Abstract
Objective
To evaluate the effect of the 4G/5G PAI-1 gene polymorphism on the development of organ failure and outcome in critically ill patients with septic syndromes.
Design and setting
Prospective, observational study in a medical intensive care unit of a university hospital.
Patients
224 consecutively admitted patients.
Interventions
Epidemiological data, severity scores, and the primary site of infection were recorded. DNA genotyping of the PAI-1, TNF-β, and IL1-ra genes, and measurement of plasma PAI-1 antigen and D-dimer were carried out.
Measurements
The primary outcome variables were organ dysfunction and mortality.
Results
Eighty-eight subjects had septic shock at ICU entry or within 48 h from admission. Homozygotes for the 4G allele exhibited higher plasma concentrations of PAI-1 antigen and D-dimer than 4G/5G and 5G/5G subjects). ICU mortality was 44.0% in patients with 4G/4G, 23.4% in 4G/5G and 12.5% in 5G/5G, mainly due to multiorgan failure. After adjusting for SAPS II at admission the genotypes independently associated with ICU mortality in septic shock were TNF-B2/B2 (OR 2.83, 1.04–7.67) and 4G/4G of PAI-1 (OR 2.23, 1.02–4.85). The PAI-1 genotype did not determine susceptibility to infection or the outcome in nonseptic systemic inflammatory response syndrome, sepsis, severe sepsis, and nosocomial septic shock.
Conclusions
Homozygosity for 4G of the PAI-1 gene confers an increase in the risk of mortality in adult patients with septic shock due to a greater organ failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is the leading cause of death in critically ill patients, with a hospital mortality ranging from 30% to 50% in patients with septic shock [1, 2]. Epidemiological studies on inflammatory mediators have suggested a strong genetic relationship on the susceptibility and outcome of sepsis. TNF-α-308A and TNF-β-252A polymorphisms have been reported to be associated with susceptibility to meningococcal disease [3] and a high risk for septic shock in patients admitted with community-acquired pneumonia [4], respectively. Regarding the risk of mortality Mira et al. [5] found that the TNF-α-308A allele had a 3.7-fold increase in death among septic shock patients whereas homozygosity for B2/B2 of TNF-β, which has been associated with a high tumor necrosis factor (TNF) response, increases the probability of severe posttraumatic sepsis in trauma by 3.4 [6]. With regard to the interleukin (IL) 1 pathway, the IL-1raA2 allele seems to be more prevalent among patients with severe sepsis than among healthy individuals [7].
Inflammation and coagulation are closely linked and most patients with severe sepsis and septic shock have coagulation abnormalities [8]. In this setting nonsurvivors present a particular hemostatic profile characterized by a marked activation of coagulation and a more intense inhibition of fibrinolysis [9, 10]. TNF-α and IL-1 increase the synthesis and release from endothelial cells of plasminogen activator inhibitor 1 (PAI-1), a key inhibitor of fibrinolysis and also decrease plasminogen activator synthesis [11, 12]. Thus, impaired fibrin degradation due to high circulating levels of PAI-1 may contribute to enhanced microvascular fibrin deposition, which favors the development of organ dysfunction [13]. PAI-1 may show a genomic variation in its promoter: a single base-pair deletion (4G) or insertion (5G). Homozygosity for the 4G allele is reported to have higher basal and inducible concentrations of PAI-1 and greater procoagulatory activity than one or two copies of the 5G allele [14]. This has been associated with an increased risk of death from meningococcal sepsis in children [15–17] and a poor survival after severe trauma [18]. On the other hand, the G4 variant of the PAI-1 gene seems to be associated with a weak increase to the risk of coronary disease [19], and G4/G4 genotype is associated with an increase in thromboembolic neurological complications after cardiac surgery [20]. Moreover, several reports claim for an involvement of the G4 variant in a miscellany of other cardiovascular [21], and systemic diseases [22–24], although these studies need confirmatory evidence.
The aim of the study was to evaluate the effect of the 4G/5G PAI-1 gene polymorphism in the development of organ failure and outcome in adult patients with septic shock. In addition, we evaluated the association of genomic variations in TNF-β and IL1-ra on the influencing the PAI-1 4G/4G gene effect on the primary endpoints.
Patients and methods
Patients
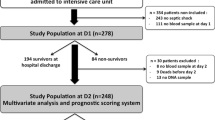
During the 12-month period from January 2003 to January 2004, 301 patients were admitted to the medical ICU of the Hospital Clinic of Barcelona. The study population consisted of 224 consecutively patients (mean age 62.3 ± 15.9 years, range 18–85; 63.8% men) with a minimum ICU stay of 48 h and without short-term irreversible diseases, as reported in the Electronic Supplementary Material (ESM; Fig. 1). The patients were included and followed until hospital discharge. Furthermore, 80 healthy blood donors recruited consecutively were used as the control population. All the subjects were of white descent and living in or around Barcelona. Informed consent was obtained from the patients or their relatives within 24 h after admission, and none refused to participate. The protocol was approved by the institutional review board of the Hospital Clinic of Barcelona.
Epidemiological data, the primary site of infection, and infection-related organisms were recorded (Table 1 and ESM). Clinical infections were defined according to the Centers for Diseases Control and Prevention criteria [25]. Severe sepsis and septic shock were defined according to SCCM/ESICM/ACCP/ATS/SIS consensus conference [26], as described in the ESM. Septic shock was considered nosocomial (late) when observed after 48 h after ICU entry. Severity indexes including Acute Physiology and Chronic Health Evaluation (APACHE) II, Simplified Acute Physiology Score (SAPS) II, and Sequential Organ Failure Assessment (SOFA) were calculated at ICU admission and thereafter on a daily basis. Within 48 h of ICU entry 88 patients exhibited septic shock and 26 severe sepsis (Fig. 1); of the remaining patients 51 had sepsis and 59 had noninfectious systemic inflammatory response syndrome (SIRS). Mean APACHE II, SAPS II, and SOFA scores at entry were 16.8 ± 6.3, 37.4 ± 12.3, and 8.6 ± 3.1 at ICU entry, respectively. Multiorgan failure was considered in case of acute progressive dysfunction of two or more organs systems, with a minimum failure score of 3 points for each organ. Acute respiratory distress syndrome was considered according to the European Consensus score [27], with patients showing a Murray et al. [28] score of 2.5 or higher. Blood samples and the information used in the study were coded and patient confidentiality was preserved. Biochemical studies and genotyping were performed in the patients after completion of follow-up. Patients with septic shock required surgery more frequently than patients with sepsis. Coagulation parameters at ICU entry did not differ among the groups of patients, except for greater fibrinogen levels in septic subjects than in those with noninfectious SIRS (Table 1).
Biochemical and genotype studies
Collection of venous blood samples and processing are reported in ESM. Prothrombin and activated partial thromboplastin times, fibrinogen, and D-dimer levels were measured [29]. Plasma antigen related to PAI-1 was measured by an enzyme-linked immunosorbent assay (Biopool, Umea, Sweden) based on a double-antibody principle [30]. Genomic DNA was extracted from 100 μl whole blood with a silica gel column method (QIAamp DNA blood mini kit, Qiagen, Hilden, Germany), and stored at −80 °C until further use. Genotyping was validated by direct sequencing of a group of random samples. We determined the PAI-1 4G/5G, TNF-β-252G B1/B2, and IL-1ra A2 polymorphisms [31–33], and methods for detection are shown in the ESM.
Statistical analysis
Results are given as means ± SD. Differences between groups were evaluated with the Fisher's exact and Student's t tests. Bonferroni's correction was applied to adjust the type I error in multiple comparisons. Pearson's correlation coefficients between continuous variables were calculated. Genotype distributions were tested for the Hardy-Weinberg equilibrium. To evaluate the variables independently associated with ICU and hospital mortality a logistic regression model (forward stepwise selection) was performed. In this model quantitative variables were introduced in its continuous form, and therefore the odds are referred to the natural unit of the predictor. All tests were performed with a bilateral significance level of p < 0.05. Statistical analysis was performed with SPSS statistical software (version 11.0.4; SPSS, Chicago, Ill., USA).
Results
Patient follow-up data
Data on the patients during ICU stay are summarized in Table 2. Patients with septic shock showed a significantly greater worsening in SAPS II score than those admitted because of sepsis or noninfectious SIRS. Thirty-two (14.3%) patients died in the ICU, mainly due to multiorgan failure. Mortality was higher in those with septic shock (27.3 vs. 5.8%, p < 0.001). Overall hospital mortality reached 20.1%, with higher post-ICU ward mortality in patients admitted for nonseptic SIRS (12.5 vs. 3.6%, p < 0.001). Logistic multivariate analysis showed that the clinical variables independently associated with ICU mortality in patients admitted with septic shock were the SAPS II score at admission [odds ratio (OR) 1.08, 95% confidence interval (CI) 1.02–1.15) and the worsening of this score during ICU stay (1.16, 1.09–1.24). Moreover, 14 patients (range between the groups 3.4–11.5%) developed nosocomial septic shock while in the ICU.
Genetic analysis
The distribution of the PAI-1 genotype was comparable in patients and controls and between the different subgroups of patients studied (Table 3). Likewise the overall allele frequency of 4G/5G was 0.49/0.51 in all patients, which did not differ from that observed in controls (0.54/0.46). Regarding the TNF-β genotype, homozygosity for the B2 allele was more prevalent in patients with septic shock than in controls (61.3 vs. 45.0%, p = 0.04). By contrast, the distribution of the IL1-ra genotype among the groups of patients did not differ from that of the healthy population. In patients with septic syndromes PAI-1 alleles distributed evenly with TNF-β and IL-1ra alleles (Table 4). Except for the higher prevalence of homozygosity for the B2 allele in patients admitted with septic shock, none of the genotypes analyzed was associated with diseases leading to ICU entry or the origin of infectious disease.
Coagulation abnormalities in organ dysfunction and septic shock
Plasma levels of the PAI-1 antigen on admission were correlated with the Δ SOFA score (r = 0.28, p = 0.02) and were greater in patients who died than in survivors (45.3 ± 23.8 vs. 33.8 ± 16.7 ng/ml, respectively, p = 0.02). The 4G/4G patients with septic shock had higher plasma concentrations of the PAI-1 antigen than 4G/5G and 5G/5G subjects (p < 0.001, both; Table 5). Coagulation data at ICU entry were not related to the PAI-1 genotype. However, 4G/4G patients showed a twice the D-dimer concentration of those with other PAI-1 genotypes (p < 0.05, both; Table 5). D-dimer levels at ICU entry were not correlated significantly with the SOFA score, but were also greater in patients with septic shock who died than in survivors (826 ± 919 vs. 513 ± 423 ng/ml, respectively, p = 0.03). A direct correlation between the PAI-1 antigen and D-dimer upon ICU admission was observed (r = 0.49, p < 0.001).
Effect of TNF-β and IL-1ra genotypes on organ dysfunction and mortality
We found no differences in severity scores with respect to baseline values and changes during ICU stay among the groups of patients homozygous to the B2/B2 compared to other forms of the TNF-β gene (data not shown). However, the mortality of B2/B2 patients with septic shock was higher than that in patients carriers of the B1 allele (37.0 vs. 11.7%, respectively, p = 0.01). Mortality was not associated with the TNF-β polymorphism in the remaining groups of patients. On the other hand, neither was the IL1-ra genotype related to susceptibility to infection, clinical data or outcome in any group of the patients studied. Neither of these two genotypes was associated with the appearance of late (nosocomial) septic shock and survival.
Effect of the PAI-1 genotype on organ dysfunction and mortality
The PAI-1 genotype affected the clinical course of patients with septic shock, as 4G homozygotes exhibited a greater worsening in clinical status (i.e., Δ SOFA) than other PAI-1 genotypes (p < 0.05, all; Table 5). The presence of 4G/4G in patients with septic shock was associated with an increase of 1 point in the SOFA score (OR 2.83, 95% CI 1.04–7.67). However, nonsignificantly greater supportive measures (i.e., mechanical ventilation, vasopressors administration, parenteral nutrition) were needed by the 4G/4G patients. Clinical changes in the patients admitted for severe sepsis, sepsis, or noninfectious SIRS were independent of PAI-1 genotype.
ICU mortality in septic shock reached 44.0% in patients with 4G/4G, 23.4% with 4G/5G, and 12.5% in 5G/5G (p = 0.03 for 4G/4G vs. other genotypes; Fig. 2), mostly due to multiorgan failure. The 4G and 5G allele distribution was 0.50/0.50 in alive and 0.69/0.31 in nonsurvivors (p = 0.03). After adjusting for SAPS II at admission the genotypes independently associated with ICU mortality in septic shock were of TNF-B2/B2 (OR 2.83, 95% CI 1.04–7.67) and 4G/4G of PAI-1 (2.23, 1.02–4.85). Taking all the genotypes into consideration, we observed that 37.7% of the subjects with septic shock carrying 4G/4G or B2/B2 died, whereas the mortality decreased to 3.7% when both these polymorphisms were absent (p < 0.001). No additive effect on mortality was observed between the genotypes. The 4G allele of the PAI-1 gene was not related to the appearance of nosocomial septic shock and its mortality, although the number of patients evaluated was too small.
Discussion
In the present study we observed greater organ dysfunction and a twofold increase in the risk of mortality in patients with septic shock who were homozygous for the 4G-deletion polymorphism of the PAI-1 gene. In addition, similarly to previously published studies [6, 34], we observed that B2/B2 of the TNF-β gene confers a higher susceptibility to septic shock and these subjects have a worse outcome. Moreover, we confirmed the lack of association between the genomic variations in PAI-1, TNF-β, and IL-1ra with each other. The study was underpowered to identify a clinical significant difference in the supportive case among the groups of patients.
It is already known that virtually all patients with sepsis have coagulation abnormalities, with widespread microvascular fibrin deposition, which contributes to organ dysfunction and profuse bleeding from various sites [35]. Inhibition of the fibrinolytic system is a key element of the pathogenesis of fibrin deposition during severe inflammation. In sepsis-induced generalized activation of coagulation the generation of thrombin also initiates fibrinolysis through the release of tissue plasminogen activator. However, the activation of the fibrinolytic system is transient due to a strongly proinflammatory cytokine-induced PAI-1 expression and secretion by endothelial cells [36, 37]. Thus the net result is a proinflammatory and prothrombotic disorder with exhaustion of fibrinolysis and coagulation inhibitors [38]. In agreement with previous findings [39] we found that both plasma PAI-1 and D-dimer were elevated in patients with septic shock, mainly in those who died, and was correlated with the first to organ failure.
In addition to proinflammatory cytokines, the circulating plasma PAI-1 level is affected by a deletion/insertion (4G/5G) polymorphism in the promoter of the PAI-1 gene. Although both alleles bind a transcriptional activator, only the 5G allele binds a repressor protein at an overlapping site. Therefore homozygosity for the 4G allele renders this negative regulator unable to bind, resulting in greater transcription of the PAI-1 gene [9, 11, 14]. In this regard we documented that plasma PAI-1 concentrations in 4G homozygotes doubled than that observed in 5G carriers. As this increase in PAI-1 may show circadian changes [40], we determined the PAI-1 antigen from morning samples. Previous studies have shown that homozygosity for the 4G allele of the PAI-1 gene exerts a harmful effect on the prognosis of some subsets of critical patients, such as children with meningococcal sepsis, in whom the relative risk of dying from meningococcal sepsis increases from 2.0 to 2.4 compared with 5G carriers [15, 17]. In these patients logistical regression indicated a 40% reduction in the probability of death for 4G/5G patients and a 91% reduction for 5G/5G patients compared to 4G homozygotes [15]. Moreover, in patients with severe trauma, Menges et al. [18] found that the 4G allele not only has increased levels of PAI-1 during 14 days of observation after multiple traumas but also entailed a higher prevalence of sepsis and multiple organ failure. As a result 11 of 19 patients with the 4G/4G genotype did not survive, whereas only 8 of the 29 4G/5G patients, and 2 of 13 patients with 5G/5G of the PAI-1 gene died. No studies have yet determined the effect of the PAI-1 genotype in adult patients with septic shock of different origin. In the present study we observed that patients with septic shock without unsalvageable disease resulted in a hospital mortality of 52.0% for 4G/4G, 27.7% for 4G/5G and 18.8% for 5G/5G patients, mainly due to multiorgan failure. This association with PAI-1 gene polymorphism occurred independently of the causative infectious pathogen and was not observed in patients with sepsis and severe sepsis or in those with late (nosocomial) septic shock. However, this study has some limitations due to number of subjects and power of calculation, as well as derived from the complexity of the disease [41], and these initial positive findings needs to be confirmed in a large independent cohort in order to verify that the genetic background or environmental exposures did not affect the results. The G4 variant of the PAI-1 gene has also been implicated in many other diseases [42–49], as is reported in ESM.
On the other hand, in the present study we evaluated other genotypes that coded for the production of TNF-α and IL-1ra and found septic shock to be more prevalent in patients homozygous for the TNF-B2/B2 polymorphism. However, in contrast to the report by Fang et al. [7], the prevalence of IL-1raA2 among patients with severe sepsis and septic shock did not differ from that observed in healthy individuals. More importantly, TNF-B2/B2 was associated with a 2.8-fold increase in the risk of mortality in patients with septic shock. Other candidate genes which regulate the inflammatory response and which may be implicated in the appearance and end result of septic shock are those that code for the heat shock protein, IL-6, IL-10, CD-14, and Toll-like receptors [50], were not evaluated in the present study.
In summary, we observed that patients admitted to the ICU with septic shock had greater organ dysfunction and exhibited a higher mortality when homozygous to the 4G form of the PAI-1 gene. This observation may be related to a procoagulant state in sepsis, as a consequence of fibrinolysis inhibition by PAI-1. However, the evidence from this single association study needs to be replicated to provide insurance against errors and biases. In addition, further studies of combined gene effects and gene-gene interactions as well as therapeutic approaches based on genetic risk in patients with both sepsis and a derangement of coagulation are needed.
References
Angus D, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348:1546–1554
Nadel S, Newport MJ, Boody Booy R, Levin M (1996) Variation in the tumor necrosis factor-alpha gene promoter region may be associated with death from meningococcal disease. J Infect Dis 174:878–880
Waterer GW, Quasney MW, Cantor RM, Wunderink RG (2001) Septic shock and respiratory failure in community-acquired pneumonia have different TNF polymorphism associations. Am J Respir Crit Care Med 163:1599–1604
Mira JP, Cariou A, Grall F, Delclaux C, Losser MR, Heshmati F, Cheval C, Monchi M, Teboul JL, Riche F, Leleu G, Arbibe L, Mignon A, Delpech M, Dhainaut JF (1999) Association of TNF2, a TNF-alpha promoter polymorphism, with septic shock susceptibility and mortality: a multicenter study. JAMA 282:561–568
Majetschak M, Flohe S, Obertacke U, Schroder J, Staubach K, Nast-Kolb D, Schade FU, Stuber F (1999) Relation of a TNF gene polymorphism to severe sepsis in trauma patients. Ann Surg 230:207–214
Fang XM, Schroder S, Hoeft A, Stuber F (1999) Comparison of two polymorphisms of the interleukin-1 gene family: interleukin-1 receptor antagonist polymorphism contributes to susceptibility to severe sepsis. Crit Care Med 27:1330–1334
Dellinger RP (2003) Inflammation and coagulation: implications for the septic patient. Clin Infect Dis 36:1259–1265
Kornelisse RF, Hazelzet JA, Savelkoul HFJ, Hop WC, Suur MH, Borsboom AN, Risseeuw-Appel IM, van der Voort E, de Groot R (1996) The relationship between plasminogen activator inhibitor-1 and proinflammatory and counter-inflammatory mediators in children with meningoccocal septic shock. J Infect Dis 173:1148–1156
Vervloet MG, Thijs LG, Hack CE (1998) Derangements of coagulation and fibrinolysis in critically ill patients with sepsis and septic shock. Semin Thromb Hemost 24:33–44
Mesters RM, Florke N, Ostermann H, Kienast J (1996) Increase of plasminogen activator inhibitor levels predicts outcome of leukopenic patients with sepsis. Thromb Haemost 75:902–907
Ryan MP, Kutz SM, Higgins PJ (1996) Complex regulation of plasminogen activator inhibitor type-1 (PAI-1) gene expression by serum and substrate adhesion. Biochem J 314:1041–1046
Horrevoets JG (2004) Plasminogen activator inhibitor 1 (PAI-1): in vitro activities and clinical relevance. Br J Haematol 125:12–23
Dawson SJ, Wiman B, Hamsten A, Green F, Humphries S, Henney AM (1993) The two allele sequences of a common polymorphism in the promoter of the plasminogen activator inhibitor-1 (PAI-1) gene respond differently to interleukin-1 in HepG2 cells. J Biol Chem 268:10739–10745
Hermans PW, Hibberd ML, Booy R, Daramola O, Hazelzet JA, de Groot R, Levin M (1999) 4G/5G promoter polymorphism in the plasminogen-activator-inhibitor-1 gene and outcome of meningococcal disease. Meningococcal Research Group. Lancet 354:556–560
Westendorp RG, Hottenga JJ, Slagboom PE (1999) Variation in plasminogen-activator-inhibitor-1 gene and risk of meningococcal septic shock. Lancet 354:561–563
Haralambous E, Hibberd ML, Hermans PW, Ninis N, Nadel S, Levin M (2003) Role of functional plasminogen-activator-inhibitor-1 4G/5G promoter polymorphism in susceptibility, severity, and outcome of meningococcal disease in Caucasian children. Crit Care Med 31:2788–2793
Menges T, Hermans PW, Little SG, Langefeld T, Boning O, Engel J, Sluijter M, de Groot R, Hempelmann G (2001) Plasminogen-activator-inhibitor-1 4G/5G promoter polymorphism and prognosis of severely injured patients. Lancet 357:1096–1097
Ye Z, Liu EH, Higgins JP, Keavney BD, Lowe GD, Collins R, Danesh J (2006) Seven haemostatic gene polymorphisms in coronary disease: meta-analysis of 66:155 cases and 91:307 controls. Lancet 367:651–658
Sirgo G, Perez-Vela JL, Morales P, Del Rey M, Vendrell J, Gutierrez C, Rello J (2006) Association between 4G/5G polymorphism of the plasminogen activator inhibitor 1 gene with stroke or encephalopathy alter cardiac surgery. Intensive Care Med 32:668–675
Wiklund PG, Nilsson L, Ardnor SN, Eriksson P, Johansson L, Stegmayr B, Hamsten A, Holmberg D, Asplund K (2005) Plasminogen activator inhibitor-1 4G/5G polymorphism and risk of stroke: replicated findings in two nested case-control studies based on independent cohorts. Stroke 36:1661–1665
Castello R, Espana F, Vazquez C, Fuster C, Almenar SM, Aznar J, Estelles A (2006) Plasminogen activator inhibitor-1 4G/5G polymorphism in breast cancer patients and its association with tissue PAI-1 levels and tumor severity. Thromb Res 117:487–492
Hizawa N, Maeda Y, Konno S, Fukui Y, Takahashi D, Nishimura M (2006) Genetic polymorphisms at FCER1B and PAI-1 and asthma susceptibility. Clin Exp Allergy 36:872–876
Glueck CJ, Sieve L, Zhu B, Wang P (2006) Plasminogen activator inhibitor activity, 4G5G polymorphism of the plasminogen activator inhibitor 1 gene, and first-trimester miscarriage in women with polycystic ovary syndrome. Metabolism 55:345–352
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections. Am J Infect Control 16:128–140
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, for the International Sepsis Definitions Conference (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 139:720–723
Reber G, Bounameaux H, Perrier A, de Moerloose P (2001) Performances of a new, automated latex assay for the exclusion of venous thromboembolism. Blood Coagul Fibrinolysis 12:217–220
Declerck PJ (1988) Measurement of plasminogen activator inhibitor 1 in biological fluids with a murine monoclonal antibody-based enzyme-linked immuno-sorbant assay. Blood 71:220–225
Margaglione M, Grandone E, Cappucci G, Colaizzo D, Giuliani N, Vecchione G, d'Addedda M, Di Minno G (1997) An alternative method for PAI-1 promoter polymorphism (4G/5G) typing. Thromb Haemost 77:605–606
Schaaf BM, Seitzer U, Pravica V, Aries SP, Zabel P (2001) Tumor Necrosis Factor-a-308 promoter gene polymorphism and increased tumor necrosis factor serum bioactivity in farmer's lung patients. Am J Respir Crit Care Med 163:379–382
Tarlow JK, Blakemore AIF, Lennard A, Solari R, Hughes HN, Steinkasserer A, Duff GW (1993) Polymorphism in human IL-1 receptor antagonist gene intron 2 is caused by variable number of an 86-bp tandem repeat. Hum Genet 91:403–404
Stuber F, Petersen M, Bokelmann F, Schade U (1996) A genomic polymorphism within the tumor necrosis factor locus influences plasma tumor necrosis factor-alpha concentrations and outcome of patients with severe sepsis. Crit Care Med 24:381–384
Dempfle CE (2004) Coagulopathy in sepsis. Thromb Haemost 91:213–224
Levi M, Ten Cate H (1999) Disseminated intravascular coagulation. N Engl J Med 341:586–592
Dhainaut JF, Shorr AF, Macias WL, Kollef MJ, Levi M, Reinhart K, Nelson DR (2005) Dynamic evolution of coagulopathy in the first day of severe sepsis: relationship with mortality and organ failure. Crit Care Med 33:341–348
Mavrommatis AC, Theodoridis T, Economou M, Kotanidou A, El Ali M, Christopoulou-Kokkinou V, Zakynthinos SG (2001) Activation of the fibrinolytic system and utilization of the coagulation inhibitors in sepsis: comparison with severe sepsis and septic shock. Intensive Care Med 27:1853–1859
Okabayashi K, Wada H, Ohta S, Shiku H, Nobori T, Maruyama K (2004) Hemostatic markers and the sepsis-related organ failure assessment score in patients with disseminated intravascular coagulation in an intensive care unit. Am J Hematol 76:225–229
Hoekstra T, Geleijnse JM, Schouten EG, Kluft C (2002) Diurnal variation in PAI-1 activity predominantly confined to the 4G-allele of the PAI-1 gene. Thromb Haemost 88:794–798
Hattersley AT, McCarthy MI (2005) What makes a good genetic association study? Lancet 366:1315–1323
Boekholdt SM, Bjisterveld NR, Moons AH, Levi M, Buller HR, Peters RJ (2001) Genetic variation in coagulation and fibrinolytic proteins and their relation with acute myocardial infarction: a systematic review. Circulation 104:3063–3068
Ding J, Nicklas BJ, Fallin MD, de Rekeneire N, Kritchevsky SB, Pahor M, Rodondi N, Li R, Zmuda JM, Harris TB (2006) Plasminogen activator inhibitor type 1 gene polymorphisms and haplotypes are associated with plasma plasminogen activator inhibitor type 1 levels but not with myocardial infarction or stroke. Am Heart J 152:1109–1115
Goor ML van, Gomez Garcia E, Leebeek F, Brouwers GJ, Koudstaal P (2005) The plasminogen activator inhibitor (PAI-1) 4G/5G promoter polymorphism and PAI-1 levels in ischemic stroke. A case-control study. Thromb Haemost 93:92–96
Lazo-Langner A, Knoll GA, Wells PS, Carson N, Rodger A (2006) The risk of dyalisis access thrombosis is related to the transforming growth factor-beta1 production haploptype and is modified by polymorphisms in the plasminogen activator inhibitor-type 1 gene. Blood 108:4052–4058
Asselbergs FW, Williams SM, Hebert PR, Coffey CS, Hillege HL, Navis G, Vaughan DE, van Gilst WH, Moore JH (2006) The gender-specific role of polymorphisms from the fibrinolytic, renin-angiotensin, and bradykinin systems in determining plasma t-PA and PAI-1 levels. Thromb Haemost 96:471–477
Festa A, Williams K, Tracy RP, Wagenknecht LE, Haffner SM (2006) Progression of plasminogen activator inhibitor-1 and fibrinogen levels in relation to incident type-2 diabetes. Circulation 113:1753–1759
Speleman L, Kerrebin JD, Look MP, Meeuwis CA, Foekens JA, Berns EM (2006) Prognostic value of plasminogen activator inhibitor-1 in head and neck squamous cell carcinoma. Head Neck 29:341–350
Offersen BV, Pfeiffer P, Andreassen P, Overgaard J (2007) Urokinase plasminogen activator and plasminogen activator inhibitor type-1 in nonsmall-cell lung cancer: relation to prognosis and angiogenesis. Lung Cancer 56:43–50
Holmes CL, Russell JA, Walley KR (2003) Genetic polymorphisms in sepsis and septic shock: role in prognosis and potential for therapy. Chest 124:1103–1115
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was supported by grants from Fondo de Instituciones Sanitarias (020533, 020696, 020711, and 050164).
Electronic supplementary material
Rights and permissions
About this article
Cite this article
García-Segarra, G., Espinosa, G., Tassies, D. et al. Increased mortality in septic shock with the 4G/4G genotype of plasminogen activator inhibitor 1 in patients of white descent. Intensive Care Med 33, 1354–1362 (2007). https://doi.org/10.1007/s00134-007-0695-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0695-y