Abstract
Objective
The approach to acute cognitive dysfunction varies among physicians, including intensivists. Physicians may differ in their labeling of cognitive abnormalities in critically ill patients. We aimed to survey: (a) what Canadian intensive care unit (ICU) physicians identify as “delirium”; (b) choices of non-pharmacological and pharmacological management; and (c) consultation patterns among ICU patients with cognitive abnormalities.
Design
A mail-in self-administered survey was sent to Canadian intensivists registered with the Canadian Critical Care Society. The survey contained three clinical scenarios which described cognitively abnormal patients with: (a) hepatic encephalopathy; (b) multiple drug overdose; and (c) post-operative aortic aneurysm repair. Symptoms, which included fluctuating level of consciousness, inattention, disorientation, hallucinations, sleep/wake cycle disturbance, and paranoia, all fulfilled DSM-IV criteria for delirium. We asked for diagnoses in short-answer format for each scenario, and offered multiple selections of non-pharmacological and pharmacological therapies and consultation options.
Participants
All intensivists registered with the Canadian Critical Care Society.
Measurements and results
One-hundred thirty surveys were returned, for a response rate of 58.3%. When an etiological cognitive dysfunction diagnosis was obvious, 83–85% responded with the medical diagnosis to explain the cognitive abnormalities; only 43–55% used the term “delirium”. In contrast, where an underlying medical problem was lacking, 74% of respondents diagnosed “delirium” (p = 0.002). Non-pharmacological and pharmacological management varied considerably by physician and scenario but independently from whether the term “delirium” was selected. Commonly selected pharmacological agents were antipsychotics and benzodiazepines, followed by narcotics, non-narcotic analgesics, and other sedatives. Whether and when intensivists chose to consult other services varied.
Conclusions
Canadian intensivists diagnose delirium based upon the presence or absence of an obvious medical etiology. Wide variation exists in approach to management, as well as patterns of consultation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Delirium is common in clinical practice and in the intensive care unit (ICU). Prevalence ranges from 19 to 87%, depending on the study [1–4]. The development of ICU delirium is increasingly recognized as an independent predictor of morbidity and mortality [3, 5, 6]; however, as published reports increase our understanding of the topic, several gaps and inconsistencies become apparent. How do intensivists diagnose delirium? Does diagnosis affect management? How is the disorder most appropriately managed in the ICU setting?
In particular, we are unaware of any literature that examines how delirium is diagnosed in the ICU. In general, delirium is perceived to be under-diagnosed, and only a minority of practitioners use validated screening tools [7]. Identifying how ICU physicians diagnose cognitive abnormalities in patients would be a critical first step in clarifying which patients are identified as delirious, which patients are treated, and help inform outcomes.
There is also a dearth of information in the literature about how to treat ICU delirium. Even physicians with expertise in caring for elderly patients vary considerably in their approach to the clinical management of delirium with respect to diagnostic testing and use of pharmacological therapy [8]. Clinically, these differences are important to understand, as pharmacological interventions are not benign. Frequently used anxiolytics and major tranquilizers can be harmful [9, 10] and excessive sedative use in the ICU prolongs mechanical ventilation and hospital stay [11].
We therefore designed this study to investigate what Canadian ICU physicians call cognitive and perceptual abnormalities in ICU patients, using a scenario-based, self-administered questionnaire. We hypothesized that there would be a large variation in the labeling and management of this clinical syndrome among ICU physicians. Additionally, we asked how intensivists would manage these patients (both pharmacologically and non-pharmacologically), and whether intensivists would seek expert consultation (e. g., from psychiatrists, geriatricians, neurologists, or others), as there are no published data on consultation and referral patterns in the ICU for this condition.
Methods
Survey design and administration
We designed a mail-in self-administered survey featuring three hypothetical case vignettes. These vignettes were written by an expert panel consisting of a geriatrician, an intensivist, and a psychiatrist. They were then independently reviewed by a critical care surgeon, a critical care anesthesiologist, and finally by the Executive Committee of the Canadian Critical Care Trials Group (CCCTG). Non-pharmacological strategies were selected by the expert panel to reflect commonly recommended strategies for older patients with delirium [12, 13]. Specific drug choices were provided based on therapeutic practices in three Canadian ICUs (in Kingston, Montreal, and Vancouver). Face and content validity of these drug choices was determined by discussions with attending physicians in two of those ICUs. Revisions from the CCCTG meeting were incorporated into the questionnaire. The final survey was mailed to the physician membership of the Canadian Critical Care Society. A second mailing was sent several weeks later. Ethics approval was received from the University Health Network.
Each patient in the case scenarios had cognitive abnormalities, including fluctuating levels of consciousness, inattention, disorientation, hallucinations, sleep/wake cycle disturbance and paranoia, thus fulfilling DSM-IV criteria for delirium. Two of the three vignettes were written so that there was a clear underlying etiological precipitant to the cognitive impairment (hepatic encephalopathy and multiple drug overdose). The third scenario was written without an obvious underlying precipitant (cognitive abnormalities after major vascular surgery; see Appendix A).
To determine how physicians labeled cognitive and perceptual changes in these patients, respondents were asked to list the most likely diagnoses to explain the patient's symptoms, in an open-ended question. The respondents were then asked to indicate, on a five-point Likert scale (strongly agree, agree, neutral, disagree, strongly disagree, do not know), whether they would use specific non-pharmacological strategies for the patient based on their own practice environment. Respondents were then asked to indicate which pharmacological treatments, if any, would be appropriate for the patient within the next 24 h. Respondents were also given the option of adding other medications. Finally, respondents were asked if they would consult other medical or psychiatric services to help manage the patient's cognitive symptoms.
Statistical analysis
Responses to individual items on the questionnaire were summarized as counts and percentages. To simplify the statistical analysis, the Likert scale was later dichotomized as any agreement vs. neutrality or disagreement. Logistic regression was used to assess the relationships between a respondent's use of “delirium” as a diagnostic label, the respondents' demographic variables, and whether these factors affected their management techniques. Ordinal logistic regression was used to assess the relationship between the threshold at which the respondent would seek consultation (with current symptoms, with worsening symptoms, never) and whether a respondent used “delirium” as a diagnostic label. Comparisons between the three different scenarios on subjects' responses (management techniques and use of “delirium” as a diagnostic label) had to take into account the potential correlation between these responses; a generalized estimating equation (GEE) approach with logistic regression was used for these comparisons between scenarios. In the GEE models, the outcome was the dichotomous variable for agreement and the predictor was the categorical variable representing scenario; respondent was the clustering variable and an unstructured correlation matrix was used. Chi-square tests were used to assess independence between variables not listed above. Statistical software used was S-Plus Professional (version 6.2, Insightful Corporation, Seattle, WA).
Results
Survey mailing and respondent characteristics
A total of 223 surveys were sent, and 130 completed surveys were returned. The response rate was 58.3%. The characteristics of the respondents are detailed in Table 1.
Diagnosis of cognitive abnormalities
Table 2 shows the number of respondents that responded with an etiological diagnosis for each of the scenarios, the number that responded with the term “delirium,” the number that listed both “delirium” and an etiological diagnosis, and the number that listed neither. When an etiology was obvious in the scenario, 83–85% of respondents responded with the medical diagnosis to explain the cognitive abnormalities, and only 43–55% used the term “delirium”. In contrast, where an underlying medical problem was lacking, 74% diagnosed “delirium” (p = 0.002). Those respondents that listed “ICU psychosis/syndrome” were categorized with those that listed “delirium,” as researchers have successfully argued that in common use, the term does not differ from delirium [14].
Use of non-pharmacological interventions
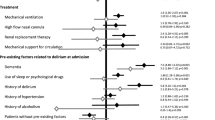
Figure 1 shows the percentage of respondents that agreed or strongly agreed with the various therapies. A similar pattern emerges in the use of three particular interventions – the use of eyeglasses, Posey jacket restraint, and wrist restraints. The GEE models show that respondents tended to choose the use of these interventions in the elderly cirrhotic and the elderly post-operative confused patient, more than for the young drug-overdose patient (p = 0.026, p = 0.001, and p < 0.001 for use of eyeglasses, Posey restraints, and wrist restraints, respectively). Chi-squared tests on contingency tables found that the use of physical restraints (Posey jacket and/or wrist restraints) had no significant relationship with the respondent's age, number of years in practice, patient population served by the ICU, or number of beds in the ICU. The use of physical restraints was not dependent on whether the respondents labeled the patient as having “delirium” (data not shown).
Non-pharmacological management. Star indicates statistically significant difference between scenarios B and C (p < 0.05); cross indicates statistically significant difference between scenarios A and B (p < 0.05); triangle indicates statistically significant difference between scenarios A and C (p < 0.05)
Pharmacological therapies
Figure 2 summarizes the most frequently used pharmacological interventions by scenario. The percentage of physicians choosing to use various classes of drugs is shown. Physicians were free to select more than one type of medication for each scenario. The most frequently used medications were typical antipsychotics (most commonly haloperidol), lorazepam, and atypical antipsychotics (including risperidone, olanzapine, and quetiapine). While over 97% of physicians chose to use some type of pharmacological intervention in the elderly cirrhotic and the elderly post-operative confused patient, only 54% of physicians chose to treat the young drug-overdose patient with antipsychotics or sedatives. (In the GEE model, p < 0.001 for comparisons of both A and C to B). Whether the patient was labeled as having “delirium” did not affect the use of drug therapy (data not shown).
Patterns of consultation
Physicians were then asked whether they would consult other medical or psychiatric services to help manage the patient's symptoms. The options offered included consulting to help manage the patient's current symptomatology, consultation only if the patient's symptoms deteriorated, and refusal to seek consultation. Over 50% of physicians asked for consultation to help manage the current symptoms in all three scenarios. Less than 20% of physicians would wait until the symptoms worsened in all three scenarios, and the others would not consult other medical or psychiatric services regardless. Separate ordinal logistic regression analyses in each scenario showed that the threshold for consultation did not depend on whether the physician diagnosed the patient with delirium; furthermore, chi-squared analyses found that consultation threshold was not related to the age of the physician, the number of years of practice, patient population serviced by the ICU, number of beds in the ICU, or primary practice environment for any of the scenarios (data not shown).
Physicians were then asked which medical service they were likely to consult within their practice environment, if they chose to consult at all. The most commonly selected service was psychiatry (50.5% in scenario A, 76.2% in scenario B, 56.9% in scenario C), followed by neurology (20.8% in scenario A, 21.6% in scenario B, and 20.0% in scenario C). Approximately 7% of physicians consulted geriatric medicine for the 70-year-old patients in scenarios A and C. Again, the decision to consult was independent of whether the specific diagnosis of “delirium” was made by the physician respondent (data not shown).
Discussion
This study is the first study to explore the semantic diagnostic classification and the therapeutic approach of Canadian intensivists to ICU delirium. The results of our self-administered mail-in questionnaire survey study show that although all three hypothetical scenarios met criteria for a diagnosis of delirium, there was wide variation in whether the label of “delirium” was identified to describe the patient's symptomatology. This finding suggests that the term “delirium,” at least among the intensivist population, lacks precision of use.
In our survey, we did not enquire specifically about whether respondents that labeled the patient as having “delirium” used standardized criteria to make this diagnosis; however, recent data suggest that only 16% of ICU health care staff use a specific tool for delirium assessment [7]. The use of a standardized tool for assessment of such cognitive changes in ICU patients (for example, using the CAM-ICU [1] or the Intensive Care Delirium Screening Checklist [15]) does not appear to decrease the variability in diagnosis of this condition [16]. Consensus as to the syndrome being diagnosed and treated is lacking. This important gap hinders meaningful application of clinical studies into patient care, such as therapeutic interventions.
Our data suggest that where there is a distinct path from etiology to symptomatology (e. g., perturbations in neurotransmitters directly attributable to drug use or withdrawal), the term is more likely to be used to describe symptomatology; however, if the link between etiology and symptomatology is not manifest, the term “delirium” is more likely to become a stand-alone diagnosis in itself. This has implications on the design of prevention and treatment studies. These different diagnostic groups within the common symptom presentation of delirium may have different responses to specific interventions which will need to be explicitly defined.
In addition to the described variability in how ICU practitioners diagnose acute cognitive and perceptual abnormalities in patients, there is also significant variation in how ICU practitioners treat these symptoms. Most intensivists would use non-invasive treatments frequently. Interestingly, almost half of respondents agreed with the use of wrist restraints for the elderly agitated patients in scenarios A and C, and more than 20% selected Posey jacket restraints. Data from the non-critical-care setting demonstrate that physical restraints had the highest relative risk among five independent precipitating factors for delirium [17], may increase delirium severity [18], and may lead to asphyxiation [19]. In the ICU, however, it is unclear that the same risk-benefit ratio is true. The increased nurse-to-patient ratio, and the potentially life-threatening consequences of extubation and central-line removal, may affect the risk-benefit ratio calculation. Finally, the effects of physical restraints on the course of cognitive and perceptual deficits in ICU patients remain unknown. Much research still needs to be done to elucidate the key factors in making this important decision.
With respect to drug therapy, our data indicated that typical and atypical antipsychotics and benzodiazepines were most likely to be the drugs of choice. The data did not ascertain whether they were likely to be used alone, in combination, or sequentially. Generally, the findings are consistent with guidelines on treatment of the agitated, delirious patient [13], although the guidelines themselves are vague as to the benefits and risks of benzodiazepines and the evidence base supporting pharmacotherapy in this setting is limited. Interestingly, a significant proportion of respondents would treat the cognitive and perceptual disturbances with anesthetic agents (mostly propofol) and opioid analgesics (morphine, fentanyl). This is of potential concern, given the findings of a recently published report suggesting that patients diagnosed with delirium in the ICU (based on the CAM-ICU) were more likely than those without delirium to receive continuous infusions of fentanyl, an opioid analgesic [20]. Indeed, a recent study found that sedatives and analgesics are deliriogenic when used to induce coma [21].
Whether or not a patient's cognitive and perceptual abnormalities were labeled as delirium did not affect subsequent management of the patient's symptoms. Since the term “delirium” itself is imprecisely used, medical labeling may not guide symptom-based drug or non-drug therapies.
Inter-ICU physician inconsistency in managing delirious patients can also be seen in the consultation patterns. Over half of respondents asked for expert consultation to help manage the patient's symptoms on presentation, most commonly the psychiatry service. Only 7% of respondents asked for help from geriatric medicine for the 70-year-old delirious patients. This may be indicative of local practice patterns, variability in available consultants, or other factors.
There are a number of limitations to the current study. The survey results represent only an approximation of ICU physician practice, as the 58.3% response rate was slightly below the previously reported average physician survey response rates of 61% [22]. Given that we did not have access to characteristics of non-respondents, self-selection bias may also affect the representativeness of the survey responses. In addition, how closely the responses reflect actual clinical practice is unknown. We did not directly sample actual practice; however, studies comparing methods for measuring quality of care (vignettes vs. chart abstraction, and standardized patients) found that vignettes were superior to chart abstraction when compared with use of standardized patients as the reference standard, and differed from the latter by only 5%, regardless of whether cases were simple or complex [23].
By virtue of its design, our survey did not allow for exploring the underlying reasoning behind the labeling of cognitive symptoms in the vignettes. Some respondents may have decided to choose a unifying diagnosis to explain the symptoms (e. g., hepatic encephalopathy), without specifically identifying the cognitive syndrome of delirium. Using a different design with direct questioning, it is possible that these respondents may indeed have identified the patients as suffering from delirium secondary to hepatic encephalopathy. This information, however, would be difficult to elicit in a written survey without introducing bias in the questions.
Conclusion
There is wide variability in the use of the term “delirium” to describe cognitive and perceptual changes in ICU patients. Canadian intensivists diagnose delirium based upon the presence or absence of an obvious medical etiology. Wide variation exists in approach to management, as well as patterns of consultation.
Appendix
Demographic Data
References
Ely W, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautman S, Bernard G, Inouye S (2001) Evaluation of delirum in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 29:1370–1379
Dubois M, Bergeron N, Dumont M, Dial S, Skrobik Y (2001) Delirium in an intensive care unit: a study of risk factors. Intensive Care Med 27:1297–1304
Lin S, Liu C, Wang C, Lin H, Huang C, Huang P, Fang Y, Shieh M, Kuo H (2004) The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med 32:2254–2259
McNicoll L, Pisani M, Zhang Y, Ely W, Siegel M, Inouye S (2003) Delirium in the Intensive Care Unit: occurrence and clinical course in older patients. J Am Geriatr Soc 51:591–598
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell F, Inouye SK, Bernard GR, Dittus RS (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. J Am Med Assoc 291:1753–1762
Ouimet S, Kavanagh B, Gottfried S, Skrobik Y (2007) Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 33:66–73
Ely EW, Stephens RK, Jackson JC (2007) Current opinions regarding the importance, diagnosis and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Crit Care Med 32:106–112
Carnes M, Howell T, Rosenberg M, Francis J, Hildebrand C, Knuppel J (2003) Physicians vary in approaches to the clinical management of delirium. J Am Geriatr Soc 51:234–239
Skrobik Y (2002) Haloperidol should be used sparingly. Crit Care Med 30:2613–2614
Gardner DM, Ross J, Baldessarini RJ, Waraich P (2005) Modern antipsychotic drugs: a critical overview. Can Med Assoc J 172:1703–1711
Kress JP, Pohlman AS, O'Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Meagher DJ (2001) Delirium: optimizing management. Br Med J 322:144–149
American Psychiatric Association (1999) Practice Guidelines for the treatment of patients with delirium. Am J Psychiatry 156:S1–S20
McGuire BE, Basten CJ, Ryan CJ, Gallagher J (2000) Intensive care unit syndrome: a dangerous misnomer. Arch Intern Med 160:906–909
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (2001) Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med 27:859–864
Riker RR, Robbins T, Bruce H, Fraser GL, Addor H (2006) ICU delirium assessment tools often disagree. Crit Care Med 34:A7
Inouye SK, Charpentier PA (1996) Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. J Am Med Assoc 275:852–857
McCusker J, Cole M, Abrahamowicz M (2001) Environmental risk factors for delirium in hospitalized older people. J Am Geriatr Soc 49:1327–1334
Rubin BS, Dube AH, Mitchell AK (1993) Asphyxial death due to physical restraint: case series. Arch Fam Med 2:405–408
Micek ST, Anand NJ, Laible BR, Shannon WD, Kollef MH (2005) Delirium as detected by the CMA-ICU predicts restraint use among mechanically ventilated medical patients. Crit Care Med 33:1260–1265
Inouye S, Van Dyck C, Alessi C, Balkin S, Siegal A, Horwitz R (1990) Clarifying confusion: the confusion assessment method. A new method for the detection of delirium. Ann Intern Med 113:941–948
Cummings SM, Savitz LA, Konrad TR (2001) Reported response rates to mailed physician questionnaires. Health Serv Res: 35:1347–1355
Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M (2000) Comparison of vignettes, standardized patients, and chart abstraction. J Am Med Assoc 283:1715–1722
Author information
Authors and Affiliations
Corresponding author
Additional information
C.Z. Cheung, S.M.H. Alibhai, M. Robinson, G. Tomlinson, D. Chittock, J. Drover, Y. Skrobik, for the Canadian Critical Care Trials Group.
Rights and permissions
About this article
Cite this article
Cheung, C.Z., Alibhai, S.M.H., Robinson, M. et al. Recognition and labeling of delirium symptoms by intensivists: Does it matter?. Intensive Care Med 34, 437–446 (2008). https://doi.org/10.1007/s00134-007-0947-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0947-x