Abstract
Purpose
We evaluated the relations among the arterial carbon monoxide (CO) concentration, heme oxygenase (HO)-1 expression by monocytes, oxidative stress, plasma levels of cytokines and bilirubin, and the outcome of patients with severe sepsis or septic shock.
Methods
Thirty-six patients who fulfilled the criteria for severe sepsis or septic shock and 21 other patients without sepsis during their stay in the intensive care unit were studied. HO-1 protein expression by monocytes, arterial CO, oxidative stress, bilirubin, and cytokines were measured.
Results
Arterial blood CO, cytokine, and bilirubin levels, and monocyte HO-1 protein expression were higher in patients with severe sepsis/septic shock than in non-septic patients. Increased HO-1 expression was related to the arterial CO concentration and oxidative stress. There was a positive correlation between survival and increased HO-1 protein expression or a higher CO level.
Conclusions
Arterial CO and monocyte HO-1 protein expression were increased in critically ill patients, particularly those with severe sepsis or septic shock, suggesting that oxidative stress is closely related to HO-1 expression. The HO-1/CO system may play an important role in sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It was recently reported that heme oxygenase (HO)-1 acts as a potent anti-inflammatory agent and anti-oxidant through its products carbon monoxide (CO) and biliverdin [1]. Thus, HO-1 may be an inducible defense against cellular stress during the inflammatory process. It has been reported that the blood levels of carboxyhemoglobin (CO-Hb) and biliverdin are increased in critically ill patients such as those with sepsis [2, 3] or multiple trauma [4]. Although CO and CO-Hb levels have been studied in septic patients, there has been no previous examination of the correlation among HO-1 expression, levels of inflammatory cytokines, oxidative stress, and the arterial CO concentration in the septic patients.
The aims of this study were as follows: (1) to examine the differences of endogenous CO and bilirubin production and HO-1 protein expression between patients with severe sepsis/septic shock and patients without sepsis, and (2) to evaluate the relation among the blood levels of CO and bilirubin, HO-1 protein expression by monocytes, oxidative stress, and plasma levels of cytokines in these patients. We also attempted to determine the influence of the HO-1/CO system on the outcome of sepsis. We found that there was increased heme breakdown via the HO-1 pathway in patients with severe sepsis and septic shock and that inadequate induction of HO-1 may be deleterious in patients with oxidative stress.
Materials and methods
Patients
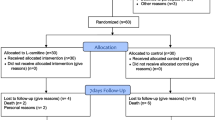
This study was conducted in conformity with the Declaration of Helsinki and was approved by the Institutional Review Board of Aichi Medical University. After receiving institutional approval and obtaining informed consent from each subject, we studied 57 consecutive critically ill patients (Table 1). Thirty-six patients were admitted to our department with severe sepsis or septic shock, or developed it during their stay in the intensive care unit (ICU). A diagnosis of severe sepsis or septic shock was made in accordance with modified criteria from the consensus statement of the 2001 Society of Critical Care Medicine, European Society of Intensive Care Medicine, American College of Chest Physicians, American Thoracic Society and Surgical Infections Society [5]. Severe sepsis was defined by the presence of the systemic inflammatory response syndrome (SIRS), known or strongly suspected infection, and hypoperfusion or fresh dysfunction of at least one vital organ. Septic shock was defined by the presence of SIRS, known or suspected infection, and the onset of shock within the previous 72 h (a systolic blood pressure of <90 mmHg despite fluid replacement or requirement for the infusion of vasopressors for at least 1 h). Patients were screened every day for SIRS and organ dysfunction until discharge from the ICU. SIRS was defined as existing if two or more of the diagnostic criteria of Bone et al. [6] were positive. Organ dysfunction was defined as described elsewhere [5]. Infection was diagnosed from clinical signs of infection and/or identification of microorganisms cultured from the suspected infectious foci. The severity of illness was assessed by calculating the Acute Physiologic and Chronic Health Evaluation (APACHE) II score [7] and the Sequential Organ Failure Assessment (SOFA) score [8].
The patients with severe sepsis or septic shock had community-acquired pneumonia (n = 6), nosocomial pneumonia (n = 14), peritonitis (n = 10), soft tissue infection (n = 2), acute pyelonephritis (n = 1), infectious endocarditis (n = 1), and post-resuscitation syndrome (n = 2). Twenty-one other patients with various conditions [acute myocardial infarction (n = 5), myocarditis (n = 1), multiple fractures (n = 5), idiopathic interstitial pneumonia (n = 3), rupture of abdominal aortic aneurysm (n = 2), acute cerebral infarction (n = 2), accidental hypothermia (n = 1), and cardiogenic pulmonary edema (n = 2)] were also studied as non-septic control patients. Some of the non-septic controls showed features of SIRS but did not demonstrate any evidence of infection during their ICU stay.
Blood samples
Blood samples were collected on the day that the criteria for severe sepsis or septic shock were met. Blood samples from the non-septic control patients were collected within 24 h after excluding the criteria for severe sepsis or septic shock. Eighteen healthy volunteers from the medical staff served as the healthy controls (eight men and ten women).
Determination of whole blood CO
CO was measured in whole blood with an automated gas chromatography CO analyzer (TRIlyzer, Taiyo Instruments, Osaka, Japan) [9]. After 100 μl of whole blood was added to a special vial, it was closed with a screw cap that incorporated a diaphragm. Then saturated potassium ferricyanide was injected through the diaphragm, and the sample was mixed. Next, 1 ml of the gas liberated from the blood sample was collected from the headspace with an airtight syringe and subjected to gas chromatographic analysis. The headspace gas was passed (with hyper-purified air) through a stainless steel column (2 m × 3 mm i.d.) packed with a 13X molecular sieve (60/80 mesh, GL Sciences Co., Tokyo, Japan) and operated at 45°C. After separation, the H2, CH4, and CO were detected by a semiconductor sensor tip connected to the electrode. The gas chromatography system was controlled, and calculation of peak areas was performed with a Dell computer using Taiyo chromatography software (Osaka, Japan) and a Uni-2 baseline adjuster (GL Sciences Co., Tokyo, Japan) that adjusted baseline drift to horizontal in real time. All measurements were corrected by the amount of CO in the blank reaction vial.
Determination of intracellular HO-1 protein expression by flow cytometry
Peripheral blood mononuclear cells (PBMCs) were isolated from heparinized fresh blood by Ficoll-Hypaque density gradient centrifugation. Washed PBMCs were resuspended at 1 × 106 cells/ml in RPMI 1640 medium (Gibco Life Technologies, Gaithersburg, MD) with 10% heat-inactivated fetal bovine serum (Hyclone Laboratories, Logan, UT) containing 2 mM glutamine. The cells were stained with an phycoerythrin/cyanin (PE) 5.1-conjugated anti-CD14 monoclonal antibody (mAb; BD Biosciences, Franklin Lakes, NJ), fixed, permeabilized, and incubated with fluorescein isothiocyanate-conjugated anti-human-HO-1 mAb (Stressgen Bioreagents, Victoria, Canada) or the isotype control (BD Biosciences) [10]. After cells were washed once with PBS, fluorescence was analyzed by a FACSCanto II flow cytometer using CellQuest software (BD Biosciences). Monocytes were acquired by gating according to their staining with PE-conjugated anti-CD14 and side-scatter properties, and then the level of intracellular HO-1 protein expression was evaluated in the monocyte population. Results are expressed as the mean fluorescence intensity (MFI) index, which was calculated as the MFI of cells stained by the specific antibody divided by the MFI of cells stained by the irrelevant isotype-matched antibody (IgG2b).
Determination of 8-hydroxy 2′-deoxyguanosine (8-OHdG) content in leukocyte DNA
Total DNA was extracted from PBMCs by the pronase/ethanol method with some modifications [11]. After hydrolyzation of the extracted DNA, nucleosides in the hydrolysate were separated on a reverse-phase high-performance liquid chromatography system (LC6A, Shimazdu, Kyoto, Japan) equipped with a C18 column (4.6 × 250 mm; Wako, Tokyo, Japan) and eluted at a flow rate of 1 ml/min by using a mobile phase of 8% methanol in 50 mmol/l potassium phosphate buffer (pH 5.5). The amount of 8-OHdG was determined by an electrochemical detector (Shimadzu, Kyoto, Japan). Deoxyguanosine (dG) and 8-OHdG were used as standards. The 8-OHdG level was expressed as the number of 8-OHdG molecules per 106 dG molecules.
Other parameters
Plasma concentrations of cytokines were determined by enzyme-linked immunosorbent assay (ELISA) kits from BioSource International (Camarillo, CA) for interleukin-8 (IL-8), IL-6, and IL-1β and from Sino Test Corporation (Sagamihara, Kanagawa, Japan) for high-mobility group box 1 (HMGB1). The detection limits of these kits were 0.7, 3, 2 pg/ml, and 1 ng/ml for IL-8, IL-6, IL-1β, and HMGB1, respectively. The plasma bilirubin level was measured by a conventional autoanalyzer. The antioxidant status was assessed by measuring the reduction of ferric ions by plasma (BAP test) using an automated tester (Diacron International, Grosseto, Italy). BAP test results were expressed as μmol/l of reduced ferric ions [12].
Statistics
Results are expressed as medians with the interquartile range. Comparison between groups was performed with the Mann–Whitney rank sum test. Mortality rates were compared between groups by the chi-square test. Correlations between variables were assessed by calculating Pearson’s product moment correlation coefficients. A probability (P) value <0.05 was considered statistically significant. Calculations were done with SigmaStat software (version 3.5; Systat Software Inc., Point Richmond, CA).
Results
ICU admission characteristics
Both groups of patients were predominantly male (Table 1). There were no significant differences between the severe sepsis/septic shock ICU group and the non-septic ICU group with respect to gender (P = 0.33), age (P = 0.41), duration of ventilation (P = 0.14), and ICU stay (P = 0.32). However, the patients with severe sepsis/septic shock differed from the non-septic patients in terms of their SOFA scores, APACHE II score, and mortality rate. All of the patients with severe sepsis/septic shock required inotropic support and mechanical ventilation. Gram-positive bacteria were cultured in 10 patients, gram-negative bacteria in 12, and mixed infections in 4. In ten of these patients, blood cultures were also positive. All of the patients with severe sepsis/septic shock had organ failure according to the criteria of Levy et al. [5], and 21 had failure of two or more organs. In contrast, some of non-septic ICU patients showed signs of SIRS, but did not have any evidence of infection or infection-induced organ failure.
HO-1, CO, cytokines, bilirubin, and oxidative stress
Expression of HO-1 protein by monocytes was increased in both groups of ICU patients, although the level of HO-1 protein expression was higher in the patients with severe sepsis/septic shock than in the non-septic patients (Table 2). The CO concentrations of whole blood, as well as the plasma levels of HMGB1, IL-6, IL-1, IL-8, and bilirubin, were significantly higher in the patients with severe sepsis/septic shock than in the non-septic patients (Table 2). CO and cytokine levels were significantly higher in the non-septic patients than in the healthy volunteers. The leukocyte level of 8-OHdG was also significantly higher in the patients with severe sepsis/septic shock than in the non-septic patients, while the plasma antioxidant capacity of patients with severe sepsis/septic shock was significantly lower than that of non-septic patients (Table 2). In contrast, the 8-OHdG level and plasma antioxidant capacity of the non-septic patients were not significantly different from those of the healthy volunteers.
Relations among the variables
As shown in Fig. 1, the extent of HO-1 expression by monocytes was correlated with the plasma levels of CO (Fig. 1a) and 8-OHdG (Fig. 1b). In addition, a negative correlation was observed between HO-1 expression and plasma antioxidant capacity (Fig. 1c). However, there was no correlation between HO-1 expression and the plasma level of IL-6 (Figs. 1d), as well as no correlation between HO-1 expression and the plasma level of IL-10 or IL-1β (data not shown). There was no correlation between plasma bilirubin and HO-1 expression (r = 0.079, P = 0.62), the plasma level of CO (r = 0.037, P = 0.24), or serum antioxidant capacity (r = −0.038, P = 0.81).
Correlation between HO-1 expression by monocytes and the plasma level of CO (a), the 8-hydroxy 2′-deoxyguanosine level in leukocytes (b), plasma antioxidant capacity (c), and plasma IL-6 (d). The solid line running through the points represents the regression line, and the broken line represents the confidence interval. Correlations were assessed by Pearson’s product moment correlation analysis
Relations of variables to the outcome
The patients with severe sepsis/septic shock who died had a significantly higher APACHE II score and SOFA score than those who survived (Table 3). The blood CO level and monocyte HO-1 expression were significantly lower in patients with severe sepsis/septic shock who died than in those who survived (Table 3).
Discussion
This study showed that the plasma CO concentration was significantly higher in patients with severe sepsis/septic shock than in non-septic patients and that plasma CO was well correlated with HO-1 expression by monocytes. It has been reported that at least 86% of endogenous CO production results from the degradation of heme, a process that depends on HO-1, the rate-limiting enzyme of heme catabolism [13]. Thus, the elevation of blood CO and the increase of monocyte HO-1 protein expression observed in this study strongly suggested an increase of heme catabolism in septic patients. Morimatsu et al. [14] reported that arterial CO-Hb, exhaled CO, and serum total biliverdin were all significantly higher in critically ill patients compared with controls, and suggested that these three major products of heme catabolism could be novel and useful markers for the severity of critical illness. However, our results showed that serum total bilirubin was not correlated with the CO level or with HO-1 protein expression. The serum bilirubin level is determined by the balance between its synthesis and clearance. Hyperbilirubinemia in patients with sepsis and SIRS presumably results from dysfunction of bilirubin transport and clearance [15], in addition to heme catabolism. Moreover, increased production of heme due to intravascular hemolysis, giant hematoma, and massive blood transfusion may have a marked influence on bilirubin synthesis. Accordingly, our results indicate that serum bilirubin is less useful than CO as a marker of heme catabolism.
Several lines of evidence have indicated that HO-1 expression is part of an adaptive response to injury and inflammation. Yachie et al. [16] reported that monocytes from patients with acute inflammatory illnesses, such as Kawasaki disease and acute infections, had high levels of HO-1 protein and mRNA. Such upregulation of HO-1 in septic patients is consistent with our results. Although HO-1 mRNA expression and enzyme activity were not measured in this study, HO-1 protein expression is primarily regulated at the transcriptional level, so there should be no major difference between protein and gene expression [17]. In addition, due to the abundance of endogenous hemoproteins, enzyme activity is not limited by lack of substrates [17].
HO-1 is not only induced by its substrate heme, but also by inflammatory cytokines and oxidative stress [13]. There is evidence that HO-1 is most commonly induced by agents and conditions that are associated with oxidative stress [13, 18]. In an animal model of sepsis created by cecal ligation and puncture, both leukocyte expression of HO-1 mRNA and plasma lipid peroxidation levels were significantly elevated after only 3 h, suggesting that more severe oxidative stress may trigger early HO-1 mRNA expression by leukocytes [18]. In the present study, we observed that oxidative stress (as detected from the leukocytes 8-OHdG level and the decrease of plasma antioxidant capacity) was correlated with HO-1 protein expression by monocytes. Most authors believe that high levels of oxyradicals and low antioxidant levels in patients with SIRS or septic shock promote oxidative damage to cells/tissues [19]. However, some investigators have shown that the serum antioxidant capacity is increased in severe sepsis due to an increase of serum bilirubin [20]. The increase of total bilirubin and the decrease of total antioxidant capacity observed in patients with severe sepsis/septic shock patients in this study were not fully consistent with previously published data. This discrepancy could be explained by the use of different methods for assessing total antioxidant capacity. Antioxidants in plasma may react to a differing extent with a given source of free radicals, so results may vary depending on the method of evaluation.
High levels of cytokines (such as HMGB1, IL-6, IL-1β, and IL-8) are found in patients with severe sepsis or septic shock, suggesting a possible role of cytokines in influencing the expression of HO-1. However, HO-1 protein expression was not correlated with plasma levels of inflammatory cytokines in the present study. Despite this, we cannot rule out a potential influence of cytokines on HO-1 expression, because only single-point blood collection was performed, and plasma cytokine kinetics could have varied rapidly before any change of HO-1 expression.
The upregulation of HO-1 is associated with less severe damage after exposure of various organs to polymicrobial sepsis [18] and endotoxemia [21], since the products of catabolism by HO-1, including CO, biliverdin, and bilirubin, have anti-inflammatory and antioxidant properties. Interestingly, the septic survivors showed a higher CO level than the septic non-survivors in the present study, suggesting that a fatal outcome of severe sepsis/septic shock may be related to limited production of CO or poor induction of HO-1. In a large group of patients who entered the ICU after cardiothoracic surgery, Melley et al. [22] showed that both low minimum and high maximum arterial CO-Hb levels were associated with increased mortality, and concluded that HO-1 is neither exclusively cytoprotective nor exclusively cytotoxic. It has been reported that the beneficial effect of HO-1 overexpression in HO-1-transfected cells is likely to be limited to a rather narrow window of expression, possibly due to the liberation of molecular iron by HO-1 [13]. The present study did not assess iron levels, so whether increased release/deposition of toxic free iron ions results from excess induction of the HO-1 gene in vivo (as has been suggested in cultured cells [23]) needs to be studied in the future.
In conclusion, we found that the increase of endogenous CO production in severe sepsis/septic shock mainly reflects increased heme turnover secondary to upregulation of HO-1, which partially occurs in response to systemic oxidative stress. A strong correlation between the blood CO level and survival supports the beneficial effect of HO-1 upregulation and increased CO production in patients with severe sepsis/septic shock.
References
Scott JR, Chin BY, Bilban MH, Otterbein LE (2007) Restoring HOmeostasis: is heme oxygenase-1 ready for the clinic? Trends Pharmacol Sci 28:200–205
Hoetzel A, Dolinay T, Schmidt R, Choi AMK, Ryter SW (2007) Carbon monoxide in sepsis. Antioxid Redox Signal 9:2013–2026
Zegdi R, Perrin D, Burdin M, Boiteau R, Tenaillon A (2002) Increased endogenous carbon monoxide production in severe sepsis. Intensive Care Med 28:793–796
Moncure M, Brathwaite CE, Samaha EMA, Marburger RRN, Ross SE (1999) Carboxyhemoglobin elevation in trauma victims. J Trauma 46:424–427
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31:1250–1256
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Ohta K, Terai H, Kimura I, Tanaka K (1999) Simultaneous determination of hydrogen, methane, and carbon monoxide in water by gas chromatography with a semiconductor detector. Anal Chem 71:2697–2699
Bachelet M, Mariethoz E, Banzet N, Souil E, Pinot F, Polla CZ, Durand P, Bouchaert I, Polla BS (1998) Flow cytometry is a rapid and reliable method for evaluating heat shock protein 70 expression in human monocytes. Cell Stress Chaperones 3:168–176
Tarng DC, Huang TP, Liu TY, Chen HW, Sung YJ, Wei YH (2000) Effect of vitamin E-bonded membrane on the 8-hydroxy 2′-deoxyguanosine level in leukocyte DNA of hemodialysis patients. Kidney Int 58:790–799
Pasquini A, Luchetti E, Marchetti V, Cardini G, Iorio EL (2008) Analytical performances of d-ROMs test and BAP test in canine plasma. Definition of the normal range in healthy Labrador dogs. Vet Res Commun 32:137–143
Bauer M, Huse K, Settmacher U, Claus RA (2008) The heme oxygenase-carbon monoxide system: regulation and role in stress response and organ failure. Intensive Care Med 34:640–648
Morimatsu H, Takahashi T, Maeshima K, Inoue K, Kawakami T, Shimizu H, Takeuchi M, Yokoyama M, Kaytayama H, Morita K (2006) Increased heme catabolism in critically ill patients: correlation among exhaled carbon monoxide, arterial carboxyhemoglobin, and serum bilirubin. Am J Physiol 290:L114–L119
Banks JG, Foulis AK, Ledingham IM, Macsween RN (1982) Liver function in septic shock. J Clin Pathol 35:1249–1252
Yachie A, Toma T, Mizuno K, Okamoto H, Shimura S, Ohta K, Kasahara Y, Koizumi S (2003) Heme-oxygenase-1 production by peripheral blood monocytes during acute inflammatory illnesses of children. Exp Biol Med 228:550–556
Maines MD (1997) The heme oxygenase system: a regulator of second messenger gases. Annu Rev Pharmacol Toxicol 37:517–554
Jao HC, Lin YT, Tsai LY, Wang CC, Liu HW, Hsu C (2005) Early expression of heme oxygenase-1 in leukocytes correlates negatively with oxidative stress and predicts hepatic and renal dysfunction at late stage of sepsis. Shock 23:464–469
Motoyama T, Okamoto K, Kukita I, Hamaguchi M, Kinoshita Y, Ogawa H (2003) Possible role of increased oxidant stress in multiple organ failure after systemic inflammatory response syndrome. Crit Care Med 31:1048–1052
Pascual C, Karzai W, Meir-Hellmann A, Oberhoffer M, Horn A, Bredle D, Reinhart K (1998) Total plasma antioxidant capacity is not always decreased in sepsis. Crit Care Med 26:705–709
Tamion F, Richard V, Renet S, Thuillez C (2006) Protective effects of heme-oxygenase expression against endotoxic shock: inhibition of tumor necrosis factor-α and augmentation of interleukin-10. J Trauma 61:1078–1084
Melley DD, Finney SJ, Elia A, Lagan AL, Quinlan GJ, Evans TW (2007) Arterial carboxyhemoglobin level and outcome in critically ill patients. Crit Care Med 35:1882–1887
Suttner DM, Dennery PA (1999) Reversal of HO-1 related cytoprotection with increased expression is due to reactive iron. FASEB J 13:1800–1809
Acknowledgments
This study was supported by the Japan Society for the Promotion of Science [Grant-in-Aid for Scientific Research (C) no. 18591991].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takaki, S., Takeyama, N., Kajita, Y. et al. Beneficial effects of the heme oxygenase-1/carbon monoxide system in patients with severe sepsis/septic shock. Intensive Care Med 36, 42–48 (2010). https://doi.org/10.1007/s00134-009-1575-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1575-4