Abstract
Objective
We compared brain tissue oxygen tension (PtiO2) measured in peri-focal and in normal-appearing brain parenchyma on computerized tomography (CT) in patients following traumatic brain injury (TBI).
Design
Prospective observational study.
Setting
Neurointensive care unit.
Patients and participants
Thirty-two consecutive TBI patients were subjected to PtiO2 monitoring.
Interventions
Peri-focal tissue was identified by the presence of a hypodense area of the contusion and/or within 1 cm from the core of the contusion. The position of the tip of the PtiO2 probe was assessed at follow-up CT scan.
Measurements and results
Mean PtiO2 in the peri-contusional tissue was 19.7 ± 2.1 mmHg and was lower than PtiO2 in normal-appearing tissue (25.5 ± 1.5 mmHg, p < 0.05), despite a greater cerebral perfusion pressure (CPP) (73.7 ± 2.3 mmHg vs. 67.4 ± 1.4 mmHg, p < 0.05). We observed both in peri-focal tissue and in normal-appearing tissue episodes of brain hypoxia (PtiO2 < 20 mmHg for at least 10 min), whose median duration was longer in peri-focal tissue than in normal-appearing tissue (51% vs. 34% of monitoring time, p < 0.01). In peri-focal tissue, we observed a progressive PtiO2 increase from pathologic to normal values (p < 0.01).
Conclusions
Multiple episodes of brain hypoxia occurred over the first 5 days following severe TBI. PtiO2 was lower in peri-contusional tissue than in normal-appearing tissue. In peri-contusional tissue, a progressive increase of PtiO2 from pathologic to normal values was observed over time, suggestive of an improvement at microcirculatory level.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Severe traumatic brain injury (TBI) is the leading cause of death in young adults in developed countries and leads to significant disability and breakdown of personal relationships in survivors, resulting in an enormous cost to society [1]. To date, TBI management is based on prompt diagnosis and removal of intracranial mass lesions and avoidance/treatment of intracranial and systemic insults [2].
Global and regional cerebral ischemia/hypoperfusion have been observed in animal models of TBI, in brain-injured patients and following analysis of post-mortem tissue [3–5]. Measures taken to insure adequate cerebral oxygenation are therefore of paramount importance in the management of TBI. The evaluation of brain oxygenation in TBI patients has been traditionally performed using measurements of jugular bulb hemoglobin oxygen saturation (SjO2) and evaluation of arterio–jugular oxygen difference (AjDO2), which permit the identification of global cerebral ischemia. However, regional cerebral ischemia has been reported during the first 24 h post injury following TBI despite the presence of normal SjO2 saturation and AjDO2, with potential deleterious effects on the final outcome of these patients [6].
The measurement of cerebral blood flow (CBF), oxygen extraction fraction (OEF), brain oxygenation and cerebral metabolic rate of oxygen (CMRO2) can be performed using positron emission tomography (PET), which provides information on global and regional brain oxygenation following TBI [7–10]. However, this monitoring technique can be performed only in selected centers and it has the limitation of offering only a snapshot of brain perfusion, while the evaluation of brain at risk for hypoxia ideally requires a continuous method of monitoring.
Brain tissue oxygen tension (PtiO2), the measurement of the mean tissue O2 tension over a volume of a few cubic millimeters that contains extracellular fluid, capillaries, cells, and axons, can be measured using sensors placed directly into the brain parenchyma [11]. PtiO2 represents a balance between O2 delivery (DO2) to the brain and its consumption. Advantages of this technique include the ability to detect changes in regional brain oxygenation that would otherwise be missed by measuring SjO2 [12] and its ability to provide data continuously over long periods during the critically acute post-traumatic period. Following TBI, a relationship has been established between outcome and PtiO2 levels and/or PtiO2 reactivity to hyperoxia [13–17]. However, a debate still exists on whether this technique should be employed in apparently undamaged brain parenchyma (normal-appearing regional monitoring, reflective of global oxygenation), or preferably in the penumbral zone of contusions/infarctions (peri-focal regional monitoring), with the objective of monitoring vulnerable regions. In this study, we describe and compare the PtiO2 measured in undamaged and in peri-focal brain parenchyma of patients following TBI.
Materials and methods
Patient population
The study was approved by the Local Research Ethics Committee of the Ospedale Maggiore Policlinico, Milan. Inclusion criteria were:
-
Age over 15 years
-
Severe TBI requiring mechanical ventilation
-
CT scan evidence of cerebral traumatic lesions
-
ICP monitoring
-
Informed consent from the next of kin
Evidence of coagulopathy was an exclusion criterion. Patients (n = 32) admitted to our neurosurgical ICU following TBI were enrolled as subjects in this study.
Clinical management
Consecutive patients were admitted to ICU after initial stabilization or surgical evacuation of an intracranial hematoma. Management goals included arterial tissue oxygen tension (PaO2) > 100 mmHg, mean arterial pressure (MAP) > 90 mmHg, ICP < 20 mmHg, with CPP > 60 mmHg, in accordance with established guidelines for the management of severe head injury [2]. CPP was calculated as the difference between MAP and ICP with transducers calibrated to zero at the foramen of Monro. ICP was measured with intraventricular catheters in 4 patients, intraparenchymal catheters in 14 and subdural catheters in 14. All patients had a jugular bulb catheter to allow for determination of SjO2 saturation and calculation of AjDO2 differences according to the following formula: AjDO2 = [(arterial saturation of O2–jugular saturation of O2)*hemoglobin grams*1.34]+[(arterial PO2–jugular PO2 mmHg)*0.003]. The internal jugular vein was cannulated ipsilaterally to the more damaged hemisphere. The tip was positioned at the jugular superior bulb and correct placement of the catheter was confirmed by skull X-ray.
Brain PtiO2 monitoring
Brain PtiO2 was continuously measured using a polarographic Clark-type microcatheter (Licox, Kiel, Germany) or a multiparameter sensor (Neurotrend Cerebral Tissue Monitoring System; Codman, Bracknell, UK). Patients underwent insertion of the PtiO2 probe in the operating room either under direct vision after neurosurgical interventions, otherwise through a burr hole. In patients with cerebral contusions detected by computed tomography (CT), our objective was to insert the probe within the hypodense area around the core of the contusion. PtiO2 monitoring commenced after radiological identification of contusion with a surrounding hypodense area. In patients with diffuse injury and no visible contusions on CT scan, the PtiO2 probe was inserted concomitant with the placement of the probe for ICP monitoring. A postoperative CT scan was performed to determine the proper position of the sensor. (Our standard protocol consists of scans at 5-mm intervals in the posterior fossa and 10-mm intervals in the supratentorial space. We used 5-mm slice intervals in the supratentorial space too in cases in which we needed to clarify the position of the probe tip.) Monitoring of PtiO2 in peri-focal tissue was defined by the presence of the tip of the probe in the hypodense area of the contusion (as seen on CT scan) and/or within 1 cm from the core of the contusion, since this tissue recapitulates a penumbra-like condition as recently shown by measuring regional CBF [18]. One centimeter away apart from the contusion core and outside the hypodense peri-contusional tissue, the CBF is above the ischemic threshold and comparable to normal-appearing control tissue [18]. The measurement of the distance between PtiO2 probe and the core of the contusion was performed using the Osiris imaging software (Digital Imaging Unit, University Hospital of Geneva, Switzerland). Brain PtiO2 was allowed to stabilize for 2 h after insertion of the probe. When Licox was used, PtiO2 was corrected by the temperature.
Data management
MAP, ICP and PtiO2 data were transmitted from the monitor to a computer through an analog–digital (AD) converter (Mac Lab; World Precision Instruments Castle Hill, NSW, Australia) for storage and analysis. Artifacts caused by nursing interventions or by temporary disconnection of catheters because of transport were manually eliminated from the datasets. Episodes of brain hypoxia (lasting at least 10 min) were categorized as “moderate hypoxia” if PtiO2 was in the range 10–19 mmHg or as severe hypoxia if PtiO2 was < 10 mmHg [11, 14–16, 19–25].
Statistical analysis
Data are presented as mean ± standard error of the mean. Data in the peri-focal and normal-appearing group were compared using a t-test. Non-parametric data are presented as median values and were compared using Mann–Whitney test. The incidence of episodes of brain hypoxia between the two groups was compared using the Fisher exact test. Trends of PtiO2 and CPP over time were evaluated using an analysis of variance (ANOVA) for repeated measurements by a mixed procedure (SAS System, version 8; SAS Institute, Cary, NC). The variables PtiO2 and CPP were modeled as linear functions of time (SAS System for Mixed Models, Cary, NC: SAS Institute, 1996). A difference with a probability of less than 0.05 was considered statistically significant.
Results
Patients' characteristics
Mean age was 37.5 ± 3.6 years (range 16–85 years) and 6 (19%) were female. The median post-resuscitation Glasgow coma score (GCS) was 5 (it was similar in the two groups); 81% of patients had an initial GCS ≤ 8. All patients had a GCS ≤ 8 at the time of PtiO2 monitoring. According to the Marshall CT classification, 9 patients were classified as diffuse injury II (1 peri-focal group), 1 patient as diffuse injury III (normal-appearing group), 20 patients as evacuated mass lesions (14 peri-focal group) and 2 patients as non-evacuated mass lesions (normal-appearing group) [26].
PtiO2 monitoring in peri-focal versus normal-appearing tissue
A total of 34 probes were placed intracranially to monitor PtiO2. Two patients received two probes, (one for repositioning and the second because the first probe stopped working properly). Fifteen of the 34 probes were placed directly in the area adjacent to a focal lesion. Monitoring of PtiO2 began on day 3 post injury in the peri-focal tissue “group” and day 2 post injury in the normal-appearing tissue “group”, continuing for 71 ± 8.7 h and 85 ± 8.5 h (p = 0.2), respectively.
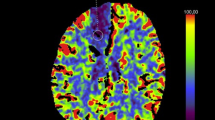
Mean PtiO2 in peri-focal tissue was 19.7 ± 2.1 mmHg, significantly lower than in normal-appearing tissue (25.5 ± 1.5 mmHg, p < 0.05; Fig. 1) despite higher CPP (73.7 ± 2.3 mmHg vs. 67.4 ± 1.4 mmHg, p < 0.05). No additional differences were observed in other variables that could have influenced the PtiO2 as shown in Table 1.
Incidence of brain hypoxia
Brain hypoxia (PtiO2 < 20 mmHg) was observed when PtiO2 was measured in both peri-focal and normal-appearing tissue. The duration of cerebral hypoxia in peri-focal tissue (51% of monitoring time) was significantly greater than that observed in normal-appearing tissue (34%, p < 0.01; Fig. 2). The median duration of hypoxic episodes of moderate severity (PtiO2 10–19 mmHg) was significantly longer in the peri-focal tissue compared to the normal-appearing tissue, (p < 0.01; Table 2). We observed 75 episodes of severe brain hypoxia, where PtiO2 sank to less than 10 mmHg, in the peri-focal tissue and 102 episodes in the normal-appearing tissue; however the median duration of these episodes and the total time of severe brain hypoxia were significantly longer in the peri-focal tissue than in the normal-appearing tissue (p < 0.05; Table 2).
Brain hypoxia in the peri-focal tissue
In the peri-focal tissue, no significant relationship was observed between PtiO2 and CPP, PaO2, PaCO2 or Hb. Interestingly, CPP was < 60 mmHg in only 4.8% of the cases, suggesting that only in a minority of episodes was global hypoperfusion associated with regional brain hypoxia. Moderately hypoxic episodes (mean PtiO2 14.5 ± 0.2 mmHg) and severely hypoxic episodes (mean PtiO2 7.2 ± 0.2 mmHg) were associated with similar values of CPP (75.9 ± 1 mmHg and 73.1 ± 1.6 mmHg respectively, p = ns), PaO2 (156 ± 2.6 mmHg and 151 ± 3.7 mmHg, p = ns), PaCO2 (28.8 ± 0.9 mmHg and 28 ± 0.5 mmHg, p = ns) and Hb (9.2 ± 0.1 g/100 ml and 9 ± 0.1 g/100 ml, p = ns). Parameters of global cerebral oxygenation were not suggestive of regional brain hypoxia since during moderate versus severe hypoxia AjDO2 was 3.3 ± 0.1 vol. % and 3.2 ± 0.18 vol. %, respectively (p = ns).
Brain hypoxia in normal-appearing tissue
Also in normal-appearing tissue, no relationship was observed between PtiO2 and CPP, PaO2, PaCO2 and Hb. Reduced CPP (< 60 mmHg) was observed in 17% of the cases, which was a significantly greater proportion than in the peri-focal tissue (p < 0.01). Moderately hypoxic episodes (mean PtiO2 14.7 ± 0.2 mmHg) and severely hypoxic episodes (mean PtiO2 7.5 ± 0.13 mmHg) showed similar values for PaO2 (133 ± 1.7 mmHg and 134 ± 2.6 mmHg, p = ns) and Hb (10.1 ± 0.06 g/100 ml and 10 ± 0.08 g/100 ml, p = ns). In contrast, CPP during severe brain hypoxia in the normal-appearing tissue (76.2 ± 1.8 mmHg) was significantly greater than that observed during moderate hypoxia (72 ± 1 mmHg, p < 0.05). Moreover, we observed a significantly greater PaCO2 during severe hypoxia (32.7 ± 0.4 mmHg) than during moderate hypoxia (31 ± 0.3 mmHg, p < 0.01). AjDO2 values were similar during episodes of severe and moderate hypoxia (4.5 ± 0.08 vol. % and 4.8 ± 0.14 vol. % respectively, p = 0.08).
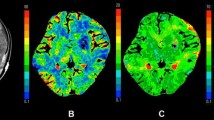
PtiO2 over time in peri-focal and normal-appearing tissue
In peri-focal tissue, a progressive elevation in PtiO2 was observed over time during the first 4 days of monitoring (p = 0.01). Brain oxygenation was < 20 mmHg during the first 36 h, then progressively rose and stabilized during the subsequent 2 days. During the first 12 h of monitoring, PtiO2 was < 20 mmHg in 11 patients and rose to normal values in 7 of them. In contrast, we observed only a slight increase in CPP during the same period (p = 0.28, Fig. 3a). In the normal-appearing tissue, the average PtiO2 was normal during the first 4 days of ICU monitoring (range 20.4 ± 2.6 mmHg to 30.2 ± 3.9 mmHg, Fig. 3b).
PtiO2 over time in peri-focal and normal-appearing tissue. In peri-focal tissue we observed a progressive PtiO2 increase over time from pathologic values to normal values (p = 0.01) with no significant change in CPP (p = 0.28; a). In normal-appearing tissue we did not observe any trend during the monitoring either for PtiO2 (p = 0.18) and for CPP (p = 0.34; b). Data are presented as mean of 12 h of monitoring (“studies”) ± standard error of the mean
Discussion
In the present study we observed that (1) PtiO2 is lower in the peri-contusional tissue than in normal-appearing tissue despite a significantly greater CPP; (2) episodes of regional brain hypoxia (undetected by measures of global cerebral oxygenation) occur both in normal-appearing and in peri-contusional tissue; (3) in peri-contusional tissue, a progressive PtiO2 increase from pathologic to normal values occurs over time, suggestive of an improvement at the microcirculatory level.
A debate exists on whether PtiO2 should be monitored in apparently undamaged brain parenchyma, or in the penumbral zone of contusions [27], with the objective of detecting brain hypoxia in vulnerable regions that may be overlooked by the monitoring of global cerebral oxygenation [6]. In our study, peri-focal PtiO2 was significantly lower than PtiO2 measured in normal-appearing tissue. Oxygen transport to the brain depends on the respiratory and circulatory systems and on local vascular factors. Oxygen is transported from alveolar air to blood and from blood to peripheral tissues and finally to the mitochondria via diffusion steps. At the microvascular level, oxygen diffusion is mostly dependent on the tension gradient between vessels and tissue and is inversely related to the diffusion distance [25]. The two groups in our study were similar in terms of blood oxygen content and PaCO2, and it is unlikely that the significantly greater CPP (73.7 ± 2.3 mmHg vs. 67.4 ± 1.4 mmHg) would translate into an increased global CBF (assuming preserved pressure autoregulation). Electron-microscopic analysis of contused brain tissue removed during neurosurgical procedures in patients following TBI has shown glial swelling with narrowing of blood vessels whose lumen might be occluded by circulating leukocytes/red blood cells and microthrombi [21, 28, 29], suggesting that a reduced regional CBF and a relative reduction of vessels/capillary density within the hypodense area of a cerebral contusion might be responsible for the reduced local oxygen delivery and diffusion, leading to the lower PtiO2 in peri-focal tissue.
To date, some uncertainty remains concerning the critical PtiO2 threshold, because different studies have utilized different probes (Licox, Paratrend and Neurotrend) placed in different locations (gray versus white matter) and because the threshold and duration of hypoxia associated with irreversible damage to the CNS has not been clarified. Since proposed thresholds have ranged from 5 mmHg to 20 mmHg using the Licox and the Neurotrend [11, 14–16, 20–25, 30], we defined moderate brain hypoxia as a PtiO2 in the range 10–19 mmHg and severe brain hypoxia as PtiO2 < 10 mmHg. In our patients brain hypoxia occurred in normal-appearing tissue and in peri-focal tissue, where it persisted for a longer time. Kiening et al. showed that the hypoxic SjO2 threshold of 50% corresponded to a PtiO2 of 8.5 mmHg, and indicated a CPP cut-off of 60 mmHg at which SjO2 and PtiO2 were shown to be sufficient [20]. In our study we observed that a normal SjO2 does not exclude regional brain hypoxia, suggesting that PtiO2 monitoring should be performed in addition to SjO2 measurements. We attempted to relate hypoxic episodes with intracranial/systemic complications but we could not find any relationship between brain hypoxia and hypotension, hypoxemia, anemia or hypocapnia, suggesting that in order to understand the pathophysiology of PtiO2 we should move from a focus on macrocirculation to microcirculation and that local O2 diffusion alterations from blood vessels to the tissue are likely to be the major determinant of the observed pathologic PtiO2 [21, 31].
Although van den Brink et al. observed that PtiO2 monitored in normal-appearing tissue was pathologic in about 50% of comatose TBI patients during the first 12–24 h post injury and then increased to normal levels for 5 days post injury [15], we did not observe any significant trend in PtiO2 over time in normal-appearing tissue. A possible explanation of these difference is that van den Brink and colleagues initiated PtiO2 monitoring within the first 12 h post injury while our study commenced on the 2nd day post injury, when global CBF is likely to be restored [10]. In contrast, in peri-focal tissue we observed a progressive PtiO2 improvement that was not linked to a similar CPP trend, suggesting that this improvement might be the result of changes at microvascular level [32], such as local vasodilation, edema reduction, and lysis of microthrombosis.
Our study has limitations: Since we could not measure the CBF, our data interpretation is largely hypothetical. Additionally, our evaluation of peri-focal tissue was strictly based on a morphological evaluation. Since we used two different catheters, we evaluated whether the observed difference in peri-focal and normal-appearing groups could be due to the different technology. Neurotrend (which underestimates PtiO2 compared to Licox [33]) was used only in normal-appearing tissue, where PtiO2 values were higher; therefore, catheter location was the determinant of the results of the study (data not shown).
In our study PtiO2 monitoring and comparison between normal-appearing and peri-focal tissue was performed in different patients starting respectively on day 2 and day 3 post-injury. Ideally, the comparison of PtiO2 in “normal” and peri-contusional brain would be to monitor the two areas in the same patient. However, because of the invasive nature of this technology, we consider the insertion of two probes unethical.
Our findings confirm that PtiO2 provides information not disclosed by other monitoring modalities, such as CPP or AjDO2, and critically dependent on the position of the probe. Unsuspected transient episodes of brain hypoxia have been detected both in contused and normal-appearing tissue. The consequences of these episodes on long-term outcome require further investigation.
References
Anonymous (1999) Consensus conference. Rehabilitation of persons with traumatic brain injury. NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury. JAMA 282:974–983
Brain Trauma Foundation (2007) Guidelines for the Management of Severe Traumatic Brain Injury. J Neurotrauma 24 [Suppl 1]:S1–S95
Bouma GJ, Muizelaar JP, Choi SC, Newlon PG, Young HF (1991) Cerebral circulation and metabolism after severe traumatic brain injury: the elusive role of ischemia. J Neurosurg 75:685–693
Graham DI, Ford I, Adams JH, Doyle D, Teasdale GM, Lawrence AE, McLellan DR (1989) Ischaemic brain damage is still common in fatal non-missile head injury. J Neurol Neurosurg Psychiatry 52:346–350
Yamakami I, McIntosh TK (1989) Effects of traumatic brain injury on regional cerebral blood flow in rats as measured with radiolabeled microspheres. J Cereb Blood Flow Metab 9:117–124
Coles JP, Fryer TD, Smielewski P, Chatfield DA, Steiner LA, Johnston AJ, Downey SP, Williams GB, Aigbirhio F, Hutchinson PJ, Rice K, Carpenter TA, Clark JC, Pickard JD, Menon DK (2004) Incidence and mechanisms of cerebral ischemia in early clinical head injury. J Cereb Blood Flow Metab 24:202–211
Bergsneider M, Hovda DA, Shalmon E, Kelly DF, Vespa PM, Martin NA, Phelps ME, McArthur DL, Caron MJ, Kraus JF, Becker DP (1997) Cerebral hyperglycolysis following severe traumatic brain injury in humans: a positron emission tomography study. J Neurosurg 86:241–251
Glenn TC, Kelly DF, Boscardin WJ, McArthur DL, Vespa P, Oertel M, Hovda DA, Bergsneider M, Hillered L, Martin NA (2003) Energy dysfunction as a predictor of outcome after moderate or severe head injury: indices of oxygen, glucose, and lactate metabolism. J Cereb Blood Flow Metab 23:1239–1250
Hutchinson PJ, Gupta AK, Fryer TF, Al Rawi PG, Chatfield DA, Coles JP, O'Connell MT, Kett-White R, Minhas PS, Aigbirhio FI, Clark JC, Kirkpatrick PJ, Menon DK, Pickard JD (2002) Correlation between cerebral blood flow, substrate delivery, and metabolism in head injury: a combined microdialysis and triple oxygen positron emission tomography study. J Cereb Blood Flow Metab 22:735–745
Martin NA, Patwardhan RV, Alexander MJ, Africk CZ, Lee JH, Shalmon E, Hovda DA, Becker DP (1997) Characterization of cerebral hemodynamic phases following severe head trauma: hypoperfusion, hyperemia, and vasospasm. J Neurosurg 87:9–19
Haitsma IK, Maas AI (2002) Advanced monitoring in the intensive care unit: brain tissue oxygen tension. Curr Opin Crit Care 8:115–120
Gupta AK, Hutchinson PJ, Al Rawi P, Gupta S, Swart M, Kirkpatrick PJ, Menon DK, Datta AK (1999) Measuring brain tissue oxygenation compared with jugular venous oxygen saturation for monitoring cerebral oxygenation after traumatic brain injury. Anesth Analg 88:549–553
Maas AI, Fleckenstein W, de Jong DA, van Santbrink H (1993) Monitoring cerebral oxygenation: experimental studies and preliminary clinical results of continuous monitoring of cerebrospinal fluid and brain tissue oxygen tension. Acta Neurochir Suppl (Wien) 59:50–57
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS (1998) Relationship of brain tissue PO2 to outcome after severe head injury. Crit Care Med 26:1576–1581
van den Brink WA, van Santbrink H, Steyerberg EW, Avezaat CJ, Suazo JA, Hogesteeger C, Jansen WJ, Kloos LM, Vermeulen J, Maas AI (2000) Brain oxygen tension in severe head injury. Neurosurgery 46:868–876
van Santbrink H, Maas AI, Avezaat CJ (1996) Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery 38:21–31
Zauner A, Doppenberg EM, Woodward JJ, Choi SC, Young HF, Bullock R (1997) Continuous monitoring of cerebral substrate delivery and clearance: initial experience in 24 patients with severe acute brain injuries. Neurosurgery 41:1082–1091
Steiner LA, Coles JP, Johnston AJ, Czosnyka M, Fryer TD, Smielewski P, Chatfield DA, Salvador R, Aigbirhio FI, Clark JC, Menon DK, Pickard JD (2003) Responses of posttraumatic pericontusional cerebral blood flow and blood volume to an increase in cerebral perfusion pressure. J Cereb Blood Flow Metab 23:1371–1377
Johnston AJ, Steiner LA, Coles JP, Chatfield DA, Fryer TD, Smielewski P, Hutchinson PJ, O'Connell MT, Al Rawi PG, Aigbirihio FI, Clark JC, Pickard JD, Gupta AK, Menon DK (2005) Effect of cerebral perfusion pressure augmentation on regional oxygenation and metabolism after head injury. Crit Care Med 33:189–195
Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR (1996) Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg 85:751–757
Menon DK, Coles JP, Gupta AK, Fryer TD, Smielewski P, Chatfield DA, Aigbirhio F, Skepper JN, Minhas PS, Hutchinson PJ, Carpenter TA, Clark JC, Pickard JD (2004) Diffusion limited oxygen delivery following head injury. Crit Care Med 32:1384–1390
Nortje J, Gupta AK (2006) The role of tissue oxygen monitoring in patients with acute brain injury. Br J Anaesth 97:95–106
Stiefel MF, Udoetuk JD, Spiotta AM, Gracias VH, Goldberg A, Maloney-Wilensky E, Bloom S, Le Roux PD (2006) Conventional neurocritical care and cerebral oxygenation after traumatic brain injury. J Neurosurg 105:568–575
Stocchetti N, Chieregato A, De Marchi M, Croci M, Benti R, Grimoldi N (1998) High cerebral perfusion pressure improves low values of local brain tissue O2 tension (PtiO2) in focal lesions. Acta Neurochir Suppl 71:162–165
Zauner A, Daugherty WP, Bullock MR, Warner DS (2002) Brain oxygenation and energy metabolism. I. Biological function and pathophysiology. Neurosurgery 51:289–301
Marshall LF, Marshall SB, Klauber MR, Clark MvB, Eisenberg HM, Jane JA, Luerssen TG, Marmarou A, Foulkes MA (1991) A new classification of head injury based on computerized tomography. J Neurosurg [Suppl] 75
Rose JC, Neill TA, Hemphill JC III (2006) Continuous monitoring of the microcirculation in neurocritical care: an update on brain tissue oxygenation. Curr Opin Crit Care 12:97–102
Schroder ML, Muizelaar JP, Bullock MR, Salvant JB, Povlishock JT (1995) Focal ischemia due to traumatic contusions documented by stable xenon-CT and ultrastructural studies. J Neurosurg 82:966–971
Stein SC, Chen XH, Sinson GP, Smith DH (2002) Intravascular coagulation: a major secondary insult in nonfatal traumatic brain injury. J Neurosurg 97:1373–1377
Longhi L, Valeriani V, Rossi S, De Marchi M, Egidi M, Stocchetti N (2002) Effects of hyperoxia on brain tissue oxygen tension in cerebral focal lesions. Acta Neurochir Suppl 81:315–317
Stocchetti N, Longhi L (2004) Moving from macro- to microcirculation in head injury. Crit Care Med 32:1429–1430
Thomale UW, Kroppenstedt SN, Beyer TF, Schaser KD, Unterberg AW, Stover JF (2002) Temporal profile of cortical perfusion and microcirculation after controlled cortical impact injury in rats. J Neurotrauma 19:403–413
Jaeger M, Soehle M, Schuhmann MU, Winkler D, Meixensberger J (2005) Correlation of continuously monitored regional cerebral blood flow and brain tissue oxygen. Acta Neurochir (Wien) 147:51–56
Acknowledgements
The authors thank Angelo Colombo, MD for computer support, data processing and statistical advice; the students and nursing staff of the neurointensive care unit for their valuable cooperation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Longhi, L., Pagan, F., Valeriani, V. et al. Monitoring brain tissue oxygen tension in brain-injured patients reveals hypoxic episodes in normal-appearing and in peri-focal tissue. Intensive Care Med 33, 2136–2142 (2007). https://doi.org/10.1007/s00134-007-0845-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0845-2