Abstract
Purpose
In acute respiratory distress syndrome (ARDS), combined high frequency oscillation (HFO) and tracheal gas insufflation (TGI) improves oxygenation versus standard HFO, likely through TGI-induced lung recruitment. Experimental data suggest that steady flows such as TGI favor the filling of the lower (i.e., subcarinal) lung. We used whole-lung computerized tomography (CT) to determine whether HFO-TGI versus HFO improves the recruitment of the lower lung, and especially of its dependent region, where loss of aeration is maximized in ARDS.
Methods
We enrolled 15 patients who had ARDS for 96 h or less, and pulmonary infiltrates in at least three chest X-ray quadrants. Patients were subjected to whole-lung CT after lung-protective conventional mechanical ventilation (CMV) and after 45 min of HFO and 45 min of HFO-TGI. HFO/HFO-TGI were employed in random order. CT scans were obtained at a continuous positive airways pressure equal to the mean tracheal pressure (P tr) of CMV. During HFO/HFO-TGI, mean airway pressure was titrated to the CMV P tr level. Gas exchange and intra-arterial pressure/heart rate were determined for each ventilatory technique.
Results
Regarding total lung parenchyma, HFO-TGI versus HFO and CMV resulted in a lower percentage of nonaerated lung tissue (mean ± SD, 51.4 ± 5.1% vs. 60.0 ± 2.5%, and 62.1 ± 9.0%, respectively; P ≤ 0.04); this was due to HFO-TGI-induced recruitment of nonaerated tissue in the dependent and nondependent lower lung. HFO-TGI increased normally aerated tissue versus CMV (P = 0.04) and poorly aerated tissue versus HFO and CMV (P ≤ 0.04), and improved oxygenation versus HFO and CMV (P ≤ 0.04).
Conclusions
HFO-TGI improves oxygenation versus HFO and CMV through the recruitment of previously nonaerated lower lung units.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In acute respiratory distress syndrome (ARDS), combined high frequency oscillation (HFO) and tracheal gas insufflation (TGI) improves gas exchange relative to HFO without TGI at the same mean airway pressure (P aw) [1, 2] and mean tracheal pressure (P tr) [3]. Continuous, forward-thrust TGI exerts a positive end-expiratory pressure (PEEP) effect by impeding the opposite-directed expiratory flow [1–4]. Recent data, including esophageal pressure measurements [3], suggest a TGI-related increase in lung volume, which largely explains the improvements in oxygenation and PaCO2 when TGI is added to HFO. This implies a TGI-induced lung recruitment, partly achieved through its PEEP effect [3].
Steady flows, such as TGI, probably favor the filling of the lower lung, because the branching angles of the lower and right middle lobar and segmental bronchi are less acute compared to the branching angles of the upper lobar and segmental bronchi [5]. Consequently, the addition of TGI to HFO should mainly enhance the aeration of the lung parenchyma located below the carina [3, 5]. This potential effect should be more prominent in dependent, lower lung regions, in which the ARDS-related loss of aeration is maximized [6–9].
Preceding studies [1, 3] could not elucidate the effect of HFO-TGI on regional lung aeration. Besides recruitment, TGI could enhance the asymmetry between inspiratory and expiratory impedances observed during HFO [3, 10], and concurrently contribute to hyperinflation [1, 10]. Whole-lung computed tomography (CT) is the gold standard method of assessment of regional lung aeration [8, 9, 11–13]. In this study, we used CT to compare the regional effects of HFO and HFO-TGI at a pre-specified P tr level. We theorized that HFO-TGI would mainly reduce the amount of nonaerated lung tissue, especially in the dependent, lower lung, and thus improve both overall and lower lung aeration.
Methods
Patients
Institutional approval and informed, written next-of-kin consent were obtained. Patients had ARDS [14] for 96 h or less. PaO2/inspired O2 fraction (FiO2) was within 80–199 mmHg with a PEEP of at least 8 cmH2O for longer than 12 h. Pulmonary infiltrates were present in at least three frontal chest X-ray quadrants (Murray chest roentgenogram score at least 3 [15]). Full eligibility criteria are provided in Table E1 of the “Electronic supplementary material” (ESM).
On study-enrollment, patients were anesthetized, intubated (8.5- to 9.0-mm orotracheal or 8.0- to 9.0-mm tracheostomy tube [3]), and mechanically ventilated (Maquet Servo 300C or Servo-i ventilator) in a semirecumbent position (ESM). Electrocardiographic lead II, intra-arterial pressure, and peripheral oxygen saturation (SpO2) were monitored continuously. Patients were on lung-protective, low-volume, plateau pressure-limited, conventional mechanical ventilation (CMV) employing pre-specified PEEP/FiO2 combinations [16; ESM]. Gas exchange targets were PaO2 = 60–80 mmHg, SpO2 = 90–95%, and arterial pH = 7.20–7.45.
Study design
Pre-transportation period
Details are provided in the ESM. Within 60–40 min before transportation to the CT suite, cisatracurium (0.15 mg/kg) was administered, a 2-catheter (i.e., a TGI catheter and a pressure-measuring catheter)-circuit adapter system was introduced [3], and a recruitment maneuver [continuous positive airway pressure (CPAP) of 40 cmH2O for 30 s at FiO2 1.0] was performed. CMV was resumed, patients were placed supine, and P tr was determined and termed the study P tr level. The P tr level was within less than 1 cmH2O of the concurrent, conventional ventilator-displayed P aw [3], which was also recorded and termed the study CMV P aw. Subsequently, arterial blood gases, respiratory compliance [17], and Murray score [14] were determined.
At 40 min pre-transportation, patients were connected to the Sensormedics 3100B high frequency ventilator. Ventilator settings were FiO2 = 1.0, bias flow = 60 L/min, frequency = 4.0 Hz, oscillatory pressure amplitude (ΔP) = 90 cmH2O, and inspiratory-to-expiratory time ratio 1:2. Following HFO initiation, a reproducible [1, 3] cuff leak of 4–5 cmH2O (corresponding to cuff deflation by 2.0–3.0 mL) was established, and the high frequency ventilator P aw was titrated to the study P tr level and its value recorded and termed the study HFO P aw. Subsequently, continuous, forward-thrust TGI (FiO2 = 1.0; flow = 50% of immediately preceding CMV minute ventilation) was added to HFO, and the high frequency ventilator P aw was re-titrated to the study P tr level and its value recorded and termed the study HFO-TGI P aw.
At 20 min pre-transportation, the catheters were withdrawn and CMV was resumed. Following arrival at the CT suite, patients were placed supine on the CT scanner bed and reconnected to the intensive care unit (ICU) ventilator. CMV was continued at FiO2 = 1.0 and all other original ICU settings were maintained unchanged. Subsequently, cisatracurium was re-administered.
Main study period
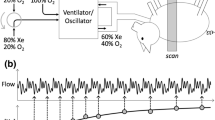
Figure 1 illustrates the main investigational interventions. A recruitment maneuver (CPAP = 40 cmH2O for 30 s) was performed and the TGI catheter and pressure-measuring catheter were reintroduced through their respective adapters. The TGI catheter was proximally connected to a variable orifice O2 flowmeter, with O2 flow set at 0 L/min, whereas the proximal orifice of the pressure-measuring catheter was capped. We inserted both catheters to reproduce the pre-transportation, supine ventilatory conditions. This consistently resulted in a ventilator-displayed P aw that was within less than 0.5 cmH2O of the predetermined study CMV P aw. Following 15 min of equilibration, a set of physiological measurements (i.e., arterial/central-venous blood gas analyses, intra-arterial pressure and heart rate, and respiratory mechanics [17]) was obtained. Immediately after the end-inspiratory occlusion, the ICU ventilator was set at CPAP = predetermined study P tr level and a whole-lung CT was performed (Fig. 1). Subsequently, patients were connected to the high frequency ventilator, the recruitment maneuver was repeated, and HFO or HFO-TGI (each for 45 min in random order) was initiated with the aforementioned pre-transportation, high frequency ventilator and/or TGI settings (including the predetermined study HFO P aw or study HFO-TGI P aw), and the same cuff leak. After every 45 min of HFO or HFO-TGI, blood gases and hemodynamics were redetermined and the whole-lung CT scan was repeated at high frequency ventilator-applied CPAP = study P tr level (Fig. 1). Subsequently, patients were transported back to the ICU (ESM).
Schematic representation of study methodology. CT computed tomography, RM recruitment maneuver, CMV conventional mechanical ventilation, HFO high frequency oscillation, TGI tracheal gas insufflation, P aw mean airway pressure, P tr mean tracheal pressure, CPAP continuous positive airways pressure, Roi region of interest. Left panel schematic representation of the investigational interventions of the study protocol; *see text for details; † P aw settings were aimed at achieving the study P tr level (see also “Methods”); §HFO preceded HFO-TGI in eight patients, and the reverse order was followed in another seven patients; we did not perform any RM in-between HFO and HFO-TGI. Right upper panel in each CT section, the subdivision of lung parenchyma in anterior (nondependent) and posterior (dependent) regions was performed by drawing a line (XX′) passing through the midpoint of and being vertical to the anteroposterior axis of the thoracic cavity (MM′). Right lower panel for each CT section, the aforementioned subdivision resulted in two nondependent Rois (i.e., Roi-1 and Roi-3) and two dependent Rois (i.e., Roi-2 and Roi-4)
CT imaging and analysis
Helical CT scanning was performed on a Toshiba Aquilion 16-row detector CT scanner (detector configuration, 16 × 2.0 mm; z-direction length, 32 mm), software version V1.41ER001 (Toshiba, London, UK). CT scanner settings were contiguous slice thickness = 7 mm (voxel volume, ~4.2 mm3); speed, 30 mm/rotation; beam pitch, 0.9375 [18, 19]; exposure time = 0.50 s; voltage = 135 kV; and current = 200 mA. CT data analysis is detailed in the ESM. Briefly, in each CT section, the outline of the lungs was manually drawn (Fig. 1) by two investigators blinded to the employed ventilatory technique. Lung regions were classified as hyperinflated [CT number = −901 to 1,000 Hounsfield units (HU)], normally aerated (CT number = −501 to 900 HU), poorly aerated (CT number = −101 to 500 HU), and nonaerated (CT number = +100 to 100 HU). Whole-lung results were expressed according to the varying degrees of aeration and corresponding percentage of lung tissue weight [13].
CT analysis was repeated after lung parenchymal subdivision in nondependent and dependent upper, and nondependent and dependent lower regions. Anterior (nondependent) and posterior (dependent) subdivision of CT sections is illustrated in Fig. 1. Lower lung ranged from the first subcarinal CT section to the last basal section. Upper lung extended from the CT section corresponding to the carina to the first apical section.
Statistical analysis
According to an apriori power analysis, 15 patients were required for a = 0.04, and power = 0.88 (see ESM). Data were analyzed with SPSS version 12.0 (SPSS, Chicago, IL, USA). The distribution normality was tested by the Kolmogorov–Smirnov test. For each ventilatory technique level, physiological and CT image analysis data were compared with repeated-measures analysis of variance for one within-subjects factor (i.e., ventilatory technique), followed by the Tukey test. Bivariate, least-squares, linear regression was used to interpret changes in physiological variables. Significance was accepted at P < 0.05. Data are reported as mean ± SD.
Results
We enrolled 15 nonconsecutive patients with ARDS over a 3.5-year period (i.e., within 2006–2009). Table 1 displays the patients’ baseline characteristics. There were no study protocol-related complications or instances of patient spontaneous breathing or coughing. SpO2 was always at least 90% throughout study period.
Relative to baseline, the first set of study physiological measurements (Fig. 1) showed that transportation did not notably affect gas exchange (Tables 1, 2; ESM), inspiratory/expiratory CMV pressures, CMV P aw (see also above and ESM), and respiratory resistance or compliance (ESM). Tracheal tube dimensions, insertion depth, and patency remained unchanged throughout the study (ESM). Thus, the pre-transportation, supine, CMV P tr level (i.e., the study P tr level) should have been re-achieved during pre-HFO/HFO-TGI CMV in the CT suite [3] (ESM). Also, in the presence of identical HFO/HFO-TGI settings (including bias flow and ΔP) and cuff leak, and unchanged tracheal tube characteristics, the use of study HFO/HFO-TGI P aw in the CT suite should have reproduced the study P tr level [3] (ESM).
The study HFO P aw and HFO-TGI P aw were 28.7 ± 1.5 and 27.4 ± 1.4 cmH2O, respectively, and employed TGI flow was 6.1 ± 0.5 L/min (range 4.5–6.5); in the presence of a 4–5 cmH2O cuff leak, the between-P aw difference of 1.3 ± 0.3 cmH2O reflected the TGI-induced increment in P tr [3].
Whole-lung CT scans were performed at CPAP = 21.6 ± 1.7 cmH2O (range 19.0–25.6) (study P tr level; see also above and Table 1).
Physiological variables
Table 2 displays the gas exchange and hemodynamics results. HFO-TGI resulted in a higher PaO2/FiO2 and lower shunt fraction versus CMV and HFO (P ≤ 0.04). The arterial and central-venous PCO2 and pH were improved during HFO-TGI versus CMV (P ≤ 0.03). The oxygenation index was lower during HFO-TGI versus HFO (P = 0.001). The mean arterial pressure, heart rate, and central-venous O2 saturation were unaffected by the ventilatory technique.
CT image analysis
The results are presented in Table 3. Regarding total lung parenchyma, HFO-TGI versus CMV resulted in higher lung volume (P = 0.005) and gas volume (P = 0.002). HFO-TGI versus HFO resulted in trends toward higher lung and gas volume (P = 0.09–0.10). The percentage of normally aerated lung parenchyma was higher during HFO-TGI versus CMV (P = 0.04). The percentage of poorly aerated parenchyma was higher during HFO-TGI versus CMV and HFO (P ≤ 0.04), whereas percentage of nonaerated parenchyma was lower during HFO-TGI versus CMV and HFO (P ≤ 0.001). Notably, in the dependent, lower lung, we observed the same HFO-TGI-related improvements in the percentages of normally aerated (increased vs. CMV, P = 0.005), poorly aerated (increased vs. CMV and HFO, P ≤ 0.002), and nonaerated (decreased vs. CMV and HFO, P < 0.001) parenchyma. Accordingly, the corresponding, regional gas volume was higher during HFO-TGI versus CMV and HFO (P < 0.001). Furthermore, in the nondependent, lower lung, there was an HFO-TGI-related decrease in the percentage of nonaerated parenchyma versus CMV and HFO (P < 0.001). The corresponding regional lung volume and tissue weight were higher during HFO-TGI vs. CMV and HFO (P ≤ 0.009); HFO-TGI resulted in a higher gas volume versus CMV (P = 0.003), and a trend toward higher gas volume versus HFO (P = 0.08). Figure 2 displays average density histograms for the whole lung and dependent, lower lung. Figure 3 displays lower lung CT sections from representative patients.
Computed tomography (CT) sections of the lower lung from four representative patients (1–4). CMV conventional mechanical ventilation, HFO high frequency oscillation, TGI tracheal gas insufflation CT sections correspond to ~7 cm below the carina. In patients 1 and 3 HFO preceded HFO-TGI. In patients 2 and 4 HFO-TGI preceded HFO. Percentages reflect proportions of nonaerated lung tissue weight
In the dependent and nondependent upper lung, ventilatory technique had no significant effect on the distribution of parenchymal aeration. However, both HFO and HFO-TGI were associated with increases in regional lung volume (average increase = 39.5–44.9%) and tissue weight (average increase = 31.2–41.8%) relative to CMV (P ≤ 0.01). The average gas-to-tissue ratios of the HFO/HFO-TGI-induced lung volume increments ranged within 0.9–1.5 and 1.5–2.2 in the dependent and nondependent upper lung, respectively. There was no appreciable, HFO/HFO-TGI-related change in the percentage of hyperinflated lung tissue (Table 3).
Regression analysis
Changes in PaO2/FiO2 from CMV to HFO-TGI and from HFO to HFO-TGI were strongly correlated with concurrent changes in nonaerated, dependent, lower lung parenchyma (R 2 = 0.61–0.74, P ≤ 0.001; Fig. E5 of ESM). PaO2/FiO2 changes were also significantly correlated with concurrent changes in nonaerated, total lung parenchyma (R 2 = 0.42–0.43, P ≤ 0.008). Weaker correlations were observed between changes in shunt fraction and nonaerated, dependent, lower lung parenchyma (R 2 = 0.30–0.33, P ≤ 0.03).
Discussion
HFO-TGI versus HFO and CMV resulted in a reduced amount of nonaerated lung tissue below the carina. During HFO-TGI, poorly aerated tissue increased versus HFO and CMV, and normally aerated tissue increased versus CMV. There were concurrent, HFO-TGI-related improvements in oxygenation and shunt fraction versus HFO and CMV, and PaCO2 versus CMV. These results indicate improved lung recruitment and function with HFO-TGI.
In supine ARDS patients, loss of aeration predominates in dependent, lower lung regions, because it increases along both the anteroposterior and cephalocaudal axes [6–9]. Proposed mechanisms include reductions in regional transpulmonary pressure due to external compression by the heart [7, 8], pleural fluid collections [8], and abdominal contents [6, 8], and increased superimposed pressure exerted by the overlying, edematous lung tissue [9, 20, 21]. In these regions, “inflammatory” atelectasis (i.e., loss of gas volume with excess tissue volume/weight) and/or “compression” atelectasis (i.e., loss of gas volume without excess tissue volume/weight) predominate, and threshold opening pressures may range from ~15 to more than 30 cmH2O [6, 21, 22].
Ιn this study, most patients had moderate to severe hypoxemia during CMV, primary ARDS, and Murray roentgenogram scores were at least 3 (Table 1). Accordingly, CT scanning revealed either diffuse or patchy attenuations [23]. These characteristics are consistent with increased recruitment potential, irrespective of ARDS etiology [13, 22]. Preceding experimental and clinical studies indicate that HFO exhibits time-dependent recruiting effects [24, 25]. This is partly attributable to minimal, distal, parenchymal, distending pressure swings during the respiratory cycle [24, 26], which should attenuate or prevent expiratory derecruitment [24]. Clinical HFO effects on oxygenation depend on the P aw/P tr level, and become evident after 1 h or longer (when HFO is combined with recruitment maneuvers [1, 3, 27, 28]) or 8 h or longer (when HFO is used alone [11, 23]).
Recently [3], 60-min sessions of HFO with P aw titrated to the preceding CMV P tr level did not improve oxygenation versus CMV. In contrast, 60-min sessions of HFO-TGI with P aw titrated to the same P tr level resulted in higher PaO2/FiO2 vs. both CMV and HFO. These results were largely attributed to a TGI-related PEEP effect and associated lung recruitment. Accordingly, in the present study, HFO did not significantly affect whole-lung aeration or gas exchange. In contrast, and in concordance with our hypothesis, HFO-TGI increased total lung and gas volume, largely by promoting penetration of gas into nonaerated, lower lung tissue, thus changing it into poorly aerated tissue participating in gas exchange (Table 3). This partly explains the observed reduction in pulmonary shunt (Table 2) at the employed FiO2 of 1.0 [12].
Hypoxic pulmonary vasoconstriction is frequently impaired in ARDS [8]. Thus, the partial re-aeration of potentially well-perfused (due to gravitational effects) but previously nonaerated, dependent, lower lung regions should be a major cause of HFO-TGI-related oxygenation improvement. Accordingly, regression results showed that the reduction in nonaerated, dependent, lower lung tissue accounted for 61–74% of the TGI-induced oxygenation improvement (Table 2; Fig. E5 of ESM).
HFO and HFO-TGI had similar effects on upper lung aeration. This further confirms our hypothesis that TGI should primarily affect the lower lung. In the upper lung, the HFO/HFO-TGI-induced, concurrent increase in volume and tissue weight can be explained by a potential, early reopening of partially/totally collapsed small airways/alveoli. In cephalic lung regions, external compressive forces are absent and opening pressures of collapsed tissue are relatively low [6, 8, 9]. Also, our results did not reveal any concurrent, regional overdistention (Table 3). Thus, an earlier upper lung recruitment may have reduced regional pulmonary vascular resistance, with consequent blood flow diversion from still non-recruited lower lung units toward recruited upper lung units [12]. This in turn could have increased regional, extravascular lung water, because of the impaired microvascular permeability [29]. In the lower lung, the same mechanism (i.e., earlier recruitment of nondependent/non-compressed vs. dependent/externally compressed lung units [6, 8, 9], causing blood flow diversion toward faster-recruited units) can explain the observed HFO-TGI-related increase in nondependent tissue weight (Table 3). This potential, dependent-to-nondependent blood flow shift is consistent with the HFO-TGI-related reduction in shunt fraction.
Methodological considerations
The lack of P tr determination in the CT suite constitutes a limitation. However, such measurements would have necessitated the co-transport and recalibration of the pressure-measuring equipment (ESM), with a consequent increase in protocol duration/workload and associated safety issues. Furthermore, the unchanged CMV pressures, and ventilatory settings/conditions in the CT suite indicate that the study P tr level was maintained throughout main study period (see “Results” and ESM).
We obtained the CT scans at CPAP level = study P tr level in an effort to approximate the “average” ventilatory conditions during the use of different ventilatory techniques. This may have caused a minor underestimation of lung volume during HFO/HFO-TGI [24]. The periods of HFO/HFO-TGI use were short, and some time-dependent recruiting effects were likely missed. Another limitation was the lack of evaluation of regional lung perfusion [9].
HFO was used first in eight patients (Fig. 1), and relative to CMV, the HFO-recruited lung volume was 0.04 ± 0.10 L before HFO-TGI initiation (ESM). In the remaining seven patients, HFO-TGI was used first, and HFO-TGI-recruited volume was 0.33 ± 0.19 L before HFO initiation (ESM). The higher recruited volume of the “HFO-TGI-first subgroup” may have favorably affected our results on HFO.
Increasing the CT slice thickness and voxel volume may affect the accuracy of hyperinflation assessment [30, 31]. A voxel with CT attenuation greater than −900 HU may contain hyperinflated alveoli in a proportion insufficient to reduce its radiological density to less than −900 HU [22]. Our patients had diffuse aeration loss (Table 3), and the selection of 7-mm slice thickness instead of the 5-mm standard [13] had probably minor to negligible effects on our pulmonary subvolume measurements [30, 31].
Several prior studies have used at least two whole-lung CTs to evaluate the effect of PEEP on lung aeration [6, 12, 13, 22, 23, 30, 32, 33]. Also, several experts support the routine use of CT in ARDS management [8, 9, 34]. We used three whole-lung CTs to determine the effects of HFO and HFO-TGI on lung aeration. Following inspection of CT films, attending physicians of 12 study participants requested long-term HFO-TGI [35] for their patients.
Clinical implications
Our results indicate that when added to HFO, TGI improves oxygenation through a PEEP effect confined to the lower lung. We did not detect any concurrent, TGI-related, regional hyperinflation. We could not determine the degree of TGI flow penetration into lower-lung airways [3]. However, the high TGI jet stream velocity implies a short deadspace transit time and contribution to direct alveolar ventilation [3, 36]. Furthermore, as continuous, forward-thrust TGI opposes expiratory flow [1–4], its regional PEEP effect should comprise a regional increase in expiratory resistance and alveolar pressure. Such a selective, lower-lung recruiting effect may not be achievable through an increase in P aw of HFO without TGI.
PaCO2 results are consistent with a TGI-associated, improved deadspace clearance and augmentation of HFO tidal volume and alveolar ventilation [3]. HFO-TGI caused absolute reductions of ~9–11% in regional/overall nonaerated lung tissue and moderate gas exchange improvements. These effects may prove useful in patients with severe oxygenation disturbances (e.g., PaO2/FiO2 less than 100 mmHg) and/or poor tolerance to hypercapnia [3, 35].
The limitations of long-term TGI include the absence of commercially available equipment, and possible tracheal mucosal damage, retention/inspissation of secretions, hemodynamic compromise, pneumothorax, and gas embolism [1, 3, 4]. For long-term HFO-TGI, we establish a cuff leak, and employ a single catheter-adapter system for humidified TGI gas administration [3, 35].
Conclusions
HFO-TGI improves oxygenation versus HFO and CMV through the recruitment of previously nonaerated lower lung units.
References
Mentzelopoulos SD, Roussos C, Koutsoukou A, Sourlas S, Malachias S, Lachana A, Zakynthinos SG (2007) Acute effects of combined high-frequency oscillation and tracheal gas insufflation in severe acute respiratory distress syndrome. Crit Care Med 35:1500–1508
Dolan S, Derdak S, Solomon D, Farmer C, Johanningman J, Gelineau J, Smith RB (1996) Tracheal gas insufflation combined with high-frequency oscillatory ventilation. Crit Care Med 24:456–465
Mentzelopoulos SD, Malachias S, Kokkoris S, Roussos C, Zakynthinos SG (2010) Comparison of high-frequency oscillation and tracheal gas insufflation versus standard high-frequency oscillation at two levels of tracheal pressure. Intensive Care Med 36:810–816
Nahum A (1998) Equipment review: tracheal gas insufflation. Crit Care 2:43–47
Slutsky AS, Berdine GG, Drazen JM (1980) Steady flow in a model of human central airways. J Appl Physiol 49:417–423
Puybasset L, Cluzel P, Chao N, Slutsky AS, Coriat P, Rouby JJ, CT Scan ARDS Study Group (1998) A computed tomography scan assessment of regional lung volume in acute lung injury. Am J Respir Crit Care Med 158:1644–1655
Malbuisson LM, Busch CJ, Puybasset L, Lu Q, Cluzel P, Rouby JJ, CT Scan ARDS Study Group (2000) Role of the heart in the loss of aeration characterizing lower lobes in acute respiratory distress syndrome. Am J Respir Crit Care Med 161:2005–2012
Rouby JJ, Puybasset L, Nieszkowska A, Lu Q (2003) Acute respiratory distress syndrome: lessons from computed tomography of the whole lung. Crit Care Med 31(Suppl):S285–S295
Gattinoni L, Caironi P, Pelosi P, Goodman LR (2001) What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med 164:1701–1711
Solway J, Rossing TH, Saari AF, Drazen JM (1986) Expiratory flow and dynamic pulmonary hyperinflation during high-frequency ventilation. J Appl Physiol 60:2071–2078
Luecke T, Herrmann P, Kraincuk P, Pelosi P (2005) Computed tomography scan assessment of lung volume and recruitment during high-frequency oscillation. Crit Care Med 33(Suppl):S155–S162
Malbuisson LM, Muller JC, Constantin JM, Lu Q, Puybasset L, Rouby JJ, CT Scan ARDS Study Group (2001) Computed tomography assessment of positive end-expiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1444–1450
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G (2006) Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 354:1775–1786
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R, The Consensus Committee (1994) The American–European consensus conference on ARDS. Definition, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138:720–723
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Mentzelopoulos SD, Roussos C, Zakynthinos SG (2005) Prone position reduces lung stress and strain in severe ARDS. Eur Respir J 25:534–544
Goldman LW (2007) Principles of CT and CT technology. J Nucl Med Technol 35:115–128
Goldman LW (2008) Principles of CT: multislice CT. J Nucl Med Technol 36:57–68
Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Lossapio S, Gattinoni L, Marini JJ (2001) Recruitment and derecruitment during acute respiratory failure. An experimental study. Am J Respir Crit Care Med 164:122–130
Crotti S, Mascheroni D, Caironi P, Pelosi P, Ronzoni G, Mondino M, Marini JJ, Gattinoni L (2001) Recruitment and derecruitment during acute respiratory failure. A clinical study. Am J Respir Crit Care Med 164:131–140
Puybasset L, Gusman P, Muller JC, Cluzel P, Coriat P, Rouby JJ, CT Scan ARDS Study Group (2000) Regional distribution of gas and tissue in acute respiratory distress syndrome. III. Consequences for the effects of positive end-expiratory pressure. Intensive Care Med 26:1215–1227
Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby JJ, CT Scan ARDS Study Group (2000) Regional distribution of gas and tissue in acute respiratory distress syndrome. I. Consequences for lung morphology. Intensive Care Med 26:857–869
Luecke T, Meinhardt JP, Herrmann P, Weisser G, Pelosi P, Quintel M (2003) Setting mean airway pressure during high-frequency oscillatory ventilation according to the static pressure–volume curve in surfactant-deficient lung injury. A computed tomography study. Anesthesiology 99:1313–1322
Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, Carlin B, Lowson S, Granton J, Multicenter oscillatory ventilation for acute respiratory distress syndrome trial (MOAT) study investigators (2002) High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med 166:801–808
Frantz ID 3rd, Close RH (1985) Alveolar pressure swings during high frequency ventilation in rabbits. Pediatr Res 19:162–166
Ferguson ND, Chiche JD, Kacmarek RM, Hallett DC, Mehta S, Findlay GP, Granton JT, Slutsky AS, Stewart TE (2005) Combining high-frequency oscillatory ventilation and recruitment in adults with early acute respiratory distress syndrome: the treatment with oscillation and an open lung strategy (TOOLS) trial pilot study. Crit Care Med 33:479–486
Funk DJ, Lujan E, Moretti EW, Davies J, Young CC, Patel MB, Vaslef SN (2008) A brief report: the use of high-frequency oscillatory ventilation for severe pulmonary contusion. J Trauma 65:390–395
Gattinoni L, Carlesso E, Cadringher P, Valenza F, Vagginelli F, Chiumello D (2003) Physical and biological triggers of ventilator-induced lung injury and its prevention. Eur Respir J 22(Suppl 47):15s–25s
Vieira SR, Nieszkowska A, Lu Q, Elman M, Sartorius A, Rouby JJ (2005) Low spatial resolution computed tomography underestimates lung overinflation resulting from positive pressure ventilation. Crit Care Med 33:741–749
Reske AW, Busse H, Amato MB, Jaekel M, Kahn T, Schwarzkopf P, Schreiter D, Gottschaldt U, Seiwerts M (2008) Image reconstruction affects computer tomographic assessment of lung hyperinflation. Intensive Care Med 34:2044–2053
Vieira SR, Puybasset L, Lu Q, Richecoeur J, Cluzel P, Coriat P, Rouby JJ (1999) A scanographic assessment of pulmonary morphology in acute lung injury. Significance of the lower inflection point detected on the lung pressure–volume curve. Am J Respir Crit Care Med 159:1612–1623
Borges JB, Okamoto VN, Matos GF, Caramez MP, Arantes PR, Barros F, Souza CE, Victorino JA, Kacmarek RM, Barbas CS, Carvalho CR, Amato MB (2006) Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Am J Respir Crit Care Med 174:268–278
Reske AW, Reske AP, Gast HA, Seiwerts M, Beda A, Gottschaldt U, Josten C, Schreiter D, Heller N, Wrigge H, Amato MB (2010) Extrapolation from ten sections can make CT-based quantification of lung aeration more practicable. Intensive Care Med 36:1836–1844
Malachias S, Kokkoris S, Zakynthinos S, Mentzelopoulos SD (2009) High frequency oscillation and tracheal gas insufflation for severe acute respiratory distress syndrome: results from a single-center, phase II, randomized controlled trial [NCT00416260] [abstract]. Intensive Care Med 35(Suppl 1):S6
Pillow JJ (2005) High-frequency oscillatory ventilation: mechanisms of gas exchange and lung mechanics. Crit Care Med 33(Suppl):S135–S141
Acknowledgments
This work has been funded by the Thorax Foundation, Athens, Greece.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mentzelopoulos, S.D., Theodoridou, M., Malachias, S. et al. Scanographic comparison of high frequency oscillation with versus without tracheal gas insufflation in acute respiratory distress syndrome. Intensive Care Med 37, 990–999 (2011). https://doi.org/10.1007/s00134-011-2162-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2162-z