Abstract
Purpose
A high incidence of secondary adrenal insufficiency (AI) has been reported several months after a traumatic brain injury (TBI) in pediatric patients. Data from studies in adults suggest that AI may occur during the acute phase of TBI, with potential negative effects in the management of these vulnerable patients. The aim of this study was to describe the prevalence and the characteristics of AI in the acute phase of pediatric TBI.
Methods
Adrenal function was systematically evaluated in patients admitted to the pediatric intensive care unit following a TBI. Serial measurements of cortisol (9 samples) and adrenocorticotropic hormone (ACTH) were drawn from the second morning to the third morning post admission. Secondary AI was defined as all cortisols <200 nmol/l (6 μg/dl) with ACTH <12 pmol/l.
Results
Twenty-eight patients (2–15 years old) were evaluated. Secondary AI occurred in ten (36%) patients. AI was more frequent in patients with intracranial hypertension (p < 0.05). Patients with AI required longer mechanical ventilation (p < 0.05), and a non-significant trend for a higher Pediatric Logistic Organ Dysfunction score (p = 0.09) and greater norepinephrine dose (p = 0.11) was observed.
Conclusions
Secondary AI is frequent during the acute phase of pediatric TBI, particularly when intracranial hypertension is present. Systematic assessment of pituitary function after TBI appears to be essential. A randomized clinical trial is warranted to evaluate the benefits of hormonal replacement therapy in TBI patients with AI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
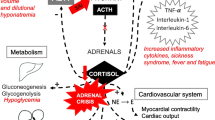
Traumatic brain injury (TBI) is a leading cause of death and disability in children [1, 2]. Maintaining homeostasis in the acute phase management of patients with TBI is crucial to prevent sequelae [1]. The vulnerable hypothalamic-pituitary axis, located in the sella turcica, can be injured following a TBI by direct (skull fracture, pituitary stalk rupture) or indirect mechanisms (hematoma, ischemia, edema) [3, 4]. Consequently, the hypothalamic-pituitary hormonal secretions can be altered, causing hypopituitarism.
A high incidence of pituitary insufficiency several months after a TBI has been reported in adult [4] and pediatric patients [5–7]. All hypothalamic-pituitary axes can be involved, and this chronic pituitary dysfunction is associated with poor recovery [4]. In the acute phase of illness, studies in adult patients suggest that hypopituitarism may occur early [8–10] and is associated with hemodynamic instability [10].
In view of the data published in adults, and considering the critical role of pituitary function in the acute phase of TBI management (especially regarding hemodynamic status and the homeostasis of water and sodium), some authors recommend systematic assessment of the pituitary function following a pediatric TBI [11, 12]. Based on adult studies and following these pediatric experts' recommendations, screening for secondary adrenal insufficiency (AI) has been included in the management protocol for patients with TBI in our Pediatric Intensive Care Unit (PICU) since May 2006.
Three years later, the objectives of this retrospective study are to describe the prevalence of AI observed in pediatric TBI following this protocol implementation and to assess the association of AI with trauma severity and with markers of organ dysfunction.
Materials and methods
Patients
Patients admitted between May 2006 and May 2009 to the PICU of Grenoble University Hospital following a TBI were eligible for the study. As the endocrine evaluation begins on the second morning after admission and lasts 24 h, patients with an expected length of PICU stay shorter than 3 days were not eligible and not explored. Patients were not included if they had preexisting adrenal or pituitary insufficiency, or if an inflicted TBI was suspected. Eligible patients were identified from the archives of PICU hospitalization for TBI, and the charts of all eligible patients were reviewed retrospectively.
The study was approved by the research ethics committee Comité d’Ethique des Centres d’Investigation Clinique de l’inter-région Rhône-Alpes-Auvergne.
TBI patient management
Patients with severe TBI were managed following a protocol derived from the “Guidelines for the acute medical management of severe TBI in infants, children, and adolescents” [13]. The targets for cerebral perfusion pressure were 40–50 mmHg in infants, 50–60 mmHg in children aged between 2 and 6 years, and 60–70 mmHg in older children. The targets for intracranial pressure were 18 mmHg in infants, 20 mmHg in older patients.
Hormonal screening
Because of the frequent loss of diurnal variation of cortisol and ACTH levels in ICU patients [14], serial serum cortisol and plasma adrenocorticotropic hormone (ACTH) were measured during a 24-h period. The first cortisol and ACTH dosages were drawn at 8 a.m. on the second morning following admission, with subsequent samples obtained every 3 h for serum cortisol (total 9 cortisol levels) and every 6 h for ACTH (total 5 levels), ending after the third morning 8 a.m. measurement. The patients were in supine position during the study. All urine output was collected during the same 24-h period for evaluation of the daily free urinary cortisol. As etomidate is known to block cortisol synthesis by specifically inhibiting the activity of 11β-hydroxylase [15, 16], resulting in a primary AI, a serum sample for 11-deoxycortisol measurement was collected at both 8 a.m. draws in patients who had received etomidate before admission.
All samples were processed in the same laboratory. Plasma cortisol was determined using automated chemoluminescence assay (Modular, Roche diagnostic, Meylan, France). Plasma ACTH was measured using radioimmunoassay (Brahms, Berlin, Germany). Plasma 11-deoxycortisol was measured using a liquid-phase tritium antibody radioimmunoassay (New England Nuclear, Boston, MA). Urinary free cortisol was measured using radioimmunoassay (Beckman coulter kit, France). The normal reference ranges (for normal non-stressed patients) are 171–536 nmol/l for plasma 8 a.m. cortisol, 2–12 pmol/l for ACTH, and 38–208 nmol/24 h for 24 h urinary free cortisol. The intra-assay and inter-assay coefficients of variation in cortisol measurement are respectively 6 and 7% in plasma and urine. For ACTH, they are respectively 5 and 8%.
Definition of adrenal insufficiency
TBI patients were defined as having secondary AI if all the serial cortisol levels were below 200 nmol/l (6 μg/dl) [11], with all ACTHs below the higher limit of normal values (12 pmol/l). In patients who had received etomidate, a drug-induced 11β-hydroxylase deficiency was considered if 11-deoxycortisol was higher than 8 nmol/l [15].
Clinical variables
Age, gender, pre-admission etomidate use, and initial post-resuscitation GCS score were recorded. TBI was considered as minor if the post-resuscitation GCS score was >13, moderate if between 9 and 13, and severe if <9. Initial severity was also assessed using the Pediatric Risk of Mortality (PRISM) score [17] and the Pediatric Trauma score [18]. Intracranial hypertension was defined as intracranial pressure higher than 20 mmHg for at least 15 min [19]. Pre-admission episodes of arterial hypotension (defined as systolic blood pressure lower than 70 mmHg + (2× age in years) [20]) and of hypoxia (defined as SaO2 < 90% [20]) were recorded. Cerebral computed tomographic (CT) findings were obtained from the neuroradiologist's conclusions on the CT scans conducted within 24 h of injury. During the 24 h of the endocrine evaluation period, organ dysfunction was assessed using the Pediatric Logistic Organ Dysfunction (PELOD) score [21]. Vasopressor requirements were also recorded during the same period. Norepinephrine was the only vasopressor used in these patients; the average dose [μg/(kg min)] of norepinephrine infused during the 24 h period was recorded. Duration of mechanical ventilation was calculated as the time from initial intubation until successful extubation (followed by 48 h without ventilatory support).
Data analysis
Data are reported as the median (25th–75th percentiles) unless otherwise specified [22]. Comparisons between AI and non-AI patient groups were performed with Mann-Whitney tests for skewed data and Fisher’s exact tests for percentages. A logistic regression analysis was conducted using AI as the dependent variable and the following potential explanatory variables: PRISM and GCS scores, etomidate use, intracranial hypertension, pre-admission hypotension or hypoxia, and CT findings. The association of AI with mechanical ventilation duration was also evaluated with a multiple regression analysis to adjust for initial severity markers (PRISM, GCS score, and intracranial hypertension). A p value <0.05 was considered to be significant. No adjustment for multiple testing was made due to the exploratory nature of the study [23], and as such, the results should be interpreted with caution.
Results
From May 2006 to May 2009, 96 patients were admitted to the PICU following a TBI. Sixty-five patients stayed less than 72 h, and 4 had inflicted TBIs, leaving 31 eligible patients. Three eligible patients only had one or two cortisol measurements and were excluded from the study (Fig. 1). Twenty-eight patients were therefore analyzed, including 22 males and 6 females. The median (25th–75th percentiles) age was 12 (10–13) years (range 2–15 years). TBI was caused by a motor vehicle accident in 14 patients, a sports accident in 10 patients, and a fall in 4. Sixteen patients had associated injuries: eight had facial trauma, seven lung contusions, six bone fractures, and two abdominal trauma. In the two patients with abdominal trauma, no sign of adrenal gland injury was evidenced on the CT scan or the ultrasound exams. Seventeen patients had a severe TBI, eight a moderate, and three a minor. Median post-resuscitation GCS was 7 (6–11); the PRISM score was 14 (12–21). Twenty patients (71%) had received etomidate before admission. Seventeen patients (61%) had at least one episode of intracranial hypertension. Norepinephrine was required in 17/17 patients with intracranial hypertension and 4/11 patients without intracranial hypertension. All patients survived the acute phase of TBI and were discharged from the hospital.
The serial cortisol levels of all the patients are presented in Fig. 2. Cortisol levels varied widely during the day, and the normal 24-h circadian rhythm was abolished in 25 (90%) patients.
Serial cortisol values in patients with normal adrenal function (a) and in patients with adrenal insufficiency (b). The grey zone illustrates the normal range of morning cortisol in non-stressed patients. All the measured cortisol values are below 200 nmol/L in patients with secondary adrenal insufficiency
Ten (36%) patients had AI (Table 1). In all AI patients, 11-deoxycortisol was below 8 nmol/l (median 2.2, range 1.9–3.2 nmol/l). The 24-h free urinary cortisol was significantly lower in patients with AI (Table 1) and was positively correlated with the mean daily plasma cortisol (p < 0.01, Spearman's correlation test; r 2 = 0.67) (Fig. 3).
Characteristics of patients with and without AI are presented in Table 1. A higher incidence of intracranial hypertension was observed in the AI group (p < 0.05) whereas the differences in PRISM, GCS, and Pediatric Trauma scores did not reach significance. No evident association between AI and etomidate use, pre-admission hypotension or hypoxia, or CT findings was observed. In a logistic regression analysis (Table 2), the only explanatory parameter significantly associated with AI occurrence was intracranial hypertension (p = 0.03).
Regarding markers of clinical instability, AI was associated with a longer duration of mechanical ventilation (p < 0.05), and a trend of higher PELOD scores (p = 0.09) and higher doses of norepinephrine (p = 0.11) was noted. After adjustment for initial severity markers, the difference in mechanical ventilation duration did not remain significant (p = 0.36).
Discussion
This study reports the systematic evaluation of corticotrophin function during the acute phase of 28 pediatric TBIs. Based on 24-h serial cortisol and ACTH measurements, 10 (36%) patients were identified as having secondary AI. AI incidence was associated with a greater TBI severity, specifically with intracranial hypertension. A longer duration of mechanical ventilation and a trend of greater norepinephrine requirements and higher PELOD scores were observed in AI patients, but these differences are probably not independent from the initial injury severity.
Previous studies
Adrenal function has been evaluated previously in the acute phase of TBI in adults. In a multicenter study including 80 patients, Cohan et al. [10] reported a prevalence of AI of 53%. An association between AI and severity of trauma, lower GCS score, and vasopressor requirements was observed [10]. In this study, the difference in initial GCS, PRISM, and Pediatric Trauma scores between patients with or without AI did not reach significance, but a clear association with intracranial hypertension was observed. In another study of adult patients with TBI, Tanriverdi et al. [9] found a lower prevalence of AI (9%), and no association with severity indicators was observed. The difference between these results and our study and Cohan’s study may be explained by differences in the studied population—the majority of the patients in this study had a mild or a moderate TBI—and in the different diagnostic criteria of AI. Bernard et al. [24] reported a prevalence of 78% of AI in a retrospective study conducted in a selected population corresponding to only 23% of the patients admitted for TBI; the prevalence of AI may have been overestimated because these patients were probably more unstable [24]. In pediatric populations, two publications have reported data on the acute phase of TBI. Using a mixed retrospective and prospective design study, Einaudi et al. [6] reported some hormonal dysfunctions in the acute post-TBI phase, including low T3 syndrome, central salt wasting syndrome, and diabetes insipidus. Low cortisol values were observed in 4 patients out of 30, but all had received steroid therapy before evaluation, and the interpretation of this result is difficult. Srinivas et al. [25] reported the prospective evaluation of pituitary-adrenal axis function in the acute phase of 37 pediatric patients with TBI, using 8 a.m. cortisol and ACTH measurements at admission, on day 3 and 7 post-injury. The etomidate use was not described. Similar to our findings, a large dispersion of cortisol levels was observed, and 46% patients were considered to have inappropriately low cortisol [25]. Interestingly, a dynamic evolution was observed in the entire group, with an initial increase of cortisol and ACTH levels at admission, followed by a normalization on day 3 and 7 [25]. Our study was conducted on day 2, and this temporal evolution may explain in part our findings. No relationship between outcome and cortisol was observed [25].
Diagnosis of AI
Diagnosis of AI in the pediatric ICU population is complex; several definitions have been proposed, but none are considered the gold standard [26]. In the particular setting of TBI, AI originates from a hypothalamic-pituitary dysfunction [3, 4, 12]; the ACTH stimulation test frequently described in other medical conditions is therefore usually considered not essential in this setting [9, 10, 12, 25]. The measurement of a repeated low level of ACTH permits identifying cases of AI consecutive to ACTH deficiency [12, 27]. An increased cortisol level is considered to be an appropriate response to stress in ICU patients [28]. Several authors have proposed to define AI in the ICU as one (or two) random cortisol measurements below a given threshold that is considered to represent an appropriate response [28]. In previous studies conducted in adults with TBI, patients were considered to have AI when one basal morning cortisol measurement was below 140 nmol/l [10], 190 nmol/l [9], or 414 nmol/l [24], or when two consecutive cortisol measurements were below 415 nmol/l [10]. In the pediatric population, some authors consider that AI should be suspected and treated if one early morning cortisol level is below 200, or 400 nmol/l when AI features are present (hypotension, hypoglycemia, hyponatremia) [11]. In the study by Srinivas et al. [25], cortisol values were considered normal between 300 and 600 nmol/l and ACTH values between 2 and 49 pg/ml. The diurnal variations of cortisol (low nocturnal secretion and high morning level) are frequently abolished in ICU patients [14, 29]. It is therefore possible that the same patient may have a single cortisol level that appears to be inappropriate to the critical situation at one moment, but demonstrate an appropriate cortisol increase a few hours later. In order to avoid overestimating the incidence of AI, we chose to measure cortisol levels nine times a day, and AI was considered only when all the cortisol levels were below the threshold proposed by Tasker et al. [11] for a single cortisol measurement (200 nmol/l). Without knowing the normal values of cortisol and ACTH in stressed pediatric ICU patients, it is possible that this method underestimates the prevalence of AI; however, we think that an overestimation of AI is improbable.
In patients with critical illness, corticosteroid binding globulin and albumin levels are commonly decreased because of hemodilution by fluid therapy and multi-organ dysfunction [30]. Plasma cortisol measurement, which reflects both the free and the protein-bound fractions of cortisol, may not always reflect actual adrenal function [30, 31]. To evaluate this possible bias, we measured the free cortisol in the 24-h urine. A good correlation was observed between the free urinary cortisol and the mean serum cortisol level; it seems therefore that the AI frequency is unlikely to be explained simply by hemodilution of binding proteins.
Pathophysiology
Different mechanisms may explain the high incidence of secondary AI reported in patients following TBI. Due to its particular vascular system, the hypothalamic-pituitary axis is highly vulnerable, despite its protected location in the bony sella turcica. The latter can be involved in skull fracture, resulting in direct injury of the pituitary gland. Moreover, restricted space around the gland facilitates local compression by tissue swelling, hematoma, or edema, which can result in ischemic lesions [3, 4]. Although some studies failed to demonstrate the correlation between AI and the initial severity of the TBI, a systematic review suggests that the prevalence of neuroendocrine dysfunction is greater in adult patients with severe TBI [4]. In this study of pediatric patients, AI occurrence is associated with intracranial hypertension, and a trend towards an association between GCS and PRISM score is observed, but this must be confirmed in a larger study. Srinivas et al. [25] reported an association between AI and frontal–temporal injuries; in the present study, no evident link with CT findings was observed.
Peripheral mechanisms are frequently involved in the development of AI during pediatric critical illness [26, 30, 32], particularly in sepsis; these mechanisms may also play a role in the acute phase post-TBI. A normal response after ACTH stimulation test would be necessary to rule out such primary AI. However, the persistently low levels of ACTH observed in all AI patients in the present study are not in favor of a peripheral origin of AI.
Etomidate use can block cortisol synthesis by inhibiting the 11β-hydroxylase in the adrenal cortex [15, 16]. Etomidate use did not differ between patients with and without AI, and no accumulation of 11-deoxycortisol occurred in patients with AI, reflecting a normal function of 11β-hydroxylase [15, 16]. Primary AI due to etomidate seems therefore improbable in the present study. The low ACTH levels observed in these patients are also highly suggestive of pituitary dysfunction.
Clinical implications
Our results are similar to data from studies in adults and suggest that AI is a frequent and under-recognized condition following pediatric TBI. The association observed between AI and markers of instability in our study as in previous study [10] suggests that AI may be deleterious. However, it is difficult from our results to differentiate the impact of AI from the consequence of intracranial hypertension, which is associated with AI. Maintaining optimal hemodynamic status is a critical part of TBI management to improve outcome [33, 34]. It therefore seems reasonable to suggest that evaluation of corticotrophin status be done systematically in the acute phase of TBI and that hydrocortisone replacement therapy be considered when AI is diagnosed [11]. Of course, it must be emphasized that only a randomized clinical trial will provide conclusive evidence of the benefit of this practice.
Limitations
Beside the aforementioned discussion about the absence of a gold standard to define AI during critical illness, the primary limitation of this study is the small sample size, reducing our ability to examine the relation between AI and clinical instability. The lack of an ACTH stimulation test limited the capacity to rule out a primary origin of AI in this context. The consequences of the retrospective nature of the study have been probably limited by the fact that a large majority of eligible patients were evaluated and that the adrenal function was always tested according to the same clinical protocol. Finally, the design of this study does not permit giving a clue concerning the time course of adrenal function following a pediatric TBI.
Conclusions
The systematic assessment of corticotrophin function during the acute phase of pediatric TBI reveals a high prevalence of AI, particularly when intracranial hypertension is present. The benefits of systematic neuroendocrine evaluation and of hormonal replacement in patients with AI warrant evaluation by a randomized clinical trial.
References
Orliaguet GA, Meyer PG, Baugnon T (2008) Management of critically ill children with traumatic brain injury. Paediatr Anaesth 18:455–461
Keenan HT, Bratton SL (2006) Epidemiology and outcomes of pediatric traumatic brain injury. Dev Neurosci 28:256–263
Maiya B, Newcombe V, Nortje J, Bradley P, Bernard F, Chatfield D, Outtrim J, Hutchinson P, Matta B, Antoun N, Menon D (2008) Magnetic resonance imaging changes in the pituitary gland following acute traumatic brain injury. Intensive Care Med 34:468–475
Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A (2007) Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a systematic review. JAMA 298:1429–1438
Acerini CL, Tasker RC (2007) Traumatic brain injury induced hypothalamic-pituitary dysfunction: a paediatric perspective. Pituitary 10:373–380
Einaudi S, Matarazzo P, Peretta P, Grossetti R, Giordano F, Altare F, Bondone C, Andreo M, Ivani G, Genitori L, de Sanctis C (2006) Hypothalamo-hypophysial dysfunction after traumatic brain injury in children and adolescents: a preliminary retrospective and prospective study. J Pediatr Endocrinol Metab 19:691–703
Poomthavorn P, Maixner W, Zacharin M (2008) Pituitary function in paediatric survivors of severe traumatic brain injury. Arch Dis Child 93:133–137
Agha A, Rogers B, Mylotte D, Taleb F, Tormey W, Phillips J, Thompson CJ (2004) Neuroendocrine dysfunction in the acute phase of traumatic brain injury. Clin Endocrinol (Oxf) 60:584–591
Tanriverdi F, Ulutabanca H, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2007) Pituitary functions in the acute phase of traumatic brain injury: are they related to severity of the injury or mortality? Brain Inj 21:433–439
Cohan P, Wang C, McArthur DL, Cook SW, Dusick JR, Armin B, Swerdloff R, Vespa P, Muizelaar JP, Cryer HG, Christenson PD, Kelly DF (2005) Acute secondary adrenal insufficiency after traumatic brain injury: a prospective study. Crit Care Med 33:2358–2366
Tasker RC (2008) Head and spinal cord trauma. In: Nichols DG (ed) Rogers’ textbook of pediatric intensive care, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 887–911
Ghigo E, Masel B, Aimaretti G, Leon-Carrion J, Casanueva FF, Dominguez-Morales MR, Elovic E, Perrone K, Stalla G, Thompson C, Urban R (2005) Consensus guidelines on screening for hypopituitarism following traumatic brain injury. Brain Inj 19:711–724
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR, Warden CR, Wright DW (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med 4:S1–S75
Marik PE, Zaloga GP (2002) Adrenal insufficiency in the critically ill: a new look at an old problem. Chest 122:1784–1796
Vinclair M, Broux C, Faure P, Brun J, Genty C, Jacquot C, Chabre O, Payen JF (2008) Duration of adrenal inhibition following a single dose of etomidate in critically ill patients. Intensive Care Med 34:714–719
den Brinker M, Hokken-Koelega AC, Hazelzet JA, de Jong FH, Hop WC, Joosten KF (2008) One single dose of etomidate negatively influences adrenocortical performance for at least 24 h in children with meningococcal sepsis. Intensive Care Med 34:163–168
Pollack MM, Ruttimann UE, Getson PR (1988) Pediatric risk of mortality (PRISM) score. Crit Care Med 16:1110–1116
Tepas JJ 3rd, Mollitt DL, Talbert JL, Bryant M (1987) The pediatric trauma score as a predictor of injury severity in the injured child. J Pediatr Surg 22:14–18
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR, Warden CR, Wright DW (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 7. Intracranial pressure monitoring technology. Pediatr Crit Care Med 4:S28–S30
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 4. Resuscitation of blood pressure and oxygenation and prehospital brain-specific therapies for the severe pediatric traumatic brain injury patient. Pediatr Crit Care Med 4:S12–S18
Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J, Gottesman R, Joffe A, Pfenninger J, Hubert P, Lacroix J, Leclerc F (2003) Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 362:192–197
Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gotzsche PC, Lang T (2001) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 134:663–694
Bender R, Lange S (2001) Adjusting for multiple testing—when and how? J Clin Epidemiol 54:343–349
Bernard F, Outtrim J, Menon DK, Matta BF (2006) Incidence of adrenal insufficiency after severe traumatic brain injury varies according to definition used: clinical implications. Br J Anaesth 96:72–76
Srinivas R, Brown SD, Chang YF, Garcia-Fillion P, Adelson PD (2009) Endocrine function in children acutely following severe traumatic brain injury. Childs Nerv Syst 24:24
Menon K, Lawson M (2007) Identification of adrenal insufficiency in pediatric critical illness. Pediatr Crit Care Med 8:276–278
Sherlock M, Ayuk J, Tomlinson JW, Toogood AA, Aragon-Alonso A, Sheppard MC, Bates AS, Stewart PM (2010) Mortality in patients with pituitary disease. Endocr Rev 19:19
Cooper MS, Stewart PM (2003) Corticosteroid insufficiency in acutely ill patients. N Engl J Med 348:727–734
Barton RN, Stoner HB, Watson SM (1987) Relationships among plasma cortisol, adrenocorticotrophin, and severity of injury in recently injured patients. J Trauma 27:384–392
Poomthavorn P, Lertbunrian R, Preutthipan A, Sriphrapradang A, Khlairit P, Mahachoklertwattana P (2009) Serum free cortisol index, free cortisol, and total cortisol in critically ill children. Intensive Care Med 35:1281–1285
Hamrahian AH, Oseni TS, Arafah BM (2004) Measurements of serum free cortisol in critically ill patients. N Engl J Med 350:1629–1638
Hebbar K, Rigby MR, Felner EI, Easley KA, Fortenberry JD (2009) Neuroendocrine dysfunction in pediatric critical illness. Pediatr Crit Care Med 10:35–40
Ducrocq SC, Meyer PG, Orliaguet GA, Blanot S, Laurent-Vannier A, Renier D, Carli PA (2006) Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med 7:461–467
Kochanek PM (2006) Pediatric traumatic brain injury: quo vadis? Dev Neurosci 28:244–255
Acknowledgments
We thank Dr. Karen Harrington for reviewing the manuscript and Mrs. Cécile Gervasoni for her assistance during the manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dupuis, C., Thomas, S., Faure, P. et al. Secondary adrenal insufficiency in the acute phase of pediatric traumatic brain injury. Intensive Care Med 36, 1906–1913 (2010). https://doi.org/10.1007/s00134-010-2012-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2012-4