Abstract
Introduction
Monitoring ventilated infants is difficult during high-frequency oscillatory ventilation (HFOV). This study tested the possible causes of hypoxemic episodes using a new method for monitoring chest wall movement during HFOV in newborn infants.
Methods
Three miniature motion sensors were attached to both sides of the chest and to the epigastrium to measure the local tidal displacement (TDi) at each site. A >20% change in TDi was defined as deviation from baseline.
Results
Eight premature infants (postmenstrual age 30.6 ± 2.6 weeks) were monitored during 10 sessions (32.6 h) that included 21 hypoxemic events. Three types of such events were recognized: decrease in TDi that preceded hypoxemia (n = 11), simultaneous decrease in TDi and SpO2 (n = 6), and decrease in SpO2 without changes in TDi (n = 4). In the first group, decreases in TDi were detected 22.4 ± 18.7 min before hypoxemia, and were due to airway obstruction by secretions or decline in lung compliance. The second group resulted from apnea or severe abdominal contractions. In the third group, hypoxia appeared following a decrease in FiO2.
Conclusions
Monitoring TDi may enable early recognition of deteriorating ventilation during HFOV that eventually leads to hypoxemia. In about half of cases, hypoxemia is not due to slowly deteriorating ventilation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
High-frequency oscillatory ventilation (HFOV) is one of several methods for ventilating newborn infants with respiratory insufficiency [1–3]. This method is frequently used for rescue or as a lung-protective ventilation strategy [4].
Hypoxemic episodes are frequent in ventilated prematurely newborn infants even when ventilated, for which decrease in lung volume and acute worsening in lung mechanics were found to be responsible during conventional ventilation [5]. Monitoring the adequacy of ventilation during HFOV is a clinical challenge compared with during conventional ventilation. Moreover, most of the monitoring devices alert the attending staff to a problem only after a significant change in one of the vital signs has occurred, when the infant already has established respiratory failure [6–10].
We hypothesized that direct and continuous monitoring of chest wall movement using miniature motion sensors would provide additional information about the development of various respiratory problems in mechanically ventilated infants. These data may facilitate correct diagnosis and early implementation of corrective measures. Therefore, we have developed a method of continuous noninvasive monitoring of ventilation dynamics and symmetry of ventilation. We have evaluated this method in a preclinical study in which decreases in peak inspiratory pressure, one-lung intubation, and slowly progressive pneumothorax were investigated in mechanically ventilated anesthetized rabbits. The results showed high sensitivity to changes in the amplitude and symmetry of ventilation and fast detection of developing pneumothorax [11].
The objective of this study is to test the utility of continuous monitoring of chest wall movement for characterization of hypoxemic episodes in premature infants during HFOV.
Methods
This observational study included newborn infants who were born at the Carmel Medical Center between December 2007 and July 2008, and who needed mechanical ventilation in the neonatal intensive care unit (NICU). The study was approved by the Institutional Review Board and the Israeli Ministry of Health, and registered at the US National Institutes of Health (NCT00702169).
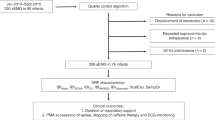
The babies were mechanically ventilated by either an SLE 2000 or SLE 5000 ventilator (SLE Ltd., UK). The following parameters were continuously monitored by a Philips IntelliVue MP40 monitoring system (Philips Ltd., Medizin Systeme, Boeblingen, Germany) with an attached pulse oximeter module (Nellcor Puritan Bennett, LLC, Pleasanton, CA): heart rate (HR), mean arterial blood pressure (MABP), and pulse oximetry (SpO2), recorded in all infants. Transcutaneous O2 and CO2 partial pressure (TCM-Radiometer module for Philips MP40) and blood gas analysis were performed and recorded according to clinical team needs. Printouts of the monitor recordings and the medical follow-up sheets were collected for offline analysis.
Three miniature motion sensors were attached to each baby using commercial adhesive patches; one sensor was attached to each side of the chest, adjacent to electrocardiographic electrodes, and the third sensor was attached on the epigastrium. Each sensor was connected to an isolated preamplifier, and data were acquired at sampling rate of 5 kHz on a laptop computer. Each sensor measures the local acceleration at the attachment site, which is then used to calculate the local displacement of the chest wall due to lung inflation and deflation. The caregivers were blind to the monitored signals.
Each sensor weighs less than 1 g and has a diameter of 5 mm. Each sensor measures the chest wall motion and the subsonic and acoustic vibrations of breath and heart sounds. The sensitivity of each sensor was quantified and calibrated by using a high-resolution (1 μM) computerized lever arm system (Aurora Scientific Inc., Ontario, Canada). A linear relationship (R 2 = 0.99) between the imposed oscillation amplitude and the measured tidal displacement was found, and the variability in sensitivity between the sensors was 3.7%. The flatness of the frequency response of the system was good over the frequency spectrum of HFOV.
The only inclusion criterion for the study was the need for tight respiratory monitoring of the newborn infant. The exclusion criteria were: parental refusal to participate in the study, weight less than 700 g, postmenstrual (i.e., gestational + postnatal) age less than 27 weeks, hydrops fetalis or an acute life-threatening condition, a major congenital anomaly, or skin reactions to the adhesive patches.
Data analysis
Data analysis was performed offline. The subsonic signal of each motion sensor was used to calculate the local tidal displacement (TDi) at each site, i.e., at the right (TDiR) and left (TDiL) sides of the chest and on the epigastrium. The TDi at each site is a measure of the peak-to-peak motion amplitude, in millimeters. The ratio of the right to left chest wall displacement (R/L) characterized the symmetry of ventilation.
Based on our previous experience in animal studies [11] a 20% change from the baseline value in the displacement of one or more of the motion sensors was defined as a deviation. The time elapsed from a detected deviation in the TDi values to detection of a hypoxemic event was used as a measure of the time of detection of inappropriate ventilation by the motion sensors. A hypoxemic event was defined as a sustained drop in SpO2 to below 90%. Our choice of the 90% threshold for the SpO2 value is not a reflection of the standard interventional and management procedures of the NICU. Values are presented as mean ± standard deviation (SD).
Results
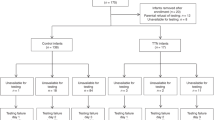
Eight babies with respiratory failure (three males) were monitored during the time that they were ventilated by HFOV at ten different sessions. Mean postmenstrual age was 30.6 ± 2.6 weeks (gestational age at birth 29.2 ± 3.5 weeks), and mean weight was 1,251.6 ± 429.1 g. Six infants suffered from respiratory distress syndrome (RDS) and were recorded between the second and fourth day after birth. Two babies with bronchopulmonary dysplasia (BPD) were ventilated because of sepsis, and the recordings were made 25–33 days after birth. Each monitoring session lasted 196 ± 116 min. In total, 32.6 h of monitoring data, which included 21 hypoxemic events, was acquired (Fig. 1). Four representative events and their monitoring records are shown in Figs. 2–5. The ventilator parameters were: frequencies of 11 ± 1 Hz, mean airway pressure 8 ± 3 cmH2O, and delta P (ΔP) 15 ± 7 cmH2O. The monitored babies did not receive sedation or opiates before or during the monitored periods.
Early detection of deterioration of ventilation due to obstruction by secretions (case 0309). Deterioration in ventilation was detected 47 min before hypoxemia appeared. Suction removed the sticky secretions and resulted in an improvement in the TDi values, which was followed later by an improvement in SpO2. (The TCM traces were interrupted twice due to separation of the sensor from the skin)
Early detection of deterioration of ventilation due to inadequate ventilation (case 0308). Deterioration of ventilation was detected 13 min before the drop in SpO2 and TCpO2. The neonate suffered from hemodynamic instability [fluctuations in heart rate (HR)] and became restless (crying). Bilateral improvement in TDi was followed by an improvement in SpO2 and TCpO2 that occurred after increasing the continuous distending pressure (CDP)
Figure 1 summarizes the distribution of all hypoxemic events and events in which TDi decreased. There were 21 hypoxemic events and 19 events in which TDi decreased. Three main types of hypoxemic events were recognized: (a) events that were preceded by a gradual and persistent decrease in TDi, (b) events in which there was simultaneous decrease in TDi and SpO2, and (c) events of hypoxemia in which there were no significant deviations in TDi.
The first type (a) was the most frequent and accounted for 52.4% (n = 11) of all hypoxemic events. In this group, deteriorating ventilation was detected by the motion sensors 22.4 ± 18.7 min (range 4–46 min) before the appearance of hypoxemia, and before the newborns became symptomatic (restless, startled, and/or developed tachycardia). Six events were resolved by suction, with overt and fast increase in TDi that was followed by slow improvement in SpO2, as shown in Fig. 2. Three events were successfully treated by increasing the continuous distending pressure (CDP), as shown in Fig. 3, resulting in restoration of TDi and SpO2. Two relatively mild (SpO2 > 85%) and short (<3 min) events were not treated or investigated, and both TDi and SpO2 recovered spontaneously.
The second type of hypoxemic events (b) accounted for 28.6% (n = 6) of all the events. In one newborn, there were two desaturation events with sudden disappearance of the spontaneous breathing pattern (apnea), as shown in Fig. 5. In one newborn, who suffered from severe ileus and sepsis, four hypoxemic events concomitantly occurred with severe abdominal contractions that were also detected by the ventilator alarm.
The third type of hypoxemic events (c) accounted for only 19% (n = 4) of all the events. Three of the four events in this group appeared in an infant with BPD after attempts to reduce the FiO2 (below 40%).
There was only one mild, unexplained, event of desaturation (SpO2 > 80%) without changes in TDi. The duration of this event was less than 5 min, and it resolved spontaneously. One neonate had two transient events of decrease in TDi, for less than 3 min, which occurred without any changes in SpO2. Therefore, the predictive value of significant deviation in TDi for early detection of deteriorating ventilation was 84.6%. There were 13 events of progressive decrease in TDi, and in 11 events (a) this deterioration progressed to hypoxemia and required intervention.
The initial 70 min of monitoring of a 35 weeks gestation female infant with RDS and weight 1,964 g are shown in Fig. 2. A decrease in TDi was detected after 4 min, 47 min before the occurrence of a profound hypoxemic event (SpO2 < 70%). Detection of the decrease in the TDi values was associated with moderate instability in the heart rate. The TDi immediately returned to the initial baseline level after successful open endotracheal suction was performed, followed by a slow increase in SpO2 and a reduction in the heart rate. Therefore, the decrease in TDi and the hemodynamic instability were probably due to the prolonged (47 min) reduced ventilation. About 30 min after the decrease in the TDi was detected, closed endotracheal suction was performed. Interestingly, it was unsuccessful, without extraction of secretions, and was not associated with improvement in the TDi values.
Figure 3 depicts 45 min of recordings from a 33 weeks, 1,643 g female infant with RDS. A decrease >20% in the TDi was detected after 42 min of monitoring on the right side and after 46 min on the left side. The changes in the TDi values were associated with hemodynamic instability (HR rose from 150 to 200 bpm). Simultaneous decrease in SpO2 and TCpO2 and mild increase in TCpCO2 occurred 13 min after the overt decrease in the TDi values. Bilateral improvement in the TDi values occurred after the CDP was raised (from 10 to 13 cmH2O) and was followed by a slow increase in SpO2.
Figure 4 presents recording from a 25 weeks gestation, 752 g female infant with BPD, monitored on day 25 after birth. After 107 min, the FiO2 was decreased from 40% to 35%, which caused a slow gradual drop in SpO2. Twelve minutes later, a hypoxemic event presented, lasting for 15 min, and she was initially treated with suction for a suspected airway obstruction. Suction did not yield any secretions, and SpO2 continued to drop (70%). It is important to note that there was no change in TDi before the event. Therefore, the decrease in SpO2 was probably due to FiO2 reduction that preceded this event.
Figure 5 displays the abrupt disappearance of the spontaneous breathing pattern from the sensor on the epigastrium in one infant. This episode was associated with a concomitant hypoxemic event.
The effects of the therapeutic interventions on the monitored TDi values were also studied. Altogether, 29 therapeutic interventions were done. There were 13 instances in which only FiO2 was modified. There were 16 mechanical interventions that comprised 10 interventions of suction, 3 changes in CDP, 2 changes in endotracheal tube positioning, and 1 ventilator replacement.
In 9 of the 16 mechanical interventions (56%) there was an improvement in TDi, which was followed by an improvement in SpO2 (Figs. 2, 3). This group included suction in six cases, and three cases in which CDP was increased. In the four unsuccessful suction interventions (no extracted secretions) that were done when the patient suffered from hypoxemia the motion sensors did not detect any improvement in TDi. Interestingly, this lack of improvement in the TDi values was associated with no improvement in SpO2. Therefore, and considering that the number of studied patients is very small, the positive predictive value for efficacy assessment of mechanical intervention was 100%, since all interventions that were associated with significant improvement in TDi were also associated with concomitant changes in SpO2. The negative predictive value was also 100%.
Discussion
This study explores the feasibility of continuous monitoring of chest wall dynamics while ventilating premature newborn infants with HFOV and the utility of the method for better characterization of hypoxemic events. This observational study suggests that the novel method has three important advantages: (a) it provides sensitive detection of changes in the amplitude and dynamics of ventilation during HFOV that enables early recognition of deteriorating ventilation, (b) it provides additional information that can improve the accuracy of diagnosis of hypoxemic events and thus may facilitate the correct therapeutic intervention, and (c) it assesses the efficacy of therapeutic interventions.
Early detection of gradual and persistent deteriorating ventilation was observed before development of hypoxemia in 52.4% of recordings. The main cause was partial obstruction by secretions, and a less frequent cause was inadequate ventilation, probably due to slow change in lung compliance. In this group, the deterioration was detected by the motion sensors 22.4 ± 18.7 min before its detection by pulse oximetry or by attending staff who recognized that the infant was restless.
The existence of a substantial and critical delay in detection of deteriorating ventilation during mechanical ventilation is well known, especially during HFOV [8, 9, 12–14]. Measuring endotracheal tube pressure and flow is sometimes of limited value due to the uncontrolled air leak around the uncuffed endotracheal tubes that are used in premature newborn infants. This air leak varies from moment to moment, causing errors in tidal volume readings [15]. Measurement of TDi as described herein can provide sensitive detection of changes in the amplitude and dynamics of ventilation during HFOV without errors due to air leaks.
Monitoring chest wall displacement could have facilitated correct diagnosis in 95.2% of cases of deteriorating ventilation (20 of 21 events) by providing additional crucial information, and may enable the attending team to differentiate between three types of hypoxemic events:
(a) A decrease in SpO2 that appears after a gradual and persistent decrease in ventilation due to progressive development of obstruction by secretions or slow decreases in lung compliance.
(b) A paroxysmal decrease in TDi and SpO2 appearing due to two causes: apnea and severe abdominal contractions. These events are characterized by severe immediate impairments in the normal functioning of breathing muscles.
(c) The third type of hypoxemic events occurred when the FiO2 was reduced, and it was not associated with changes in the TDi. Hypoxemia without changes in the mechanical ventilation (TDi) can also occur when diffusion of oxygen across the alveoli decreases or when ventilation–perfusion mismatch develops. In these situations, the absence of change in the TDi provides important information: it may eliminate the possibility of a mechanical problem, and avoid unnecessary intervention such as suction.
Measuring TDi provides additional valuable information, because it provides immediate feedback on the effects of therapeutic interventions on changes in ventilation dynamics. Ten interventions of suction were performed; six were successful and four were unsuccessful (without extraction of secretions). For all ten suctions, there was a tight correlation between the changes in TDi and the subsequent change in SpO2.
Auscultation can be used for monitoring lung ventilation during HFOV [16]. Numerous studies have explored the use of breath sounds to develop a “pulmonary hearing aid” for diagnosing different respiratory diseases [17–20], based on recorded breath sounds in normal condition and various diseases [17–20]. The method described herein does not use a databank. Instead, the method compares the immediate recordings against a previous recording from the same patient. The comparison against a previous recording from the same patient makes the analysis highly sensitive to changes in ventilation in the monitored patient. It should also be noted that TDi monitoring captures the signal from subsonic vibrations of the chest (below 20 Hz).
Several noninvasive modalities have been developed for assessing respiratory mechanics in infants, such as respiratory inductance plethysmography [21, 22], elastomeric plethysmography, optic respiratory plethysmography [23], and electrical impedance tomography (EIT) [24]. The plethysmographic modalities are not easy to use for continuous monitoring in the setting of an NICU and are bulky [21]. EIT has been studied as a means for quantification of end-expiratory lung volume [25] and global inhomogeneity of lung ventilation, in adults [26]. None of these modalities are presently used in the clinical setup of NICU.
Hot-wire anemometers were recently used for measuring the tidal volume during HFOV [27, 28]. These studies did not present an attempt to detect deteriorating ventilation or to provide early detection of significant changes in ventilation, before the initiation of therapeutic interventions.
Potential limitations of the device
The modality presented herein monitors tidal displacement at three different sites but does not directly quantify absolute changes in tidal volume. There is a clear relationship between the two, but this relationship depends on the precise location of the patches, which varies from patient to patient. Assessment of changes in tidal volume requires separate calibration for each patient.
Conclusions
This small, observational study shows the feasibility of continuous monitoring of chest wall dynamics during HFOV in premature infants and its utility for better characterization of hypoxemic events.
The main findings of the study are:
-
This noninvasive method is simple to implement in an NICU.
-
Monitoring deviation in TDi enabled detection of deteriorating ventilation 22.4 ± 18.7 min before deterioration evolved to hypoxemia that required treatment.
-
Monitoring TDi provided crucial data that could facilitate correct diagnosis in 95.2% of hypoxemic events that required treatment.
-
The TDi enabled fast assessment of the efficacy of therapeutic interventions in the studied group.
Further, larger studies are required to confirm these findings, in an attempt to increase the safety of mechanical ventilation.
References
Eichenwald EC, Stark AR (2008) Management and outcomes of very low birth weight. N Engl J Med 358:1700–1711
Ambalavanan N, Carlo WA (2006) Ventilatory strategies in the prevention and management of bronchopulmonary dysplasia. Semin Perinatol 30:192–199
Greenough A, Donn SM (2007) Matching ventilatory support strategies to respiratory pathophysiology. Clin Perinatol 34:35–53
Lampland AL, Mammel MC (2007) The role of high-frequency ventilation in neonates: evidence-based recommendations. Clin Perinatol 34:129–144
Polimeni V, Claure N, D’Ugard C, Bancalari E (2006) Effects of volume-targeted synchronized intermittent mandatory ventilation on spontaneous episodes of hypoxemia in preterm infants. Biol Neonate 89:50–55
Linder N, Haskin O (2003) Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case-control study. Pediatrics 111:e590–e595
Gammon CM, Wiswell TE, Spitzer AR (1998) Volutrauma, PaCO2 levels, and neuro-developmental sequelae following assisted ventilation. Clin Perinatol 25:159–175
McIntosh N (2002) Intensive care monitoring: past, present and future. Clin Med 2:349–355
McIntosh N, Becher JC, Cunningham S, Stenson B, Laing IA, Lyon AJ, Badger P (2000) Clinical diagnosis of pneumothorax is late: use of trend data and decision support might allow preclinical detection. Pediatr Res 48:408–415
Watkinson M, Tiron I (2001) Events before the diagnosis of a pneumothorax in ventilated neonates. Arch Dis Child Fetal Neonatal Ed 85:F201–F203
Waisman D, Levy C, Konyukhov E, Hanani N, Weisbrod H, Landesberg A (2007) Continuous monitoring of chest wall dynamics allows earlier detection of mechanical complications, in small animal model. E-PAS2007:615895.2 (Abstract)
Frey B, Kehrer B, Losa M, Braun H, Berweger L, Micallef J, Ebenberger M (2000) Comprehensive critical incident monitoring in a neonatal-pediatric intensive care unit: experience with the system approach. Intensive Care Med 26:69–74
Szekely SM, Webb RK, Williamson JA, Russell WJ (1993) The Australian incident monitoring study. Problems related to the endotracheal tube: an analysis of 2,000 incident reports. Anaesth Intensive Care 21:611–616
Sweeney AM, Lyle J, Ferguson ND (2005) Nursing and infection-control issues during high-frequency oscillatory ventilation. Crit Care Med 33:S204–S208
Keszler M (2009) State of the art in conventional mechanical ventilation. J Perinatology 29:262–275
Waisman D, Weintraub Z, Rotschild A, Davkin O, Kessel I, Bental Y (2001) High-Frequency oscillatory ventilation: “Please do not forget me”, said the stethoscope. Pediatrics (letter) 108:819
Kiyokawa H, Pasterkamp H (2002) Volume-dependent variations of regional lung sound, amplitude, and phase. J Appl Physiol 93:1030–1038
Gross V, Dittmar A, Penzel T, Schüttler F, von Wichert P (2000) The relationship between normal lung sounds, age, and gender. Am J Respir Crit Care Med 162:905–909
Kraman SS, Wodicka GR, Pressler GA, Pasterkamp H (2006) Comparison of lung sound transducers using a bioacoustic transducer testing system. J Appl Physiol 101:469–476
Kraman SS, Pressler GA, Pasterkamp H, Wodicka GR (2006) Design, construction, and evaluation of a bioacoustic transducer testing (BATT) system for respiratory sounds. IEEE Trans Biomed Eng 53:1711–1715
Gappa M, Pillow JJ, Allen J, Mayer O, Stocks J (2006) Lung function tests in neonates and infants with chronic lung disease: lung and chest-wall mechanics. Pediatr Pulmonol 41:291–317
Copnell B, Tingay DG, Kiraly NJ, Sourial M, Gordon MJ, Mills JF, Morley CJ, Dargaville PA (2007) Effects of open endotracheal suction on lung volume in infants receiving HFOV. Intensive Care Med 33:689–693
Davis C, Mazzolini A, Mills J, Dargaville P (1999) A new sensor for monitoring chest wall motion during high-frequency oscillatory ventilation. Med Eng Phys 21:619–623
Dunlop S, Hough J, Riedel T, Fraser JF, Dunster K, Schibler A (2006) Electrical impedance tomography in extremely prematurely born infants and during high frequency oscillatory ventilation analyzed in the frequency domain. Physiol Meas 27:1151–1165
Bikker IG, Scohy TV, Bogers AdJ JC, Bakker J, Gommers D (2009) Measurement of end-expiratory lung volume in intubated children without interruption of mechanical ventilation. Intensive Care Med 35:1749–1753
Zhao Z, Möller K, Steinmann D, Frerichs I, Guttmann J (2009) Evaluation of an electrical impedance tomography-based Global Inhomogeneity Index for pulmonary ventilation distribution. Intensive Care Med 35:1900–1906
Sturtz WJ, Touch SM, Locke RG, Greenspan JS, Shaffer TH (2008) Assessment of neonatal ventilation during high-frequency oscillatory ventilation. Pediatr Crit Care Med 9:101–104
Zimová-Herknerová M, Plavka R (2006) Expired tidal volumes measured by hot-wire anemometer during high-frequency oscillation in preterm infants. Pediatr Pulmonol 41:428–433
Acknowledgments
This work was supported in part by the Dr. Y. Rabinovitz Research Fund and the Ruth and Allen Ziegler Fund for Pediatric Research (D.W.), and by a grant for the promotion of research at the Technion (A.L.). The authors thank Pneumedicare for the use of the monitoring equipment and the Department of Neonatology, Carmel Medical Center, for the use of departmental facilities during the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waisman, D., Levy, C., Faingersh, A. et al. A new method for continuous monitoring of chest wall movement to characterize hypoxemic episodes during HFOV. Intensive Care Med 37, 1174–1181 (2011). https://doi.org/10.1007/s00134-011-2228-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2228-y