Abstract
Objective
To determine the effects of increasing mean arterial pressure (MAP) on renal resistances assessed by Doppler ultrasonography in septic shock.
Design and setting
Prospective, single-center, nonrandomized, open-label trial in the surgical intensive care unit in a university teaching hospital.
Patients and participants
11 patients with septic shock who required fluid resuscitation and norepinephrine to increase and maintain MAP at or above 65 mmHg.
Interventions
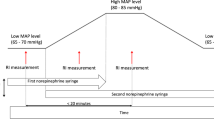
Norepinephrine was titrated in 11 patients in septic shock during three consecutive not randomized periods of 2 h to achieve a MAP at successively 65, 75, and 85 mmHg.
Measurements and results
At the end of each period hemodynamic parameters and renal function variables (urinary output, creatinine, clearance) were measured, and Doppler ultrasonography was performed on interlobar arteries to assess the renal resistive index. When increasing MAP from 65 to 75 mmHg, urinary output increased significantly from 76 ± 64 to 93 ± 68 ml/h and the resistive index significantly decreased from 0.75 ± 0.07 to 0.71 ± 0.06. No difference was found between 75 and 85 mmHg.
Conclusions
Doppler ultrasonography and resistive index measurements may help determine in each patient the optimal MAP for renal blood flow and may be a relevant end-point to titrate the hemodynamic treatment in septic shock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In septic shock, when fluid administration fails to restore an adequate arterial pressure and organ perfusion, therapy with vasopressor agents should be initiated. Updated guidelines for hemodynamic support of adult patients with sepsis recommend that vasopressors should be titrated to the minimum level required to provide an effective organ perfusion [1]. Adequate arterial pressure is the end-point of vasopressor therapy but does not always mean adequate organ blood flow.
The precise level of mean arterial pressure (MAP) required to optimize renal perfusion is still debated and certainly depends on each patient's medical history. Monitoring renal function is of great importance in intensive care units [2]. To determine the optimal arterial pressure for renal perfusion in septic shock patients the variables used are usually urinary output as an index of renal blood flow and creatinine clearance as an index of renal function [3, 4]. LeDoux et al. [3] observed that increasing MAP from 65 mmHg to 85 mmHg with norepinephrine infusion did not affect significantly urinary output. More recently Bourgoin et al. [4] reported that when MAP was increased to 85 mmHg by increasing the dose of norepinephrine in septic patients, urine flow and creatinine clearance were not improved in comparison to a group of septic patients in whom MAP was maintained at 65 mmHg. This is not surprising because norepinephrine may have opposite effects on renal blood flow. Increase in systemic pressure may increase blood flow both through a direct effect and by decreasing vascular resistance through flow-induced dilation and/or changes in the number of perfused renal vessels. However, vasoconstrictive effect of norepinephrine on renal vessels may also exist when dose increases inducing an increase in vascular resistances and reducing the renal blood flow. The net balance of these two opposite effects is difficult to evaluate in septic patients by usual parameters of renal function because they do not reflect the acute renal hemodynamic changes. In contrast the use of an ultrasonographic variable, i.e., the renal resistive index (RI), can directly and rapidly quantify modifications in renal blood flow. For instance, Lerolle et al. [5] reported recently that RI had a predictive value for acute renal failure in septic shock. This technique has also been demonstrated to be useful in the field of nephrology since Radermacher et al. [6] reported that a high RI value was predictive of poor long-term allograft survival in renal transplant.
We postulated that this renal arterial resistance index would be interesting to titrate early vasopressor therapy in septic shock patients. Thus the present study aimed to assess the effects of increasing MAP from 65 to 75 and 85 mmHg by titrating norepinephrine in septic shock, on renal hemodynamics using not only usual indices of renal perfusion but also renal arterial resistance index obtained with Doppler ultrasonography.
Methods
The study included 11 patients. The protocol was approved by our institutional ethics committee. Patients were included in the trial if within the first 12 h after they had been admitted in ICU for septic shock as defined by the Society of Critical Care Medicine/American College of Chest Physicians criteria [7]: (a) they were hemodynamically stabilized, with hypotension requiring the administration of vasopressor agents after correction of hypovolemia (the diagnosis of infection was established using the Centers for Disease Control criteria [8]), (b) written informed consent from each patient's next of kin was obtained, and (c) the echographist was available for the period of time required by the study. Exclusion criteria were any preexisting disease affecting renal vascular resistance such as unilateral kidney, renal stone disease, renal failure, or renal artery stenosis.
General management
All patients had an arterial catheter and a central venous catheter (both from Arrow International, Reading, Pa., USA). A urinary indwelling catheter was also inserted in each patient. All patients were mechanically ventilated. Sedation (with midazolam up to 5 mg/h) and analgesia (with fentanyl up to 150 μg/h) was provided according to individual needs. Patients were monitored with a transesophageal Doppler probe (CardioQ, Deltex Medical, UK). Treatment of septic shock was standardized following the Guidelines of the American College of Critical Care Medicine [1], including vasopressors to maintain MAP at 65 mmHg, in addition to repeated fluid challenges with crystalloids and artificial colloids (gelatin or hydroxyethyl starch) to optimize stroke volume and to allow the lowest dose of vasopressors to be used. Moreover, pulse pressure variation (ΔPP, expressed in percentage was used to trigger fluid challenge (all patients had ΔPP< 13%) [9, 10]. Norepinephrine was the only vasopressor used in this early phase.
Measurements
The study was divided into three consecutive periods of 2 h. During each period norepinephrine administration was adjusted to maintain MAP at successively 65, 75 and 85 mmHg. Before increasing the dose of norepinephrine and at the end of each period, measurements included temperature, heart rate, arterial pressure, and cardiac index. Arterial and venous blood samples were withdrawn simultaneously, and blood gases and lactate concentrations were measured. Age, sex, site of infection and the Simplified Acute Physiology Score (SAPS) II were noted (Table 1).
Renal measurements
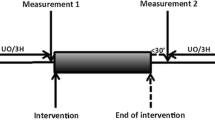
Before increasing the dose of norepinephrine and at the end of each period the 2-h urine output was measured, and creatinine was simultaneously measured in serum and in the 2-h urine collection. Renal Doppler measurements were performed before increasing the dose of norepinephrine and at the end of each 2-h period, and RI was calculated. Renal Doppler was performed on interlobar arteries by an intensive care investigator experienced in the technique using a 2.5-MHz transducer working at 1.8 MHz for Doppler analysis (Fig. 1). The Doppler gain was set in order to obtain a clear outline of flow waves with minimal background noise. Doppler spectrum was considered optimal when at least three similar consecutive waveforms were visualized. RI was calculated as: (peak systolic velocity-end diastolic velocity)/peak systolic velocity. RI value is independent of the angle between ultrasound beam and blood flow. Three measurements were performed on each kidney and RI values were averaged to obtain mean RI values for each kidney. If the difference in RI between the two kidneys was less than 0.05, the mean of the two RI values was noted; if not, the patient was excluded because this difference could have signed unilateral acute obstruction [11].
Statistical analysis
Results are reported as mean ± standard derivation except SAPS II which is expressed as median and interquartile range. Quantitative data were analyzed using Friedman's test (nonparametric test). Differences with p values less than 0.05 were considered statistically significant. Post-hoc analysis was performed using the Wilcoxon test.
Results
The mean difference between left and right renal RI was 0.01 ± 0.01. No patient presented a difference larger than 0.05. Hemodynamic and renal variables are reported in Table 2. When increasing MAP from 65 to 75 and 85 mmHg with norepinephrine infusion, there was a significant increase in cardiac index (p = 0.002) without change in heart rate.
The mean standard derivation of RI for a single patient and a single MAP was 0.02 which is comparable to values reported in the literature [12]. Renal RI decreased significantly from 0.75 ± 0.07 at MAP 65 mmHg to 0.71 ± 0.06 at MAP 75 mmHg (p = 0.003, Wilcoxon post-hoc test). No significant difference in RI value was found when increasing MAP from 75 to 85 mmHg. The individual profiles of RI as a function of changing MAP are reported in Fig. 2. An identification number is given to each patient in Fig. 2. In two cases RI did not vary with changing MAP levels; one patient had a normal RI regardless of the MAP studied (patient no. 10), and in the other RI remained increased even at the highest MAP studied (patient no. 1). In one patient RI decreased when MAP was increased from 65 to 75 mmHg but increased greatly when raising MAP to 85 mmHg (patient no. 9). In the eight remaining patients a significant decrease in renal resistance was observed when increasing MAP from 65 to 75 mmHg. No significant difference in serum creatinine or creatinine clearance was observed. A significant increase in urinary output was noticed when increasing MAP from 65 to 75 mmHg (p = 0.02, Wilcoxon post-hoc test), whereas no difference was found between 75 and 85 mmHg.
Considering these results suggesting 75 mmHg as an optimal value for renal function, a second group of patients was performed in the study. Five additional patients in septic shock and with the same criteria of inclusion and exclusion (described above) were included. During the third period norepinephrine was titrated down from 75 mmHg to 65 mmHg (instead of 85 mmHg) to assure that the previous results were related to MAP and not to time. Each period was 30 min long. During the three consecutive periods (65, 75, and 65 mmHg) RI values were respectively: 0.80 ± 0.06, 0.74 ± 0.06, and 0.78 ± 0.06. A significant difference in RI values was found between the first and second periods (p = 0.04) and between the second and third periods (p = 0.04). No difference was found between the first and third period. The individual profiles of these patients' RI as a function of changing MAP are reported in Fig. 3.
Discussion
The present study shows that in patients with septic shock a significant decrease in renal RI can be observed using Doppler ultrasonography when increasing MAP by norepinephrine from 65 mmHg to 75 mmHg. Thus Doppler ultrasonography with RI calculation can be of interest in the management of these patients to determine as early as possible the optimal MAP level for renal perfusion. In this prospective study we also report a significant increase in urinary output associated with a significant improvement in RI values when raising MAP with norepinephrine in septic shock from 65 to 75 mmHg. In contrast, our results showed that in the studied patients, increasing MAP from 75 to 85 mmHg was not associated with any benefit in terms of urinary output or RI. Futhermore, RI of the five additional patients included for whom MAP was decreased from 75 mmHg to 65 mmHg (instead of an increase to 85 mmHg) confirmed that the results of this study were related to norepinephrine and not to time.
In 1974 Pourcelot [13] described the “resistance Index” used in the assessment of Doppler velocity waveforms. Doppler of renal arteries is a rapid, noninvasive, painless, repeatable, and easy to perform technique. When applied to the kidney, this index reflects intrarenal vascular resistance distal to the point of Doppler sampling. It also presents sufficient reproducibility when performed on the interlobar arteries [14]. A value of mean renal RI of 0.60 is considered as a normal value [12], whereas 0.70 is considered the upper threshold of the normal RI in adults [15, 16].
The use of Doppler ultrasonography to assess renal blood flow is increasing in many kidney diseases. For example, RI has been studied in ureteral obstruction [11, 17], evaluation of solitary kidney function [18], renal transplant dysfunction [6] and several diseases such as diabetic nephropathy and atherosclerosis [19]. RI is also correlated to the progression of renal disease [20, 21]. In 2006 Lerolle et al. [5] reported the first application of RI in the field of sepsis and intensive care. In this prospective study the authors proved that in septic shock RI performed on day 1 had a predictive value for acute renal failure apparition in the 5 following days.
Renal perfusion may be compromised early in the vasodilated conditions of septic shock, and this often leads to acute renal failure [22]. Current treatment of acute renal failure in septic shock combines early fluid resuscitation and administration of vasopressor agents such as norepinephrine to maintain MAP above an “adequate” threshold. Norepinephrine is currently recommended to restore blood pressure, and its nephroprotective effects makes it part of the septic shock treatment [23]. Nevertheless in these circumstances one must balance improving regional perfusion and inducing excessive vasoconstriction. Consensus recommendations suggest that 65 mmHg is the acceptable lowest limit to maintain adequate global circulatory conditions. However, patients with underlying cardiovascular disease may require higher levels of MAP because of shifts in their autoregulatory curves. Thus there is no universal optimal MAP in septic shock patients, and individual adjustment of MAP may be of value to obtain optimal organ blood flow. One previous study which assessed the role of norepinephrine on renal function in septic shock concluded that a MAP value of 65 mmHg should not be the end-point, but that the best MAP should be determined according to clearly defined perfusion goals [24]. The present study clearly showed that renal Doppler can help to achieve this goal, allowing the optimal MAP to be determined for each septic shock patient. Determining the optimal MAP level not only on systemic parameters but also on regional perfusion indices such as RI could be beneficial as it may help optimizing organ perfusion. In our study, increasing MAP with norepinephrine was associated with a decrease in renal resistance and RI significantly decreased between 65 and 75 mmHg. This result is in agreement with a recent animal study; Peng et al. [25] showed in bacteremic dogs that increasing the dose of norepinephrine is associated with a partial improvement of renal perfusion.
We believe that our results may suffer from some confounding variables. RI has been shown to be correlated with age [26] and some cardiovascular risk factors including atherosclerosis [19] or primary hypertension [27]. In our study only one patient had a history of untreated hypertension (patient no. 1). It is interesting to note that this patient is the only one in whom RI values remained high and unmodified regardless of the MAP value. It has already been proposed that such patients may benefit from higher MAP levels because of a higher level of autoregulation in regional circulations. However, concerning this patient, using RI, it is clear that there was no benefit to increase MAP. Furthermore the nonrandomized and open-label characteristics of this study are also a possible confounder. Another limitation in our study is the small number of patients, but the goal of our study was to assess the effects of titrating norepinephrine to increase MAP on renal arterial resistance and was not powered to evaluate an improvement in renal function. Moreover, creatinine clearance was calculated using the creatinine concentration measured in a 2-h urine collection which is questionable as a reliable estimation of creatinine clearance [28]. Larger studies with a longer period of assessment are needed to determine the impact, if any, of early optimization of renal perfusion using renal RI on the prevention of renal failure in septic shock.
In conclusion, we have shown that Doppler ultrasonography and renal RI may help to determine in each patient the optimal MAP for renal blood flow and can be a relevant end-point to adjust hemodynamic treatment in septic shock. This new parameter may be in the future an assessment tool for renal perfusion in everyday ICU practice.
References
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Andrews P, Azoulay E, Antonelli M, Brochard L, Brun-Buisson C, Dobb G, Fagon JY, Gerlach H, Groeneveld J, Mancebo J, Metnitz P, Nava S, Pugin J, Pinsky M, Radermacher P, Richard C, Tasker R, Vallet B (2005) Year in review in intensive care medicine, 2004. II. Brain injury, hemodynamic monitoring and treatment, pulmonary embolism, gastrointestinal tract, and renal failure. Intensive Care Med 31:177–188
LeDoux D, Astiz ME, Carpati CM, Rackow EC (2000) Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med 28:2729–2732
Bourgoin A, Leone M, Delmas A, Garnier F, Albanese J, Martin C (2005) Increasing mean arterial pressure in patients with septic shock: effects on oxygen variables and renal function. Crit Care Med 33:780–786
Lerolle N, Guerot E, Faisy C, Bornstain C, Diehl JL, Fagon JY (2006) Renal failure in septic shock: predictive value of Doppler-based renal arterial resistive index. Intensive Care Med 32:1553–1559
Radermacher J, Mengel M, Ellis S, Stuht S, Hiss M, Schwarz A, Eisenberger U, Burg M, Luft FC, Gwinner W, Haller H (2003) The renal arterial resistance index and renal allograft survival. N Engl J Med 349:115–124
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
Michard F, Chemla D, Richard C, Wysocki M, Pinsky MR, Lecarpentier Y, Teboul JL (1999) Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med 159:935–939
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Mostbeck GH, Zontsich T, Turetschek K (2001) Ultrasound of the kidney: obstruction and medical diseases. Eur Radiol 11:1878–1889
Tublin ME, Bude RO, Platt JF (2003) The resistive index in renal Doppler sonography: where do we stand? AJR Am J Roentgenol 180:885–892
Pourcelot L (1974) Applications cliniques de l'examen Doppler transcutané. In: Peronneau P (ed) Velocimetrie ultrasonore Doppler, INSERM, Paris, pp 213–240
Knapp R, Plotzeneder A, Frauscher F, Helweg G, Judmaier W, zur Nedden D, Recheis W, Bartsch G (1995) Variability of Doppler parameters in the healthy kidney: an anatomic-physiologic correlation. J Ultrasound Med 14:427–429
Platt JF, Ellis JH, Rubin JM (1991) Examination of native kidneys with duplex Doppler ultrasound. Semin Ultrasound CT MR 12:308–318
Platt JF (1992) Duplex Doppler evaluation of native kidney dysfunction: obstructive and nonobstructive disease. AJR Am J Roentgenol 158:1035–1042
Rawashdeh YF, Djurhuus JC, Mortensen J, Horlyck A, Frokiaer J (2001) The intrarenal resistive index as a pathophysiological marker of obstructive uropathy. J Urol 165:1397–1404
Shokeir AA, Abubieh EA, Dawaba M, el-Azab M (2003) Resistive index of the solitary kidney: a clinical study of normal values. J Urol 170:377–379
Ohta Y, Fujii K, Arima H, Matsumura K, Tsuchihashi T, Tokumoto M, Tsuruya K, Kanai H, Iwase M, Hirakata H, Iida M (2005) Increased renal resistive index in atherosclerosis and diabetic nephropathy assessed by Doppler sonography. J Hypertens 23:1905–1911
Petersen LJ, Petersen JR, Ladefoged SD, Mehlsen J, Jensen HA (1995) The pulsatility index and the resistive index in renal arteries in patients with hypertension and chronic renal failure. Nephrol Dial Transplant 10:2060–2064
Radermacher J, Ellis S, Haller H (2002) Renal resistance index and progression of renal disease. Hypertension 39:699–703
Schrier RW, Wang W (2004) Acute renal failure and sepsis. N Engl J Med 351:159–169
Bellomo R, Giantomasso DD (2001) Noradrenaline and the kidney: friends or foes? Crit Care 5:294–298
Reisbeck M, Astiz ME (2005) Arterial pressure, vasopressors and septic shock: higher is not necessarily better. Crit Care Med 33:906–907
Peng ZY, Critchley LA, Fok BS (2005) The effects of increasing doses of noradrenaline on systemic and renal circulations in acute bacteraemic dogs. Intensive Care Med 31:1558–1563
Zubarev AV (2001) Ultrasound of renal vessels. Eur Radiol 11:1902–1915
Derchi LE, Leoncini G, Parodi D, Viazzi F, Martinoli C, Ratto E, Vettoretti S, Vaccaro V, Falqui V, Tomolillo C, Deferrari G, Pontremoli R (2005) Mild renal dysfunction and renal vascular resistance in primary hypertension. Am J Hypertens 18:966–971
Cherry RA, Eachempati SR, Hydo L, Barie PS (2002) Accuracy of short-duration creatinine clearance determinations in predicting 24-hour creatinine clearance in critically ill and injured patients. J Trauma 53:267–271
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deruddre, S., Cheisson, G., Mazoit, JX. et al. Renal arterial resistance in septic shock: effects of increasing mean arterial pressure with norepinephrine on the renal resistive index assessed with Doppler ultrasonography. Intensive Care Med 33, 1557–1562 (2007). https://doi.org/10.1007/s00134-007-0665-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0665-4