000) CYP3A activity in African American and European American men: population differences and functional effect of the CYP3A4*1B5’-promoter region polymorphism. Clin Pharmacol Ther 68:82–91
Hsu CY, Ordonez JD, Chertow GM, Fan D, McCulloch CE, Go AS (2008) The risk of acute renal failure in patients with chronic kidney disease. Kidney Int 74:101–107
Driessen JJ, Vree TB, Guelen PJ (1991) The effects of acute changes in renal function on the pharmacokinetics of midazolam during long-term infusion in ICU patients. Acta Anaesthesiol Belg 42:149–155
Rogers JF, Rocci ML Jr, Haughey DB, Bertino JS Jr (2003) An evaluation of the suitability of intravenous midazolam as an in vivo marker for hepatic cytochrome P4503A activity. Clin Pharmacol Ther 73:153–158
Fragen RJ (1997) Pharmacokinetics and pharmacodynamics of midazolam given via continuous intravenous infusion in intensive care units. Clin Ther 19:405–419 (discussion 367–408)
Wiedermann CJ, Wiedermann W, Joannidis M (2010) Hypoalbuminemia and acute kidney injury: a meta-analysis of observational clinical studies. Intensive Care Med 36:1657–1665
Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, Lopez-Jimenez F (2010) Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes (Lond) 34:791–799
Verbraecken J, Van de Heyning P, De Backer W, Van Gaal L (2006) Body surface area in normal-weight, overweight, and obese adults. A comparison study. Metabolism 55:515–524
MacPhee IA, Fredericks S, Tai T, Syrris P, Carter ND, Johnston A, Goldberg L, Holt DW (2004) The influence of pharmacogenetics on the time to achieve target tacrolimus concentrations after kidney transplantation. Am J Transplant 4:914–919
Thomson SJ, Cowan ML, Johnston I, Musa S, Grounds M, Rahman TM (2009) ‘Liver function tests’ on the intensive care unit: a prospective, observational study. Intensive Care Med 35:1406–1411
Chow PKH, Yu W-K, Soo K-C, Chan STF (2003) The measurement of liver blood flow: a review of experimental and clinical methods. J Surg Res 112:1–11
Swart EL, van der Hoven B, Groeneveld AB, Touw DJ, Danhof M (2002) Correlation between midazolam and lignocaine pharmacokinetics and MEGX formation in healthy volunteers. Br J Clin Pharmacol 53:133–139
Mizushima Y, Tohira H, Mizobata Y, Matsuoka T, Yokota J (2003) Assessment of effective hepatic blood flow in critically ill patients by noninvasive pulse dye-densitometry. Surg Today 33:101–105
Nolin TD, Frye RF, Le P, Sadr H, Naud J, Leblond FA, Pichette V, Himmelfarb J (2009) ESRD impairs nonrenal clearance of fexofenadine but not midazolam. J Am Soc Nephrol 20:2269–2276
Brandi LSMD, Bertolini RMD, Santini LMD, Cavani SMD (1999) Effects of ventilator resetting on indirect calorimetry measurement in the critically ill surgical patient. Crit Care Med 27:531–539
Kurnik D, Wood AJJ, Wilkinson GR (2006) The erythromycin breath test reflects P-glycoprotein function independently of cytochrome P450 3A activity. Clin Pharmacol Ther 80:228–234
Chaobal HN, Kharasch ED (2005) Single-point sampling for assessment of constitutive, induced, and inhibited cytochrome P450 3A activity with alfentanil or midazolam. Clin Pharmacol Ther 78:529–539
Kuypers DR, de Jonge H, Naesens M, Vanrenterghem Y (2008) Effects of CYP3A5 and MDR1 single nucleotide polymorphisms on drug interactions between tacrolimus and fluconazole in renal allograft recipients. Pharmacogenet Genomics 18:861–868
Acknowledgments
The authors would like to thank the St George’s Research Fund for enabling the research to be done and Michelle Moreton of the Analytical Unit for helping us with the genotyping of the CYP 3A enzymes. Dr Christopher Kirwan was involved in the design, the recruitment of patients, collection of data and samples, analysis of data and writing of the manuscript. Dr Iain MacPhee was involved in the design and supervision of the research. Mr Terry Lee developed the midazolam assay and handled the samples. Professor David Holt developed the midazolam assay. Dr Barbara Philips was involved in the development and design of the research, the recruitment of patients, supervision of the study, analysis of the data and writing of the manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kirwan, C.J., MacPhee, I.A.M., Lee, T. et al. Acute kidney injury reduces the hepatic metabolism of midazolam in critically ill patients. Intensive Care Med 38, 76–84 (2012). https://doi.org/10.1007/s00134-011-2360-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2360-8