Abstract
Objective
Diaphragmatic palsy (DP) is a rare but severe complication after surgery for congenital heart disease. Transthoracic diaphragmatic plication is an effective means of treatment for those with respiratory impairment due to DP, but little is known about the mid-term effects of diaphragmatic plication.
Design
We performed a study in 24 patients with history of DP. Diaphragm movement was assessed using ultrasound. Patients with DP who were old enough were additionally followed-up with lung function and exercise testing. A group of patients with similar age, diagnoses and operations served as controls.
Results
Ultrasound showed that in the majority of cases with history of DP the paralysed diaphragm was static, independently of whether it was plicated or not. Patients with DP had a more restrictive lung function pattern (VC: 54.3 vs. 76.4% predicted, p < 0.001; FEV1: 58.4 vs. 86.2% predicted, p < 0.001) and a lower exercise capacity compared with the control group (peak VO2: 24.5 vs. 31.3 ml/kg/min, p = 0.03). Comparing patients with and without plication for DP, only a tendency towards lower lung function values in patients after diaphragmatic plication, but no differences regarding exercise capacity, could be found.
Conclusions
Our results provide evidence that DP is a serious surgical complication with a reduction in lung function and exercise capacity, even at mid-term follow-up; however, diaphragmatic plication, a useful tool in treating post-surgical DP in children with respiratory impairment, seems to be without mid-term risk in terms of recovery of phrenic nerve function, lung function values, and exercise capacity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diaphragmatic paralysis following phrenic nerve injury is a rare but serious complication after cardiac surgery in children and adults [1, 2] with a higher prevalence in neonates and small infants. The reported prevalence in children varies between 0.4 [3] and 16% [4] depending on the type of study, age and diagnoses of the patient group and other factors. Postoperative phrenic nerve lesion can occur as a consequence of contusion, dissection, stretch and hyperthermic or hypothermic damage [5–7]. Because newborns, infants and small children lack compensatory mechanisms, such as strong intercostal muscles, stable mediastinum and an upright course of the ribs to counteract a raised diaphragm and/or the paradoxical movement of the diaphragm [8–10], acute diaphragmatic palsy is more significant in these patients. Acute postoperative diaphragmatic palsy presents with dyspnoea and respiratory distress, and is often complicated by the need for prolonged mechanical ventilation, an increased incidence of pulmonary infections and a prolonged hospital stay [11]. As many reports have shown, unilateral diaphragmatic plication can be useful to reverse the negative effects of diaphragmatic paralysis and facilitate weaning from mechanical ventilation a few days later [12–15]. Our experience concerning diaphragmatic palsy and diaphragmatic plication as an effective means of treatment has been reported previously [11]; however, even if diaphragmatic plication is helpful to wean children from mechanical ventilation and may prevent its negative long-term effects, we do not know whether it is beneficial for the future of our patients. So far little is known about the mid-term outcome of infants and children with post-surgical diaphragmatic paralysis or the mid-term effects of diaphragmatic plication in terms of lung function and exercise capacity. In adult patients some reports with small patient numbers have shown objective evidence that all lung volumes, with the exception of functional residual capacity (FRC), are improved following diaphragmatic plication [6, 16].
Therefore, the aim of the present study was to look at the mid-term outcome of these young patients with post-surgical diaphragmatic paralysis and to answer the following questions:
1. Is there a difference between children with diaphragmatic paralysis and children who underwent equivalent surgical interventions without the complication of diaphragmatic paralysis concerning lung function and exercise capacity?
2. Are there differences between children with and without diaphragmatic plication concerning lung function and exercise capacity?
3. Is there recovery of the phrenic nerve? What is the role of diaphragmatic plication in possible spontaneous recovery of diaphragmatic function?
Patients and methods
In the present mixed retrospective and prospective study 24 patients with a history of postoperative diaphragmatic paralysis after surgery for congenital heart disease underwent assessment of diaphragm movement, lung function and/or exercise capacity during routine follow-up between January 2001 and December 2003 (for general patient data see Table 1). Follow-up examinations were performed according to the patients' age and compliance. During these years we had an incidence of 1.4% for diaphragmatic paralysis as a complication arising during surgery for congenital heart disease, as described previously [11]. Around one-third of the patients have been followed-up and analyzed in the present study. Patients and their parents, where appropriate, gave their agreement to publication of the data.
Twenty-three patients were followed-up with ultrasound or fluoroscopy to examine the movement of the diaphragm, 15 patients underwent lung function testing with spirometry and 15 patients underwent bicycle spiroergometry to test exercise capacity. Patients had a median age at surgery of 1.8 years (range 8 days to 22 years). Diaphragmatic palsy was suspected on the basis of clinical findings and the diagnosis was confirmed, in the majority of cases, by ultrasound sonography. Eleven patients received plication of a paralysed diaphragm to flatten the diaphragm in its inspiratory position using the modified central pleating technique described by Schwartz and Filler [14] and Shoemaker [15]. Diaphragmatic plication was performed at a median of 121 days after initial surgery (range 22 days to 3.9 years). Indications for plication were failed weaning from mechanical ventilation, severe recurrent pulmonary infections with the need for hospitalization and in some patients univentricular hemodynamics [11, 17]. Due to only rare experience in our center and controversial opinions concerning the benefit of diaphragmatic plication in the 1980s and 1990s, diaphragmatic plication in the patients described here was performed later than we would recommend today. Additionally, it should be mentioned that 3 of the patients with TCPC presented here without plication underwent plication later.
At follow-up patients with diaphragmatic paralysis had a median age of 9.5 years (range 4.1–27.2 years) and the median time since initial surgery was 5.5 years (range 2.9–12.6 years).
Control group
Patients who had had cardiac surgery for comparable diagnosis and indications – without the complication of diaphragmatic paralysis – who underwent lung function testing or bicycle spiroergometry during routine follow-up between January 2001 and December 2003 served as controls. The general data of the control patients for lung function testing and spiroergometry is given in Table 2. Because of the wide spectrum and the complexity of diagnoses and types of operations, analysis of matched pairs could not be performed.
The controls, like the patients, did not have any known severe comorbidity besides the corrected or palliated congenital heart disease.
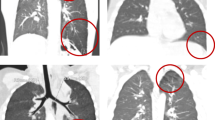
Ultrasound detection of diaphragmatic movement
Twenty-three patients with diaphragmatic palsy were followed up. Movement of the diaphragm was measured by ultrasonography in a lateral or subcostal view and graded as normal, static or paradoxical. In children who underwent heart catheterization for other reasons, movement of the diaphragm was evaluated using fluoroscopy.
Additionally, children who were of eligible age underwent lung function testing and/or cardiopulmonary exercise testing.
Lung function testing
Lung function was assessed in 15 patients with diaphragmatic palsy and 39 controls. If lung function analysis and exercise testing was done in the same patient, spirometry was performed before the exercise testing.
Cardiopulmonary exercise testing
Exercise capacity was assessed in 15 patients with DP and 80 controls using symptom-limited, bicycle-based maximal exercise testing according to the Jones protocol [18]. Patients were encouraged to exercise to exhaustion. During the tests patients wore a tightly fitting face mask connected to a capnograph and a sample tube enabling online measurement of ventilation and metabolic gas exchange (Jaeger, Hoechberg, Germany). We measured maximum effort, peak oxygen consumption (peak VO2) as an index of exercise capacity and the ventilatory response to exercise as measured by the slope of the relation between ventilation and carbon dioxide production (VE/VCO2 slope; this was displayed graphically throughout the test).
Statistical analysis
Statistical analysis was performed to detect differences between patients with diaphragmatic dysfunction and the control group. In the group of children with diaphragmatic paralysis we compared the mid-term outcome of patients who had received diaphragmatic plication with that of patients who had not.
Statistical analysis was performed using SPSS 12.0. Data are given as frequencies, medians and ranges, and mean ± 1 SD as appropriate. Patient demographics, lung function and exercise testing variables were compared between patients with DP and controls and in patients with DP between those with and without diaphragmatic plication. The Mann-Whitney U-test or contingency table analysis was applied, and for lung function and exercise testing variables a two-step univariate analysis was used. In a preliminary correlation analysis gender, body-mass index and age at follow-up were found to be confounders concerning lung function and especially exercise testing parameters; therefore, two-step univariate analysis was performed with gender as cofactor and body-mass index and age at follow-up as covariates. A probability value of p < 0.05 was taken to suggest that differences observed between the patients with diaphragmatic palsy and the control population, as well as between patients with DP with diaphragmatic plication and without, were significant.
Results
Diaphragmatic movement: Ultrasound detection
Patients who underwent ultrasound detection of diaphragmatic movement at follow-up had a median age at surgery of 1.4 years (range 8 days to 22.0 years). A total of 27 cases of diaphragmatic palsy were found, with unilateral palsy in 19 patients and bilateral palsy in four. Eleven plications were performed in these patients. Follow-up took place 5.3 years (median; range 3.0–12.6 years) after surgery and patients had a median age of 9.3 years (range 4.1–27.2 years) at follow-up.
Ultrasound examination showed an immobile diaphragm at the affected side in the majority of cases. No statistically significant differences in the movement at follow-up between plicated and non-plicated diaphragms were found (see Table 3).
Lung function testing
Patients with history of diaphragmatic palsy vs. control patients
No differences in the general patient characteristics, i.e. gender, age at surgery, age at follow-up and body weight, between patients with diaphragmatic impairment and the controls could be detected. Moreover, there were no differences in the number of patients in the two groups who had had previous operations or in the kind of thoracotomy (median or lateral) or the use of cardiopulmonary bypass.
Lung function analysis showed reduced lung function with lower values for vital capacity (VC) and forced expiratory volume in one second (FEV1) in the group of children with diaphragmatic palsy (independently of whether they had received plication or not) compared with the controls (Fig. 1a).
Except that patients with paralysis of the diaphragm have a higher residual lung volume (193 vs. 146 ml; p = 0.046) and a higher percentage of residual volume in relation to total lung capacity (199 vs. 148; p < 0.001), no differences could be found in total lung capacity or dead-space volume.
Patients with DP and plication vs. patients with DP and without plication
Among the patients with diaphragmatic palsy those who had needed diaphragmatic plication were significantly younger at time of surgery than those who managed without plication [median age 0.6 years (range 8 days to 8.7 years) vs. 9.6 years (range 314 days to 22 years; p = 0.012)], as has been reported previously [11]. At follow-up there were no statistically significant differences in terms of age, body weight or height between the two groups. In addition, the time between surgical intervention and follow-up showed no statistically significant difference, although the time interval was a little longer in patients who underwent plication of the paralysed diaphragm (6.5 vs. 5.3 years; p = 0.181).
For statistical analysis of lung function values 1 patient of the diaphragmatic plication group, who had persisting paradoxical movement of the plicated diaphragm, was excluded due to a lack of reliable lung function data. Taking into account gender, age at follow-up and body-mass index, no significant differences concerning the different lung function parameters could be found. Only for the parameter percent of predicted vital capacity (VC) and FEV1 were there slightly lower values in the plicated group (Fig. 1b). Due to the small number of patients in each group, this small difference needs to be verified in a larger group of patients.
Exercise testing
Comparison of patients with diaphragmatic palsy and control patients without history of diaphragmatic paralysis
Between patients with DP and the controls, no differences in general data, i.e. age at surgery, age at follow-up, body-mass index, kind of thoracotomy, the use of cardiopulmonary bypass or previous operations, could be detected. There was a difference in the distribution of the genders between patients with diaphragmatic palsy and the control group (male/female 6/9 vs. 55/25; p = 0.035); therefore, gender was taken into account as a cofactor in the subsequent statistical analysis. As in the evaluation of lung function, patients with DP and plication were significantly younger at surgery. These patients were younger at follow-up as well (10.7 vs. 18.1 years; p = 0.014). Due to their younger age, patients with DP and plication were smaller and weighed less at follow-up. No differences in the body-mass index could be found. In addition, the time interval between surgery and follow-up, although it was longer in patients who underwent plication, was not statistically significant (median 9.3 vs. 5.6 years; p = 0.15).
Patients with post-surgical diaphragmatic palsy showed a lower level of cardiopulmonary exercise capacity than control patients. There were significant differences between the two groups in the maximal power reached. Peak oxygen uptake (peak VO2) as a measure of maximal exercise capacity was significantly reduced in children with diaphragmatic palsy compared with controls (24.5 vs. 31.3 ml/kg min−1; p = 0.025).
The relation between ventilation and carbon dioxide production (VE/VCO2 slope) as the ventilatory response to exercise was significantly higher in patients with diaphragmatic impairment. Accordingly the minute volume (VE) as well as the tidal volume (VT) at peak exercise – as markers of the respiratory response to exercise – were significantly reduced in patients with DP, whereas there was no difference in baseline values. Although patients with DP showed higher respiratory rates at baseline (p = 0.039), at peak exercise no statistically significant difference could be detected (p = 0.291). No differences in oxygen pulse, as a non-invasive index for stroke volume, could be found (for all data see Table 4).
Patients with DP and plication vs. patients with DP and without plication
The comparison of children with and without diaphragmatic plication showed significant differences in age, body weight and height at follow-up. This is due to the fact that patients who required diaphragmatic plication were significantly younger at the initial operation. But taking these differences into account no differences in exercise capacity or peak oxygen uptake, VE/VCO2 slope, tidal (VT) and minute volume (VE) or respiratory rates between children with and without diaphragmatic plication could be found (Table 3).
Discussion
Phrenic nerve injury is a well-known clinical condition following cardiopulmonary bypass surgery [6, 19] and is an important risk factor in terms of morbidity during the postoperative period. Several studies have focused on the problems resulting from phrenic nerve damage, especially in infants and young children, such as prolonged hospital stay, prolonged mechanical ventilation and increased use of antibiotics [1, 8–11]. Diaphragmatic plication as described by Schwartz and Filler [14] and Shoemaker et al. [15] is performed to restore normal pulmonary parenchymal volume by restoring the diaphragm to its normal position [19] and has been shown to be effective in facilitating weaning from mechanical ventilation and shortening the post-operative course [1, 2, 7, 8, 11, 19–21]; however, the general value of diaphragmatic plication is controversial and its mid- and long-term results remain unknown.
Spontaneous recovery of diaphragmatic function has been described in rare cases [2, 22], but recovery itself and time to recovery cannot be predicted [7, 21, 23] – and recovery has been described even in patients after diaphragmatic plication [2, 19]. Looking at recovery of phrenic nerve function in our patient cohort we found normal diaphragmatic movement indicating recovery of phrenic nerve function in only one-third of cases, whereas the majority of paralysed diaphragms remained paralysed, regardless of whether plication was performed or not (Table 2). Although we did not perform any nerve-conduction studies in our patients, these data support the hypothesis that even after diaphragmatic plication there is a potential for recovery of the phrenic nerve.
Kizilcan et al. [19] evaluated 12 patients with diaphragmatic plication after congenital diaphragmatic eventration in terms of diaphragmatic movement and lung function, and found vital capacity and FEV1 values within the normal range in five of six patients; however, other groups have shown a restrictive ventilatory pattern in patients with unilateral diaphragmatic paralysis [16, 24, 25]. Whereas a mild to moderate restrictive lung function pattern has been described for patients after repair of more complex congenital heart disease, depending on the complexity of congenital heart disease and surgical outcome [26–30], we found an even more restrictive ventilatory pattern in our patients with a history of diaphragmatic palsy compared with our controls. But there was no clear statistically significant difference in lung function values in the comparison between patients with and without plication, even if in the small group of patients with diaphragmatic plication there was a tendency towards lower VC and FEV1 values. Due to the small number of patients with diaphragmatic palsy who were followed up by lung function testing, this difference seems to represent only a trend and has to be investigated in a larger patient cohort. Since FEV and peak VO2 are linearly related, a reduction in FEV should affect maximal work capacity as well. For children who have undergone repair of more complex congenital heart disease, a significantly impaired mean normalized maximal performance has been described [31]. In our cohort of patients with diaphragmatic palsy no differences in the resting values – besides a higher breathing rate – could be found, but, as expected, we found lower cardiopulmonary exercise capacity as well as lower values for peak VO2 and a higher VE/VCO2 slope as the ventilatory response to exercise in children with a history of diaphragmatic palsy. Additionally, at peak exercise children with DP had lower minute ventilation; therefore, one might suggest that at rest patients with diaphragmatic impairment can compensate a lower vital capacity by a higher breathing rate, but at peak exercise this mechanism of compensation no longer copes. As seen for recovery of the phrenic nerve and lung function testing, no differences in cardiopulmonary exercise testing could be found for children with and without diaphragmatic plication.
A limitation of this study is the relatively long time period between surgery and plication, which is due to the rare experience of plication at our centre and controversial opinions concerning the benefit of diaphragmatic plication in the 1980s and 1990s. Diaphragmatic plication is presently performed much earlier to prevent irreversible lung damage due to prolonged ventilation or chronic atelectasis. In addition, we have learned that in children with univentricular circulation diaphragmatic palsy is a risk factor for suboptimal Fontan hemodynamics, as described previously [17]. Having recognized this, we performed plication after 2003 in three of the patients with TCPC followed up in this study; therefore, the outcome – in terms of lung function and exercise capacity – after plication may be even better in patients who undergo plication early after initial surgery. Furthermore, as a routine check-up for diaphragmatic paralysis in our centre was not started until 1996, we cannot exclude the possibility that there might be a patient with clinically unapparent diaphragmatic paralysis in the control group, because the latter was formed retrospectively from among patients in whom all the procedures were performed.
Conclusion
In conclusion, we state that it is generally important to raise the issue of primary intraoperative prevention of damage to the phrenic nerve and to consider intraoperative phrenic nerve latency monitoring, which has been shown to be effective in adults [32–35]. At the same time, a high degree of awareness in the postoperative period is necessary to prevent further morbidity by diagnosing and treating diaphragmatic impairment and selecting the patients for plication. Plication seems to be without mid-term risk in terms of recovery of phrenic nerve function, lung function values and exercise capacity; however, it seems that it does not provide general benefit to patients with diaphragmatic impairment and it should therefore not be performed routinely in all patients (except in patients with total cavopulmonary connection) [11, 36].
References
Tonz M, Segesser LK von, Mihaljevic T, Arbenz U, Stauffer UG, Turina MI (1996) Clinical implications of phrenic nerve injury after pediatric cardiac surgery. J Pediatr Surg 31:1265–1267
van Onna IE, Metz R, Jekel L, Woolley SR, van de Wal HJ (1998) Post cardiac surgery phrenic nerve palsy: value of plication and potential for recovery. Eur J Cardiothorac Surg 14:179–184
Kunovsky P, Gibson GA, Pollock JC, Stejskal L, Houston A, Jamieson MP (1993) Management of postoperative paralysis of diaphragm in infants and children. Eur J Cardiothorac Surg 7:342–346
Russell RI, Helps BA, Dicks-Mireaux CM, Helms PJ (1993) Early assessment of diaphragmatic dysfunction in children in the ITU: chest radiology and phrenic nerve stimulation. Eur Respir J 6:1336–1339
Glassman LR, Spencer FC, Baumann FG, Admas FV, Colvin SB (1994) Successful plication for postoperative diaphragmatic paralysis in an adult. Ann Thorac Surg 58:1754–1755, 1757–1758
Wright CD, Williams JG, Ogilvie CM, Donnelly RJ (1985) Results of diaphragmatic plication for unilateral diaphragmatic paralysis. J Thorac Cardiovasc Surg 90:195–198
Watanabe T, Trusler GA, Williams WG, Edmonds JF, Coles JG, Hosokawa Y (1987) Phrenic nerve paralysis after pediatric cardiac surgery. Retrospective study of 125 cases. J Thorac Cardiovasc Surg 94:383–388
Takeda S, Nakahara K, Fujii Y, Matsumura A, Minami M, Matsuda H (1995) Effects of diaphragmatic plication on respiratory mechanics in dogs with unilateral and bilateral phrenic nerve paralyses. Chest 107:798–804
Marcos JJ, Grover FL, Trinkle JK (1974) Paralyzed diaphragm: effect of plication on respiratory mechanics. J Surg Res 16:523–526
Muller NL, Bryan AC (1979) Chest wall mechanics and respiratory muscles in infants. Pediatr Clin North Am 26:503–516
Lemmer J, Stiller B, Heise G, Hübler M, Alexi-Meskishvili V, Weng Y, Redlin M, Amnn V, Ovroutski S, Berger F (2006) Postoperative phrenic nerve palsy: early clinical implications and management. Intensive Care Med 32:1227–1233
Affatato A, Villagra F, Leon JP de, Gomez R, Checa SL, Vellibre D, Sanchez P, Diez Balda JI, Brito JM (1988) Phrenic nerve paralysis following pediatric cardiac surgery. Role of diaphragmatic plication. J Cardiovasc Surg (Torino) 29:606–609
Hamilton JR, Tocewicz K, Elliott MJ, de Leval M, Stark J (1990) Paralysed diaphragm after cardiac surgery in children: value of plication. Eur J Cardiothorac Surg 4:487–491
Schwartz MZ, Filler RM (1978) Plication of the diaphragm for symptomatic phrenic nerve paralysis. J Pediatr Surg 13:259–263
Shoemaker R, Palmer G, Brown JW, King H (1981) Aggressive treatment of acquired phrenic nerve paralysis in infants and small children. Ann Thorac Surg 32:250–259
Ciccolella DE, Daly BD, Celli BR (1992) Improved diaphragmatic function after surgical plication for unilateral diaphragmatic paralysis. Am Rev Respir Dis 146:797–799
Ovroutski S, Alexi-Meskishvili V, Stiller B, Ewert P, Abdul-Khaliq H, Lemmer J, Lange PE, Hetzer R (2005) Paralysis of the phrenic nerve as a risk factor for suboptimal Fontan hemodynamics. Eur J Cardiothorac Surg 27:561–565
Jones NL (1988) Clinical exercise testing, 3rd edn. Saunders, Philadelphia
Kizilcan F, Tanyel FC, Hicsonmez A, Buyukpamukcu N (1993) The long-term results of diaphragmatic plication. J Pediatr Surg 28:42–44
Serraf A, Planche C, Lacour Gayet F, Bruniaux J, Nottin R, Binet JP (1990) Post cardiac surgery phrenic nerve palsy in pediatric patients. Eur J Cardiothorac Surg 4:421–424
de Leeuw M, Williams JM, Freedom RM, Williams WG, Shemie SD, McCrindle BW (1999) Impact of diaphragmatic paralysis after cardiothoracic surgery in children. J Thorac Cardiovasc Surg 118:510–517
Dagan O, Nimri R, Katz Y, Birk E, Vidne B (2006) Bilateral diaphragm paralysis following cardiac surgery in children: 10–years' experience. Intensive Care Med 32:1222–1226
Iverson LI, Mittal A, Dugan DJ, Samson PC (1976) Injuries to the phrenic nerve resulting in diaphragmatic paralysis with special reference to stretch trauma. Am J Surg 132:263–269
Hillman DR, Finucane KE (1988) Respiratory pressure partitioning during quiet inspiration in unilateral and bilateral diaphragmatic weakness. Am Rev Respir Dis 137:1401–1405
Wilcox PG, Pare PD, Pardy RL (1990) Recovery after unilateral phrenic injury associated with coronary artery revascularization. Chest 98:661–666
Lubica H (1996) Pathologic lung function in children and adolescents with congenital heart defects. Pediatr Cardiol 17:314–315
Wessel HU, Weiner MD, Paul MH, Bastanier CK (1981) Lung function in tetralogy of Fallot after intracardiac repair. J Thorac Cardiovasc Surg 82:616–628
Strieder DJ, Aziz K, Zaver AG, Fellows KE (1975) Exercise tolerance after repair of tetralogy of Fallot. Ann Thorac Surg 19:397–405
Strieder DJ, Mesko ZG, Aziz K (1974) Respiratory control and exercise ventilation in tetralogy of fallot. Acta Paediatr Belg 28(Suppl):162–168
Samanek M, Sulc J, Zapletal A (1989) Lung function in simple complete transposition after intracardiac repair. Int J Cardiol 24:13–17
Norozi K, Gravenhorst V, Hobbiebrunken E, Wessel A (2005) Normality of cardiopulmonary capacity in children operated on to correct congenital heart defects. Arch Pediatr Adolesc Med 159:1063–1068
Mazzoni M, Solinas C, Sisillo E, Bortone F, Susini G (1996) Intraoperative phrenic nerve monitoring in cardiac surgery. Chest 109:1455–1460
Canbaz S, Turgut N, Halici U, Balci K, Ege T, Duran E (2004) Electrophysiological evaluation of phrenic nerve injury during cardiac surger: a prospective, controlled, clinical study. BMC Surg 4:2
Avila JM, Peiffert B, Maureira JJ, Amrein D, Villemot JP, Mathieu P (1991) Reduction in the incidence of postoperative diaphragmatic paralysis by using a phrenic nerve protector. Article in French. Ann Chir 45:689–691
Esposito RA, Spencer FC (1987) The effect of pericardial insulation on hypothermic phrenic nerve injury during open–heart surgery. Ann Thorac Surg 43:303–308
Amin Z, McElhinney DB, Strawn JK, Kugler JD, Duncan KF, Reddy VM, Petrossian E, Hanley FL (2001) Hemidiaphragmatic paralysis increases postoperative morbidity after a modified Fontan operation. J Thorac Cardiovasc Surg 122:856–862
Acknowledgements
We thank A.M. Gale, ELS, for editorial assistance and B. Peters, University of Magdeburg, for statistical assistance. This work was supported by the Kompetenznetz Angeborene Herzfehler (Competence Network for Congenital Heart Defects) funded by the Federal Ministry of Education and Research (BMBF), FKZ01G10210.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lemmer, J., Stiller, B., Heise, G. et al. Mid-term follow-up in patients with diaphragmatic plication after surgery for congenital heart disease. Intensive Care Med 33, 1985–1992 (2007). https://doi.org/10.1007/s00134-007-0717-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0717-9