Abstract
Purpose
Hypernatremia is common in the medical Intensive Care Unit (ICU) and has been described as an independent risk factor for mortality. Hypernatremia has not yet been studied in a collection of ICU patients after cardiothoracic surgery. Therefore, we wanted to determine the incidence of hypernatremia in a surgical ICU and its association with outcomes of critically ill surgical patients.
Methods
In this retrospective cohort study performed at a surgical ICU of a university hospital in Vienna, patients were admitted to the ICU after major cardiothoracic surgery between May 1999 and October 2007. Data on serum sodium in the ICU, ICU mortality, hospital mortality, and length of ICU stay were collected prospectively.
Results
2,699 patients underwent surgery during the study period, and 2,314 patients were included in the study. Two hundred twenty-one (10%) patients acquired hypernatremia during their ICU stay. Median onset of hypernatremia was on day 4 (2–7). Patients with ICU-acquired hypernatremia had a higher ICU mortality (19%) compared to patients without hypernatremia (8%; p < 0.01). Length of ICU stay was increased in patients with hypernatremia (17 vs. 3 days; p < 0.01). In a multivariate Cox regression, ICU-acquired hypernatremia was an independent risk factor for ICU mortality within 28 days.
Conclusions
Hypernatremia is a common event early in the course of critical illness after major cardiothoracic surgery and is independently associated with ICU mortality within 28 days. Future research should focus on the impact of hypernatremia on physiological functions as well as adequate and safe treatment of the electrolyte disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypernatremia is a common electrolyte disorder in critically ill patients and was recently shown to be an independent risk factor for mortality in the medical Intensive Care Unit (ICU) [1–3]. However, these studies were largely performed in medical collections of critically ill patients, and the number of hypernatremic cases was limited. Only recently has hypernatremia together with hyponatremia been studied in a collective of surgical ICU patients [4].
After (and during) major surgery, patients often receive large volumes of infusions, and their fluid management is often controlled by their physician. Therefore, this special cohort is prone to develop serum sodium concentration disorders, although the pathophysiology of hypernatremia in the surgical ICU patient is likely to be different from that of the medical ICU cohort. The incidence and effects of hypernatremia during a stay in the ICU with most patients admitted after cardiothoracic surgery have not yet been studied.
Therefore, we wanted to (1) identify the incidence of hypernatremia developing during the ICU stay after major cardiac surgery and (2) determine whether the development of hypernatremia during the ICU stay is independently associated with adverse outcomes.
Materials and methods
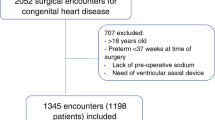
Between May 1999 and October 2007, 2,699 patients underwent open-heart surgery at the Department of Cardiothoracic Surgery, University Hospital in Vienna, Austria, as recorded in the prospectively collected database of the Department of Cardiothoracic and Vascular Anesthesia. For this analysis, we included patients who were scheduled for cardiac surgery with cardiopulmonary bypass (CPB), coronary artery bypass grafting (CABG) with or without CBP, thoracic aortic surgery with CPB, heart or lung transplant surgery, scheduled insertion of a cardiac assist device, operation on the descending aorta, or thromboendarterectomy of the pulmonary arteries. Patients with hypernatremia upon ICU admission (n = 66) and those with missing sodium values (n = 8) were excluded. We also excluded patients with a serum sodium level <130 mmol/l (n = 311) in order to rule out a confounding effect of hyponatremia, leaving 2,314 patients for analysis.
Surgery with CPB was performed according to institutional standards: crystalloid priming with 20 g of mannitol and 1,000,000 IU of aprotinin, membrane oxygenator, intermittent ante- and retrograde blood cardioplegia, and normothermic or hypothermic CPB depending on indications and surgical preferences. The endpoints were mortality in the ICU and its relation to ICU-acquired hypernatremia.
Demographic data and data acquisition of preoperative risk indicators
Preoperative patient data were collected prospectively at the time of pre-medication. Specifically, parameters that represented established risk indicators for mortality after cardiac and thoracic aortic surgery, according to the European System for Cardiac Operative Risk Evaluation (Euroscore) [5], were recorded. Severity of illness was estimated by the Simplified Acute Physiology Score (SAPS) II [6]. Additional risk indicators were body mass index, serum creatinine and preoperative dysnatremia.
The study protocol was approved by institutional review. Since no additional interventions were performed and no individual data were analyzed, the need for informed consent was waived.
Definition of ICU-acquired hypernatremia
Serum sodium routinely measured every morning at 05:00 am was used for the analysis. Hypernatremia was defined as a serum sodium level exceeding 145 mmol/l [7]. Patients with serum sodium levels exceeding 145 mmol/l in the first dataset after admission were considered to have hypernatremia upon admission. Patients were considered to have ICU-acquired hypernatremia when initially normal serum sodium rose above 145 mmol/L during the course of the ICU stay. Serum sodium was measured by ion-selective electrodes in a Hitachi 747 analyzer (Roche, Basel, Switzerland).
Statistical analysis
The statistical methods are given in the electronic repository.
Results
A total of 2,314 patients were included in the cohort. Most patients had undergone coronary and/or valvular surgery. The median ICU length of stay was 3 (1–10) days (median and 1st to 3rd quartiles), and overall ICU mortality was 9%. The standardized observed to expected mortality ratio based on the EUROSCORE was 1.29 (1.14–1.44; 95% CI). The demographic and surgical characteristics, stratified by vital status on ICU discharge, are shown in Table 1.
Incidence of ICU-acquired hypernatremia
During ICU treatment, 221 patients (10%) acquired hypernatremia. The cumulative incidence of ICU-acquired hypernatremia is shown in Fig. 1. The onset of the first ICU-acquired hypernatremic episode was on day 4 (2–7) after ICU admission (median and 1st to 3rd quartiles) (Fig. 1) and lasted 2 (0–5) days (median and 1st to 3rd quartiles). The maximum and mean serum sodium concentrations during this first episode of ICU-acquired hypernatremia were 150 ± 5 and 148 ± 3 mmol/l, respectively.
Relationship between ICU-acquired hypernatremia and outcome
Patients who died in the ICU had a higher SAPS II score, higher Euroscore, lower BMI, longer surgery length, higher preoperative sodium, and higher postoperative lactate level. Preoperative hypernatremia was also more common in non-survivors. Non-survivors also differed with respect to surgery type (Table 1).
Patients with ICU-acquired hypernatremia had a higher ICU mortality (19%) compared to patients without ICU-acquired hypernatremia (8%; p < 0.01). Moreover, the ICU stay was longer when patients developed hypernatremia (17 vs. 3 days; p < 0.01). Compared to patients without ICU-acquired hypernatremia, patients with ICU-acquired hypernatremia had an increased preoperative risk (as measured by the Euroscore) and an increased illness severity at ICU admission (as measured by the SAPS II score) (Table 2). The ICU mortality within 28 days according to quartiles of maximum serum sodium in the ICU is shown in Fig. 2.The Kaplan-Meier survival curve shows that patients with ICU-acquired hypernatremia had lower hospital survival rates than patients without ICU-acquired hypernatremia (Fig. 3, log rank test: p = 0.02).
Unadjusted 28-day ICU mortality and 95% confidence intervals according to quartiles of maximum serum sodium in the ICU. Chi-square test for trend: p < 0.01. Mean and standard deviation of maximum serum sodium in the 1st, 2nd, 3rd and 4th quartile is 135 ± 1, 138 ± 1, 140 ± 1 and 146 ± 4 mmol/l, respectively
Univariate Cox regression analysis revealed a statistically significant association of ICU-acquired hypernatremia on ICU mortality within 28 days: hazard ratio = 4.32 (95% confidence interval = 2.98–6.30). In the multivariable Cox regression model, ICU-acquired hypernatremia was independently associated with an increased probability of mortality after adjustment for the SAPS II score, Euroscore, length of surgery, surgery type and maximum lactate level within the first 24 h following surgery (Table 3). No effect was found for age, sex, preoperative hypernatremia or preoperative creatinine level with respect to mortality. Quartiles of maximum serum sodium showed an independent effect on ICU mortality within 28 days in an unadjusted Cox regression treating maximum serum sodium as a time-fixed risk factor (hazard ratio 2.2, 95% CI 1.9–2.6, p < 0.01). However, when adjusted for the time-varying variable (hypernatremia yes/no) and for the other confounders (Table 3), quartiles of maximum serum sodium no longer showed an association with mortality. Specifically, we could not demonstrate an increased risk dependent on the severity of ICU-acquired hypernatremia (data not shown).
The matched case-control study showed an association of ICU-acquired hypernatremia on hospital mortality [matched odds ratio 2.55 (1.23–5.67; 95% CI); p < 0.01], but not on ICU mortality [matched odds ratio 2.38 (0.99–6.27; 95% CI); p = 0.05].
Discussion
In this study we show that ICU-acquired hypernatremia is a common event in ICU patients after cardiothoracic surgery that occurs early in the course of critical illness and is associated with increased mortality in these patients.
Unlike hyponatremia, hypernatremia is consistently associated with hyperosmolarity [8]. Hypernatremia thereby results in cellular dehydration leading to disturbances of a different origin. The most prominent consequence of hypernatremia is cerebral shrinkage, leading to neurological impairment or even vascular rupture and cerebral hemorrhage [7]. Moreover, weakness, muscle cramping, a decrease in left ventricular contractility, disturbances in glucose metabolism and immunologic functions have been described [9–13].
Hypernatremia develops either by free water loss or a gain or retention of sodium. However, hypernatremia does not develop in healthy individuals who have a normal defense mechanism against hyperosmolality—thirst [14]. In critically ill medical and surgical patients, impaired thirst sensation is common due to intubation, sedation and loss of consciousness. Therefore, fluid management is handled by the physician. However, the high incidence of hypernatremia in critically ill patients compared to patients in non-ICU wards reflects either poor fluid management or the belief that sodium levels are irrelevant [1, 2, 15]. Thus, hypernatremia in critically ill patients is regarded as an indicator of quality of care [2], which more or less considers hypernatremia to be an iatrogenic problem. This study clearly shows the independent effect of increased serum sodium levels on outcomes of surgical ICU patients, suggesting that rising serum sodium levels must not be neglected.
The incidence of 10% of hypernatremia found in this study on patients after cardiothoracic surgery is comparable to that found in a previous study of medical ICU patients [1]. As expected, mortality is lower in this cohort of surgical patients than in medical ICU patients [1–3]. ICU-acquired hypernatremia was independently associated with adverse outcomes in this study of surgical ICU patients, supporting previous results showing that hypernatremia has an effect on mortality, independent of the underlying disease or disease severity [1–3].
Both the Cox regression as well as the log-rank statistic treat ICU-acquired hypernatremia as a time-varying risk factor, thus eliminating the immortal-time bias. Since all types of analysis yield comparable results with regard to the effect of ICU-acquired hypernatremia on mortality, the main message of the paper is probably unaffected by this type of bias.
Moreover, in this study, we were able to exclude factors that were supposed to be responsible for the excess mortality of patients with ICU-acquired hypernatremia: due to the matched case control design, it was possible for us for the first time to show that even after adjustment for acute renal failure, the application of furosemide, plasma lactate levels and base excess that ICU-acquired hypernatremia is independently associated with mortality.
Interestingly, the severity of hypernatremia was not associated with additional mortality risk. This finding may be explained by the correlation between the time during which hypernatremia developed and its symptoms; the rapid development of hypernatremia does not offer enough time for compensatory mechanisms (e.g., shift of osmoles).
Our study is limited by the fact that the patients with hypernatremia were not stratified by the cause of hypernatremia for statistical analysis, which may have provided further insight into whether hypernatremia itself or its causes are responsible for the markedly increased mortality in these patients. This analysis would require a case-by-case review of all hypernatremic patients. This type of analysis is possible given that all necessary data (e.g., urine electrolytes, total daily volume, electrolyte input and output) are available. However, such analysis is almost impossible in the case of the given study since the patient number exceeds the possibility to perform a case-by-case review. Additionally, we excluded severe hyponatremia and hypernatremia at ICU admission from our study since the data indicate that both entities are associated with increased mortality [1, 16]. A potential influence of recurring hypernatremic episodes on patient outcomes was not assessed statistically. Moreover, the excess mortality (SMR 1.29 according to EUROSCORE) observed in our study group limits the generalizability of our results.
Emphasis on future research should be on testing whether aggressive treatment of hypernatremia leads to better outcome in patients with ICU-acquired hypernatremia as well as in patients with hypernatremia on admission to the ICU.
In conclusion, hypernatremia is common in patients after cardiothoracic surgery and is independently associated with mortality, supporting previously published data on critically ill patients in a medical ICU. ICU-specific strategies should be developed to recognise and prevent hypernatremia or to assess hypernatremic etiologies that will allow physicians to treat this common electrolyte disorder effectively.
References
Lindner G, Funk GC, Schwarz C, Kneidinger N, Kaider A, Schneeweiss B, Kramer L, Druml W (2007) Hypernatremia in the critically ill is an independent risk factor for mortality. Am J Kidney Dis 50:952–957
Polderman KH, Schreuder WO, Strack van Schijndel RJ, Thijs LG (1999) Hypernatremia in the intensive care unit: an indicator of quality of care? Crit Care Med 27:1105–1108
Hoorn EJ, Betjes MG, Weigel J, Zietse R (2008) Hypernatraemia in critically ill patients: too little water and too much salt. Nephrol Dial Transplant 23:1562–1568
Stelfox HT, Ahmed SB, Khandwala F, Zygun D, Shahpori R, Laupland K (2008) The epidemiology of intensive care unit-acquired hyponatraemia and hypernatraemia in medical-surgical intensive care units. Crit Care 12:R162
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R (1999) European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 16:9–13
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Adrogue HJ, Madias NE (2000) Hypernatremia. N Engl J Med 342:1493–1499
Rose BD (2001) Clinical physiology of acid-base and electrolyte disorders. McGraw-Hill, New York
Knochel JP (1982) Neuromuscular manifestations of electrolyte disorders. Am J Med 72:521–535
Lenz K, Gossinger H, Laggner A, Druml W, Grimm G, Schneeweiss B (1986) Influence of hypernatremic-hyperosmolar state on hemodynamics of patients with normal and depressed myocardial function. Crit Care Med 14:913–914
Kozeny GA, Murdock DK, Euler DE, Hano JE, Scanlon PJ, Bansal VK, Vertuno LL (1985) In vivo effects of acute changes in osmolality and sodium concentration on myocardial contractility. Am Heart J 109:290–296
Bratusch-Marrain PR, DeFronzo RA (1983) Impairment of insulin-mediated glucose metabolism by hyperosmolality in man. Diabetes 32:1028–1034
Kuroda T, Harada T, Tsutsumi H, Kobayashi M (1997) Hypernatremic suppression of neutrophils. Burns 23:338–340
Halperin ML (1999) Fluid, electrolyte and acid–base physiology: a problem-based approach. WB Saunders, Philadelphia
Palevsky PM, Bhagrath R, Greenberg A (1996) Hypernatremia in hospitalized patients. Ann Intern Med 124:197–203
Bennani SL, Abouqal R, Zeggwagh AA, Madani N, Abidi K, Zekraoui A, Kerkeb O (2003) Incidence, causes and prognostic factors of hyponatremia in intensive care. Rev Med Interne 24:224–229
Acknowledgments
We thank the Department of Cardiothoracic and Vascular Anesthesia medical staff for their contributions to the database. No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was undertaken at the Cardiothoracic Surgical ICU, Medical University of Vienna.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lindner, G., Funk, GC., Lassnigg, A. et al. Intensive care-acquired hypernatremia after major cardiothoracic surgery is associated with increased mortality. Intensive Care Med 36, 1718–1723 (2010). https://doi.org/10.1007/s00134-010-1968-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1968-4