Abstract
Purpose
To compare the effects of two arginine vasopressin (AVP) dose regimens on the hemodynamic response, catecholamine requirements, AVP plasma concentrations, organ function and adverse events in advanced vasodilatory shock.
Methods
In this prospective, controlled, open-label trial, patients with vasodilatory shock due to sepsis, systemic inflammatory response syndrome or after cardiac surgery requiring norepinephrine >0.6 μg/kg/min were randomized to receive a supplementary AVP infusion either at 0.033 IU/min (n = 25) or 0.067 IU/min (n = 25). The hemodynamic response, catecholamine doses, laboratory and organ function variables as well as adverse events (decrease in cardiac index or platelet count, increase in liver enzymes or bilirubin) were recorded before, 1, 12, 24 and 48 h after randomization. A linear mixed effects model was used for statistical analysis in order to account for drop-outs during the observation period.
Results
Heart rate and norepinephrine requirements decreased while MAP increased in both groups. Patients receiving AVP at 0.067 IU/min required less norepinephrine (P = 0.006) than those infused with AVP at 0.033 IU/min. Arterial lactate and base deficit decreased while arterial pH increased in both groups. During the observation period, AVP plasma levels increased in both groups (both P < 0.001), but were higher in the 0.067 IU/min group (P < 0.001) and in patients on concomitant hydrocortisone. The rate of adverse events and intensive care unit mortality was comparable between groups (0.033 IU/min, 52%; 0.067 IU/min, 52%; P = 1).
Conclusions
A supplementary AVP infusion of 0.067 IU/min restores cardiovascular function in patients with advanced vasodilatory shock more effectively than AVP at 0.033 IU/min.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since 1997 [1], arginine vasopressin (AVP) has been used as a supplementary vasopressor in patients with advanced vasodilatory shock [2, 3]. While AVP repeatedly proved effective in restoring cardiovascular function in shock states poorly responsive or even resistant to catecholamine therapy [1–7], no benefit of a supplementary AVP infusion on septic shock survival was found in the Vasopressin in Septic Shock Trial (VASST) [8]. Nonetheless, an à priori defined subgroup analysis suggested that AVP improved outcome in patients with less severe septic shock [8] and in those treated with concomitant low dose hydrocortisone [9]. In the latest guidelines, the Surviving Sepsis Campaign suggests that AVP may be added as an adjunct vasopressor agent when hemodynamic instability persists despite escalating norepinephrine doses [10].
Although several clinical studies investigated the effects of AVP in vasodilatory shock [1–7], little is known about the optimal AVP dose to counteract vasodilation. Identification of this AVP dose could help to optimize hemodynamic effects while keeping adverse effects at a minimum. So far, varying AVP doses between 0.01 and 2 IU/min have been used [1–7, 11]. In the VASST study, AVP was infused at 0.01–0.03 IU/min [8]. The Surviving Sepsis Campaign recommends infusing AVP at 0.03 IU/min [10]. However, no comparisons between different AVP doses have yet been prospectively investigated. So far, one retrospective analysis has evaluated the hemodynamic effects of two AVP doses and observed that AVP at 0.067 IU/min was more effective to reverse cardiovascular failure in advanced vasodilatory shock than 0.033 IU/min [12].
We hypothesized that AVP at 0.067 IU/min could restore cardiovascular function more effectively than AVP at 0.033 IU/min. In this randomized, controlled, open-label trial, the effects of two AVP doses (0.033 vs. 0.067 IU/min) on the hemodynamic response, organ function and adverse events were prospectively compared in advanced vasodilatory shock patients.
Patients and methods
This prospective, randomized, controlled, open-label trial was performed in a 23-bed general and surgical intensive care unit in a tertiary teaching hospital from 1 January 2008 until 31 December 2008. The study protocol was approved by the institutional review board and the Ethics Committee of the Innsbruck Medical University (UN 3052_LEK; EudraCT: 2007-005010-40). Written informed consent was obtained from the patients’ next of kin or the legal representative. In all surviving patients, written informed consent was obtained after recovery.
Inclusion and exclusion criteria
Critically ill patients were considered eligible to participate in the study if they presented with vasodilatory shock due to sepsis, systemic inflammatory response syndrome (SIRS) or cardiac surgery and required norepinephrine doses >0.6 μg/kg/min to maintain MAP >60 mmHg. Patients <18 years, in a moribund state unlikely to survive >12 h, in whom intensive care therapy was withdrawn or limited in an end-of-life decision, who received AVP or any of its analogues because of other diagnoses than vasodilatory shock, participated in another clinical trial, were pregnant or refused written informed consent were excluded. Patients had to be included within 12 h after their norepinephrine demand exceeded 0.6 μg/kg/min or within 12 h after intensive care unit admission (in case norepinephrine doses exceeded 0.6 μg/kg/min before intensive care unit admission).
Definitions
Vasodilatory shock was defined as the simultaneous presence of adequate systemic blood flow (cardiac index >2–2.5 l/min/m2, mixed venous oxygen saturation >60%, or an ejection fraction >50% together with a heart rate >80 bpm in the absence of severe diastolic dysfunction on echocardiography), a mean arterial blood pressure (MAP) <60 mmHg in volume-resuscitated patients together with a systemic vascular resistance index <1,200 dyne*s/cm5*m² resulting in the need for norepinephrine >0.1 μg/kg/min for >12 h. Sepsis and SIRS were defined according to the criteria suggested by the American College of Chest Physicians and the Society of Critical Care Medicine [13].
Hemodynamic management
Study patients were routinely monitored with an arterial and central venous line. A pulmonary artery or transpulmonary thermodilution catheter (PiCCO plus®; Pulsion, Munich, Germany) was inserted at the discretion of the attending physician. Transesophageal echocardiography was done at least once in all study patients for diagnostic reasons and to guide hemodynamic management. Volume resuscitation was performed according to the response of filling pressures (e.g., central venous pressure, pulmonary arterial occlusion pressure) and stroke volume/cardiac index to repetitive fluid loading using gelatine-based colloids (Gelofusin®; B. Braun, Melsungen, Germany). If the cardiac index remained <2–2.5 l/min/m² or mixed venous oxygen saturation <60% despite adequate volume resuscitation and/or blood transfusion, milrinone (0.3–0.7 μg/kg/min) and/or epinephrine was continuously infused. After ensuring adequate systemic blood flow using fluids and/or inotropes, norepinephrine (Arterenol®; Sanofi-Aventis, Frankfurt, Germany) was infused to increase MAP >60–65 mmHg. Hydrocortisone (200–300 mg/day) was added as a continuous infusion if escalating norepinephrine doses could not stabilize hemodynamic function. Intubated patients on mechanical, assisted or spontaneous breathing were sedated by infusing either sufentanil and midazolam, or morphine alone. Continuous veno-venous hemofiltration was employed for renal indications only. Causative and supportive sepsis therapy was performed according to the Surviving Sepsis Campaign guidelines [10]. Activated protein C was not administered.
Randomization and study groups
Based on a computer-generated list, patients were randomly allocated to one of the two study groups. The first group received AVP at 0.067 IU/min, while AVP was infused at 0.033 IU/min in the second group. Clinicians and researchers were not blinded to the study group allocation. No bolus injections of AVP were given in any group. After initiation of AVP (Pressyn®; Ferring Inc, Toronto, Canada), norepinephrine infusion was adapted to maintain MAP >60–65 mmHg in both groups. If norepinephrine could be decreased <0.2 μg/kg/min, AVP was slowly tapered off at the discretion of the attending physician. Simultaneously, norepinephrine doses could be further reduced. No crossover between study groups was allowed during the 48-h observation period.
Data collection
Demographic data, pre-existent chronic diseases, admission diagnosis, duration of AVP infusion, need for continuous veno-venous hemofiltration, length of intensive care unit stay, intensive care unit and 28-day mortality were documented. A modified Goris multiple organ dysfunction syndrome score [14] and the Sepsis-related Organ Failure Assessment score [15] were calculated from most aberrant clinical and laboratory variables during the intensive care unit stay.
The following hemodynamic variables were recorded before, 1, 12, 24 and 48 h after randomization: heart rate, MAP, central venous pressure, mean pulmonary arterial pressure, pulmonary arterial occlusion pressure, cardiac index, stroke volume index and mixed venous oxygen saturation. Norepinephrine, epinephrine and milrinone requirements were documented at the same intervals. The systemic vascular resistance index was calculated using the standard formula. Platelet count, plasma levels of aspartate and alanine aminotransferase, total bilirubin, creatinine, urea, troponin T, AVP and prolactin were collected before, 24 and 48 h after the start of AVP therapy. For hormone analyses, plasma samples were immediately frozen at −70°C and transferred to the endocrinologic laboratory after completion of patient recruitment. AVP levels were determined using a conventional radioimmunoassay (DRG Diagnostics, Marburg, Germany) [16]. Prolactin was measured with an enzyme-linked immunosorbent assay (DRG Diagnostics, Marburg, Germany). Hemoglobin levels, arterial pH, lactate concentrations, base deficit and the partial arterial oxygen tension/fractional inspiratory oxygen concentration ratio were recorded before, 1, 12, 24 and 48 h after randomization. Occurrence of adverse events (>5% increase in liver enzymes or total bilirubin levels or >5% decrease in platelet count or cardiac index during the 48 h observation period compared to randomization values) was evaluated in all study patients.
Study endpoints
The primary endpoint was to compare the hemodynamic response to AVP at two doses (0.033 vs. 0.067 IU/min). Secondary endpoints included differences in organ function and laboratory variables, AVP and prolactin plasma levels as well as the rate of adverse events.
Statistical analysis
Based on the results of a retrospective study [10], a sample size of 22 patients per group was required to detect a significant difference in the hemodynamic response (MAP increase, norepinephrine decrease) between AVP at 0.033 and 0.067 IU/min (alpha error, 0.05; beta error, 0.2; power, 80%).
The SPSS 13.0 software program (SPSS Inc; Chicageo, IL) was used for statistical analysis. Normality distribution was assessed by the Kolmogorov–Smirnov test. In case the normality assumption was not fulfilled (aspartate and alanine aminotransferase, total bilirubin, troponin T, AVP, prolactin), variables were ln-transformed. All group comparisons were performed as intention-to-treat analyses. The unpaired Student’s t (continuous) or Fisher’s exact test (categorical) was used to compare demographic and clinical parameters as well as the rate of adverse events between groups. To compare the hemodynamic response, changes in laboratory variables as well as plasma hormone levels over time between groups, a linear mixed effects model was applied to account for drop-outs during the observation period [17]. If hemodynamic and laboratory variables showed group differences (P < 0.1) before randomization, the baseline value of the corresponding variable (stroke volume index, cardiac index, systemic vascular resistance index, mixed venous oxygen saturation, milrinone requirements) was entered as a covariate into the mixed effects model. P-values <0.05 were considered to indicate statistical significance. All variables are given as mean values ± SD, if not otherwise indicated.
Results
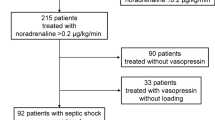
Sixty-one patients met the inclusion criteria during the observation period, of which 50 patients were enrolled (Fig. 1). A pulmonary artery or transpulmonary thermodilution catheter was in place in 16 and 13 patients in the 0.033 and 0.067 IU/min group, respectively (P = 0.57). All patients were included within 7 ± 5 h after their norepinephrine requirements exceeded 0.6 μg/kg/min or intensive care unit admission. There were no differences in demographic and clinical variables between groups before randomization (Table 1). Six patients in the 0.033 IU/min group and four patients in the 0.067 IU/min group died during the observation period (P = 0.73). Intensive care unit mortality was 52% (13/52) in both groups (P = 1).
Heart rate (0.033 IU/min, P = 0.001; 0.067 IU/min, P < 0.001) and norepinephrine requirements (0.033 IU/min, P = 0.03; 0.067 IU/min, P = 0.001) decreased, while MAP increased in both groups (0.033 IU/min, P = 0.02; 0.067 IU/min, P < 0.001) (Table 2). Patients receiving AVP at 0.067 IU/min required less norepinephrine during the study period when compared to the 0.033 IU/min group. Throughout the study period, mixed venous oxygen saturation was lower in the 0.033 than in the 0.067 IU/min group. While mixed venous oxygen saturation remained unchanged in the 0.033 IU/min group (P = 0.75), it tended to decrease in the 0.067 IU/min group (P = 0.12). Simultaneous hydrocortisone therapy did not influence the hemodynamic response to AVP in both groups (both P > 0.05).
Arterial lactate levels (0.033 IU/min, P = 0.05; 0.067 IU/min, P = 0.04) and base deficit (0.033 IU/min, P < 0.001; 0.067 IU/min, P = 0.001) decreased, while arterial pH increased in both groups (0.033 IU/min, P < 0.001; 0.067 IU/min, P < 0.001). Platelets fell in both groups, but the decrease was only significant in patients treated with 0.033 IU/min of AVP (0.033 IU/min, P = 0.02; 0.067 IU/min, P = 0.18). Patients in the 0.067 IU/min group had lower plasma troponin levels and base deficits than patients allocated to the 0.033 IU/min group (Table 3). The rate of adverse events during AVP infusion was comparable between groups (Table 4).
AVP plasma levels increased in both groups (both P < 0.001) but were higher in the 0.067 IU/min group (P < 0.001) (Fig. 2). Study patients on concomitant hydrocortisone therapy exhibited higher AVP levels than patients who did not receive hydrocortisone in both groups (Fig. 3). Prolactin plasma levels tended to increase in both groups during AVP infusion (0.033 IU/min, P = 0.05; 0.067 IU/min, P = 0.06). There was no difference in the course of prolactin plasma levels between the two AVP groups (P = 0.98).
Arginine vasopressin and prolactin plasma levels in patients receiving AVP at 0.033 IU/min (dots) and 0.067 IU/min (squares). AVP plasma levels increased in both study groups (both P < 0.001). The increase was more pronounced in patients receiving AVP at 0.067 IU/min (squares) when compared to patients receiving AVP at 0.033 IU/min (dots) (P < 0.001). There was no group difference in prolactin plasma levels (P = 0.98). Absolute values of AVP (pmol/l) were: 0 h: 0.033 IU/min, 15.9 ± 24.7; 0.067 IU/min, 13.9 ± 6.3; 24 h: 0.033 IU/min, 114.7 ± 56.2; 0.067 IU/min, 262 ± 138.2; 48 h: 0.033 IU/min, 98.8 ± 46; 0.067 IU/min, 216.5 ± 125.7
Arginine vasopressin plasma levels in patients with (triangle) and without concomitant hydrocortisone therapy (diamond) in both study groups. Arginine vasopressin (AVP) plasma levels significantly increased in both groups after start of AVP therapy (both P < 0.001), but the increase was more pronounced if patients received a concomitant hydrocortisone therapy (AVP 0.033 IU/min, P = 0.05; AVP 0.067 IU/min, P = 0.04). Absolute values of AVP (pmol/l) were: AVP 0.033 IU/min: 0 h: no HC, 9.8 ± 7.9; HC, 21.5 ± 33.1; 24 h: no HC, 103.3 ± 72.8; HC, 123.9 ± 39.2; 48 h: no HC, 100.6 ± 56.1; HC, 97.3 ± 39.3; AVP 0.067 IU/min: 0 h: no HC, 12.5 ± 5.9; HC, 15.1 ± 6.7; 24 h: no HC, 216.5 ± 128.1; HC, 318.9 ± 136.6; 48 h: no HC, 191.9 ± 123.1; HC, 234.9 ± 132.8
Discussion
The main findings of this randomized, controlled, open-label trial were that a supplementary AVP infusion increased MAP and decreased heart rate in advanced vasodilatory shock irrespective of the dose infused. The reduction of norepinephrine requirements was more pronounced in patients treated with AVP at 0.067 than 0.033 IU/min. While the incidence of adverse events was comparable between groups, base deficit and troponin levels were higher in patients receiving AVP at 0.033 IU/min.
As previously reported [1–7], an increase in MAP and a reduction in heart rate as well as norepinephrine requirements occurred in both groups after initiation of AVP. Simultaneously, arterial pH, lactate levels and base deficit improved, suggesting enhanced tissue perfusion. Lower norepinephrine demands together with comparable MAP levels confirm our hypothesis that 0.067 IU/min of AVP could restore cardiovascular functions more effectively than AVP at 0.033 IU/min. The lacking difference in MAP between groups can be explained by the fact that this variable was used to guide vasopressor therapy. The results of the endocrinologic analysis revealed higher AVP plasma levels in patients receiving 0.067 IU/min of AVP than during AVP infusion at 0.033 IU/min. This together with the finding that AVP plasma levels and norepinephrine requirements in all study patients were indirectly correlated (Spearman-rho correlation coefficient, −0.49; P < 0.001) confirms dose-dependent hemodynamic effects of AVP in vasodilatory shock.
So far, one retrospective analysis has addressed the effects of different AVP doses in vasodilatory shock [12]. This analysis revealed similar results and was performed in a comparable patient population. Including 78 subjects, it suggested that patients treated with 0.067 IU/min of AVP displayed a higher MAP and lower central venous pressure, mean pulmonary arterial pressure and norepinephrine requirements than patients receiving AVP at 0.033 IU/min [12]. The results of that and the present study are in contrast to the findings of a case series in 50 septic shock patients [18]. In that analysis, Holmes et al. reported adverse events in five patients treated with AVP at doses >0.04 IU/min and concluded that AVP should not be used at higher doses. Unlike the present trial, the latter analysis was uncontrolled, observational and did not prove a causative relationship between the occurrence of adverse events and AVP doses >0.04 IU/min [18].
Even though our study included enough patients to detect differences in the hemodynamic response between groups, it was underpowered to investigate effects on patient outcome. Since there is no proven link between the duration of norepinephrine weaning and improved outcome in septic or vasodilatory shock, no conclusions on the effects of AVP doses on patient outcome can be drawn from our results. So far, the multicentered VASST trial was the only study investigating the effects of AVP on mortality [8]. Considering that all study patients in our trial suffered from “more severe” vasodilatory shock (according to the VASST criteria), it is possible that AVP doses applied in the VASST study (0.01–0.03 IU/min) were too low. This hypothesis is supported by a recent post hoc analysis of the VASST database indicating that combined AVP and corticosteroid therapy was associated with decreased mortality and organ dysfunction than norepinephrine and corticosteroids [9]. In line with our results, combined administration of low-dose corticosteroids and AVP resulted in higher AVP plasma levels than infusion of AVP alone [9]. Although our data cannot identify the mechanism for this observation, steroid-induced inhibition of vasopressin degradation may be a possible explanation.
Although higher AVP doses appear to allow more rapid and pronounced reductions in norepinephrine support, it is possible that such a dose regime induces more adverse events thereby counterbalancing beneficial cardiovascular effects. The results of the current trial suggest that the rate of adverse events was not different between the two AVP doses. It must, however, be considered that our patient population is too small to reliably exclude differences in adverse events between groups.
The most important limitation of our analysis was that important hemodynamic variables differed between groups before randomization. Therefore, group comparisons over time had to be corrected for certain baseline differences. Although this is an accepted statistical method to compensate for group differences at randomization, it limits data interpretation. In our trial, this is particularly relevant for interpreting differences in heart function between the two study groups. It appears that patients allocated to the 0.033 IU/min group suffered from more chronic heart diseases. This could explain why at randomization indices of systemic blood flow were lower and milrinone requirements higher in this group when compared to patients receiving AVP at 0.067 IU/min. Accordingly, these baseline differences do not allow drawing firm clinical conclusions on the effects of the two AVP dose regimes on heart function. However, the observation that troponin levels increased in patients receiving lower AVP doses while they remained unchanged in the 0.067 IU/min group may point at beneficial effects of a more pronounced reduction of norepinephrine infusion and by that adrenergic stress on the heart [19, 20]. However, this finding must be considered preliminary and hypothesis-generating, since future trials are required to further elucidate this endpoint. Similarly, it is unclear whether decreasing mixed venous oxygen saturation in the 0.067 IU/min group represented reversal of hyperdynamic blood flow or a clinically relevant reduction of systemic oxygen supply.
A strength of this clinical investigation is its randomized, controlled design. Only few patients could not be enrolled because either exclusion criteria were present or written informed consent was denied suggesting minimal selection bias [21]. In accordance with results of the power analysis, the trial included an adequate number of patients to uncover differences in the hemodynamic response between the two AVP doses. The fact that study group allocation was not blinded is a weakness of our study, and we cannot exclude that a treatment-bias originating from the open-label design has influenced the study results. Since the majority of patients in both study groups were either on continuous veno-venous hemofiltration or received diuretics during the observation period, we could not compare the effects of different AVP dose regimes on urine output and net fluid balance. Furthermore, it is impossible to assess whether the preference of dobutamine as the first-line inotrope and use of activated protein C would have been more effective to resuscitate our study patients.
In conclusion, a supplementary AVP infusion of 0.067 IU/min can restore cardiovascular function in advanced vasodilatory shock more effectively than AVP at 0.033 IU/min. Future trials including more patients are warranted to evaluate the effects of AVP at 0.067 IU/min on the overall outcome of patients with advanced vasodilatory shock secondary to systemic inflammation.
References
Landry DW, Levin HR, Gallant EM, Seo S, D’Alessandro D, Oz MC, Oliver JA (1997) Vasopressin pressor hypersensitivity in vasodilatory septic shock. Crit Care Med 25:1279–1282
Mutlu GM, Factor P (2004) Role of vasopressin in the management of septic shock. Intens Care Med 30:1276–1291
Lange M, Ertmer C, Westphal M (2008) Vasopressin vs. terlipressin in the treatment of cardiovascular failure in sepsis. Intens Care Med 34:821–832
Jerath N, Frndova H, McCrindle BW, Gurofsky R, Humpl T (2008) Clinical impact of vasopressin infusion on hemodynamics, liver and renal function in pediatric patients. Intens Care Med 34:1274–1280
Dünser MW, Mayr AJ, Ulmer H, Ritsch N, Knotzer H, Pajk W, Luckner G, Mutz NJ, Hasibeder WR (2001) The effects of vasopressin on systemic hemodynamics in catecholamine-resistant septic and postcardiotomy shock: a retrospective analysis. Anesth Analg 93:7–13
Luckner G, Dünser MW, Jochberger S, Mayr VD, Wenzel V, Ulmer H, Schmid S, Knotzer H, Pajk W, Hasibeder W, Mayr AJ, Friesenecker B (2005) Arginine vasopressin in 316 patients with advanced vasodilatory shock. Crit Care Med 33:2659–2666
Dünser MW, Mayr AJ, Hanno U, Knotzer H, Sumann G, Pajk W, Friesenecker B, Hasibeder WR (2003) Arginine vasopressin in advanced vasodilatory shock: a prospective, randomized, controlled study. Circulation 107:2313–2319
Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D, VASST Investigators (2008) Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 358:877–887
Russell JA, Walley KR, Gordon AC, Cooper DJ, Hébert PC, Singer J, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Dieter Ayers for the Vasopressin, Septic Shock Trial Investigators (2009) Interaction of vasopressin infusion, corticosteroid treatment and mortality of septic shock. Crit Care Med 37:811–818
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intens Care Med 34:17–60
Klinzing S, Simon M, Reinhart K, Bredle DL, Meier-Hellmann A (2003) High-dose vasopressin is not superior to norepinephrine in septic shock. Crit Care Med 31:2646–2650
Luckner G, Mayr VD, Jochberger S, Wenzel V, Ulmer H, Hasibeder WR, Dünser MW (2007) Comparison of two dose regimes of arginine vasopressin in advanced vasodilatory shock. Crit Care Med 35:2280–2285
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organfailure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Goris RJA, te Boekhorst TPA, Nuytinck JKS, Gimbrère JS (1985) Multiple-organ failure. Arch Surg 120:1109–1115
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intens Care Med 22:707–710
Beardwell CG (1971) Radioimmunoassay of arginine vasopressin in human plasma. J Clin Endocrinol Metab 33:254–260
Laird NM, Ware JH (1982) Random effects models for longitudinal data. Biometrics 38:963–974
Holmes CL, Walley KR, Chittock DR, Lehman T, Russell JA (2001) The effects of vasopressin on hemodynamics and renal function in severe septic shock: a case series. Intens Care Med 27:1416–1421
Dünser MW, Hasibeder WR (2009) Sympathetic overstimulation during critical illness: adverse effects of adrenergic stress. J Intensive Care Med, 23 Aug [Epub ahead of print]
Goldspink DF, Burniston JG, Ellison GM, Clark WA, Tan LB (2004) Catecholamine-induced apoptosis and necrosis in cardiac and skeletal myocytes of the rat in vivo: the same or separate death pathways? Exp Physiol 89:407–416
Paradis C (2008) Bias in surgical research. Ann Surg 248:180–188
Conflict of interest statement
No author has a conflict of interest in regards to the drugs or methods discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torgersen, C., Dünser, M.W., Wenzel, V. et al. Comparing two different arginine vasopressin doses in advanced vasodilatory shock: a randomized, controlled, open-label trial. Intensive Care Med 36, 57–65 (2010). https://doi.org/10.1007/s00134-009-1630-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1630-1