Abstract
Objective
Sublingual microvascular videomicroscopy can assess tissue perfusion in critically ill patients; however, data analysis is currently limited to delayed off-line evaluation. We hypothesized that a real-time point-of-care (POC) determination of the microcirculatory flow index (MFI), an established metric for assessing microcirculatory perfusion, agrees well with the conventional off-line analysis.
Design
Prospective observational study.
Setting
Urban academic intensive care unit.
Participants
A heterogeneous population of critically ill patients.
Measurements and results
A single operator performed side stream darkfield videomicroscopy of the sublingual microcirculation and made a POC determination of MFI in real-time on a portable bedside monitor by assigning a score (0 = no flow to 3 = normal) to each quadrant of the image and averaging the four values. After image processing, de-identification and randomization, the same operator, blinded to the previous interpretation, repeated the MFI assessment by viewing an AVI-formatted image sequence on a 94 cm 1,080 pixel LCD monitor (reference standard). There were 205 paired measurements in 18 subjects. The POC and reference standard MFI had good agreement by Bland–Altman analysis [mean difference of −0.031, SD = 0.198 (95% CI, −0.43 to 0.37)]. The POC assessment was 94% sensitive and 92% specific for detecting impaired microvascular flow (defined a priori as an MFI < 2.5 based on previously published data).
Conclusions
A POC determination of MFI had good agreement with conventional off-line analysis, and was highly sensitive and specific for detecting impaired microvascular flow. This real-time technique may be useful in future clinical trials targeting impaired microcirculatory perfusion in critically ill patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Assessment of tissue perfusion is important in critically ill patients. Although the macrocirculation, comprised of the heart and large arteries, distributes blood flow globally throughout the body, it is the microcirculation, the integrated network of arterioles, capillaries and venules, that delivers blood flow to tissues and is the principal site of tissue oxygen transport. Thus, an intact and functional microcirculation is a critical element of the cardiovascular system vital for effective tissue oxygen delivery.
Microcirculatory dysfunction is a key factor in the pathophysiology of a variety of systemic pro-inflammatory states and shock etiologies including septic shock, cardiogenic shock, and ischemia/reperfusion injury [1–4]. New techniques for videomicroscopy of the vascular networks beneath mucosal surfaces have enabled minimally invasive microcirculatory assessment in critically ill patients. One accepted method of quantifying microvascular flow of vessels <20 μm in diameter is the semi-quantitative microcirculatory flow index (MFI) [5, 6]. Clinical studies have shown that MFI measured early in the course of disease can be prognostic in critically ill patients [1, 2, 4, 7, 8] and therefore can yield potentially important information during acute care and resuscitation.
Currently, conventional image analysis techniques for assessment of microcirculatory flow use off-line image processing and delayed evaluation of the image sequences in a laboratory setting. However, real-time assessment of microcirculatory flow at the bedside would be necessary for timely application of clinical interventions targeting improvement in microcirculatory perfusion. No validation studies of a real-time analysis technique for measuring microcirculatory flow at the bedside have yet been reported. This study tested the hypothesis that real-time point-of-care (POC) determination of MFI at the bedside has good agreement with conventional off-line analysis techniques in a heterogeneous patient population across a wide range of flow characteristics.
Materials and methods
This was a prospective observational study within the intensive care unit (ICU) of an urban academic medical center. We obtained 205 paired measurements (POC and reference standard) of MFI obtained and analyzed by a single operator (RCA) in a heterogeneous population of critically ill patients in various stages of disease severity. This investigation was a sub-study of two separate ongoing investigations assessing microcirculatory perfusion [8, 9]. Inclusion criteria were (1) age ≥ 18, (2) admission to the ICU, and (3) co-enrollment in one of the two study protocols at our institution that employs microcirculatory videomicroscopy in the study of circulatory shock (post-cardiac surgery utilizing cardiopulmonary bypass [9] or severe sepsis [8]).
Image acquisition
Subjects were imaged within 3 h of arrival to the ICU at multiple time intervals mandated by the co-enrollment protocols [8, 9]. A single operator performed all of the sublingual imaging with a sidestream dark field (SDF) videomicroscope (Microscan, Microvision Medical, Amsterdam), using acquisition techniques previously described and validated in both animal models and human studies [10–13]. SDF imaging produces a magnified, real-time video sequence of blood flow through submucosal microvascular networks (326× onscreen magnification) through the emission of light within the absorption frequency of hemoglobin (wavelength of 530 nm) producing an image in which red blood cells appear dark against a light background (see the Electronic Supplemental Material). At each imaging time point, video sequences were obtained from three to five separate sublingual sites in 20-s segments.
Image analysis
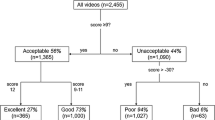
Flow characteristics of the microvasculature were quantified using the MFI, a semi-quantitative technique originally described by Boerma et al. [5] and consistent with recommendations from the recently published consensus conference on microcirculatory image analysis in human subjects [6]. The image is divided into 4 quadrants and the vessels <20 μm diameter are assigned a score based on the predominant flow characteristics of the vessels in that quadrant (0 = absent flow; 1 = intermittent; 2 = sluggish; 3 = normal). The values in each quadrant are averaged to give an MFI for each sublingual site at each time point. We have used this method in previous investigations and shown good inter-rater agreement among multiple observers (κ = 0.87) [8]. The bedside POC determination of the MFI (POC-MFI) was performed through real-time microcirculatory image assessment at the bedside without image processing as viewed on a 33 cm analog monitor attached to a portable stand. Using the technique described above for MFI assessment, the images were scored during acquisition by the operator at each sublingual site. The images obtained at the bedside were recorded onto digital tape (DVCAM Recorder, Sony DSR-11, USA). Video sequences from each sublingual site were processed and transferred into AVI format and digitally stored by code (1–10,000) without patient identifiers. Images were assigned a random number to enable offline analysis blinded to all clinical data and POC-MFI value. Off-line assessment of MFI served as the reference standard for this study. Each processed video sequence was viewed on a 94 cm LCD monitor with 1,080 pixel resolution in a laboratory. The processed images were scored with the investigator blinded to the POC-MFI value.
Statistical analysis
The agreement between POC-MFI and the reference standard MFI was tested using the Bland–Altman method [14], which plots the mean of the paired measurements (x-axis) against the difference between each measurement (y-axis). We also tested the ability of the POC-MFI to detect impaired microcirculatory flow. A priori, we defined impaired microcirculatory flow as an MFI < 2.5 based on MFI averages for control subjects previously reported by our group (2.66–3.0) [4].
The sensitivity, specificity and likelihood ratio of the POC-MFI assessment’s ability to detect impaired microvascular flow were calculated using the off-line MFI as the reference standard. All analyses were carried out using SPSS 14.0 software (SPSS Inc, Chicago, Illinois). The sample size estimate for a Bland–Altman method is based on 95% confidence intervals around the standard deviation (SD) of the difference between the two measurements. We calculated that a minimum sample size of 130 paired measurements would give an acceptably low variance (95% CI ± 0.30 SD) [14, 15], and thus we enrolled consecutive subjects imaged by a single operator until a minimum of 130 paired measurements were accrued. After obtaining 150 measurements, interim analysis revealed the consecutive enrollment resulted in a majority of CABG patients; enrollment then continued targeting only sepsis patients until equivalent numbers were obtained.
Results
We performed 205 paired measurements in 18 subjects (Table 1). Vasopressor medications were used at the time of imaging in 65/205 (32%) of the paired measurements, vasodilators alone in 20/205 (10%), vasodilators, vasopressors, and inotropes in 15/205 (7%), and no vasoactive medications in 105/205 (51%). The reference standard (offline) MFI values ranged from 1.25 to 3.00. When compared using the Bland–Altman method, the POC-MFI demonstrated good agreement with the reference standard. The mean difference between the two tests was −0.031, SD = 0.198 [95% CI, −0.43 to 0.37] (Fig. 1). The Bland–Altman method defines the upper limits of agreement as 2 SDs from the mean (±0.396). When comparing MFI values, 94% of the POC-MFI measurements in this study were ±0.25 from the offline MFI, the smallest measurable increment of disagreement (see the Electronic Supplemental Material).
Bland–Altman plot of the comparison between conventional offline and the bedside point-of-care (POC) determinations of microcirculatory flow index (MFI). This graph describes the level of agreement between different methods of measurement. The solid line shows the mean deviation (bias) between POC-MFI and reference standard (offline) MFI (−0.031); the dashed line represents the limits of agreement (mean ± 2 SD) with SD = 0.198
To control for repeated measures in a data set with an unequal number of replicates, as per Bland and Altman [16], we first checked with the assumption that the within-subject variances for each method were independent of the subjects’ mean MFI (see the Electronic Supplemental Material) showing good agreement (perfect agreement = MFI difference of zero) regardless of mean MFI. We then verified this independence with a modified Bland–Altman plot displaying only mean MFI for each subject in the study (Fig. 2) and reported the 95% limits of agreement using the SD of the means and separate limits adjusted for the within-subject variance (SDv).
Bland–Altman plot of the mean differences between conventional offline and point-of-care (POC) determinations of microcirculatory flow index (MFI) for each subject (n = 18). The solid line shows the mean deviation (bias) between mean POC-MFI and reference standard (offline) MFI (−0.033); the dashed lines represent the limits of agreement (mean ± 2SD) of the means with SD = 0.072. The dotted lines represent the 95% limits of agreement adjusted for the within-subject variance of the differences (SDv) between observations by the two methods
Impaired microcirculatory flow (MFI < 2.5) occurred in 120/205 (59%) images by the reference standard. The POC assessment was 94% sensitive (95% CI: 91–97%) and 92% specific for detecting an MFI < 2.5 (95% CI: 87–95%). The overall diagnostic accuracy of the POC assessment was 93% (Table 2). The positive (+) likelihood ratio for impaired microcirculatory flow with a POC-MFI < 2.5 was 11.4 (95% CI: 6.7–19.5). The negative (−) likelihood ratio for impaired microcirculatory flow with a POC-MFI < 2.5 was 0.06 (95% CI: 0.04–0.11). Additionally, the directional change in the average MFI between time points within an individual patient (∆MFI) as measured by the reference standard was accurately tracked by the POC assessment (see the Electronic Supplemental Material). While the data set includes repeated imaging separated by time in each patient, the operator characteristics for the POC measurement were performed as if each observation were independent of the others.
Discussion
Microcirculatory dysfunction is an important pathophysiologic mechanism in critically ill patients. Observational studies have reported that sublingual microcirculatory blood flow indices are prognostic in patients with overt or impending shock, and these indices may yield distinct physiologic information that macrocirculatory parameters cannot [1, 2, 4, 7]. As this line of research evolves from observational studies to interventional trials, microcirculatory flow indices are transforming from markers of disease severity to therapeutic targets [17–19]. Currently, microcirculatory image analysis requires offline processing and scoring, delaying results to the treating clinician, and precluding guidance in clinical decisions. There is a need for a bedside real-time assessment of the microcirculation to enable the timely application of novel therapeutics and resuscitative strategies targeting an improvement in microcirculatory perfusion [19].
In the present study, we aimed to validate a real-time POC measurement of MFI at the bedside as compared to the conventional technique of measuring MFI off-line in a laboratory. We found that real-time POC determination of MFI had good agreement with conventional analysis, and was highly sensitive and specific for detecting impaired microvascular flow. We conclude that the wide range of MFI values in this sample supports the use of the POC-MFI measurement over a wide spectrum of microcirculatory perfusion characteristics. Specifically, the clustering of the points around the mean is greatest at low MFI values (MFI ≤ 2.0) in Figure 1. This supports the conclusion that the POC-MFI technique may prove useful in clinical trials of therapies targeting impaired microcirculatory perfusion in critically ill patients until a more accurate computer-assisted microvascular flow scoring technique is available.
We acknowledge important limitations. First, we examined only the POC method for determining MFI, and did not attempt to validate a real-time determination of perfused vessel density (PVD) [6]. Conventional techniques to assess PVD require a multi-step offline process that may not be as readily translated to the bedside for a rapid POC measurement; and failure to capture PVD could potentially omit important information on the status of the microcirculation [6]. Second, an operator experienced in SDF acquisition obtained the MFI measurements in both the POC and reference standard and these results may be applicable only to similarly experienced operators. Also, the resolution of the bedside monitor was not the same as that of the offline LCD monitor and may have contributed to some of the difference in scoring methods. Third, the analysis to control for within-subject variance widened the 95% confidence intervals for the limits of agreement. While the subject means demonstrated good agreement with a small SD (Fig. 2), there was an increase in the limits of agreement when adjusted for repeated measures (SDv). We felt this increase was partially due to the use of the total variance of each method in the calculation, an expectedly high number in our patient population with a dynamic change in disease severity and wide range of MFI (1.25–3.00).
Conclusion
A POC determination of MFI had good agreement with conventional off-line analysis, and was highly sensitive and specific for detecting impaired microvascular flow. As the microcirculation emerges as a viable resuscitation target for new therapeutic strategies in critically ill patients, this bedside technique can be used to generate real-time data on the status of microvascular perfusion.
References
De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL (2004) Microvascular alterations in patients with acute severe heart failure and cardiogenic shock. Am Heart J 147:91–99
De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL (2002) Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med 166:98–104
Fox-Robichaud A, Payne D, Hasan SU, Ostrovsky L, Fairhead T, Reinhardt P, Kubes P (1998) Inhaled NO as a viable antiadhesive therapy for ischemia/reperfusion injury of distal microvascular beds. J Clin Invest 101:2497–2505
Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM (2007) Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med 49:88–98
Boerma EC, Mathura KR, van der Voort PH, Spronk PE, Ince C (2005) Quantifying bedside-derived imaging of microcirculatory abnormalities in septic patients: a prospective validation study. Crit Care 9:R601–R606
De Backer D, Hollenberg S, Boerma C, Goedhart P, Buchele G, Ospina-Tascon G, Dobbe I, Ince C (2007) How to evaluate the microcirculation: report of a round table conference. Crit Care 11:R101
Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL (2004) Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med 32:1825–1831
Trzeciak S, McCoy JV, Phillip Dellinger R, Arnold RC, Rizzuto M, Abate NL, Shapiro NI, Parrillo JE, Hollenberg SM (2008) Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med 34:2210–2217
Arnold RC, Parrillo JE, Trzeciak S, McCoy J, Hollenberg SM, Dellinger RP (2007) Impact of cardiopulmonary bypass on microcirculatory perfusion: a pilot study (abstract). Inflamm Res 56:S217
Groner W, Winkelman JW, Harris AG, Ince C, Bouma GJ, Messmer K, Nadeau RG (1999) Orthogonal polarization spectral imaging: a new method for study of the microcirculation. Nat Med 5:1209–1212
Harris AG, Sinitsina I, Messmer K (2000) The Cytoscan Model E-II, a new reflectance microscope for intravital microscopy: comparison with the standard fluorescence method. J Vasc Res 37:469–476
Mathura KR, Vollebregt KC, Boer K, De Graaff JC, Ubbink DT, Ince C (2001) Comparison of OPS imaging and conventional capillary microscopy to study the human microcirculation. J Appl Physiol 91:74–78
Dubin A, Edul VS, Pozo MO, Murias G, Canullan CM, Martins EF, Ferrara G, Canales HS, Laporte M, Estenssoro E, Ince C (2008) Persistent villi hypoperfusion explains intramucosal acidosis in sheep endotoxemia. Crit Care Med 36:535–542
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Bland JM (2008) How can I decide the sample size for a study of agreement between two methods of measurement? http://www-usersyorkacuk/~mb55/meas/sizemethhtm
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant C, Vincent JL (2006) The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med 34:403–408
De Backer D, Verdant C, Chierego M, Koch M, Gullo A, Vincent JL (2006) Effects of drotrecogin alfa activated on microcirculatory alterations in patients with severe sepsis. Crit Care Med 34:1918–1924
Trzeciak S, Cinel I, Phillip Dellinger R, Shapiro NI, Arnold RC, Parrillo JE, Hollenberg SM (2008) Resuscitating the microcirculation in sepsis: the central role of nitric oxide, emerging concepts for novel therapies, and challenges for clinical trials. Acad Emerg Med 15:399–413
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Acknowledgments
This study was supported in part by a Resident Research Grant from the Emergency Medicine Foundation to Dr. Arnold. Dr. Trzeciak’s effort to this project was supported by a grant from the National Institutes of Health/National Institutes of General Medical Sciences (K23GM83211).
Conflict of interest statement
None of the authors have financial conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Microcirculatory Alterations in Resuscitation and Shock (MARS) Investigators.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Arnold, R.C., Parrillo, J.E., Phillip Dellinger, R. et al. Point-of-care assessment of microvascular blood flow in critically ill patients. Intensive Care Med 35, 1761–1766 (2009). https://doi.org/10.1007/s00134-009-1517-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1517-1