Abstract
Objective
To appraise the literature on the value of urinary biomarkers in septic acute kidney injury (AKI).
Design
Systematic review.
Setting
Academic medical centre.
Patients and participants
Human studies of urinary biomarkers.
Interventions
None.
Measurements and results
Fourteen articles fulfilled inclusion criteria. Most studies were small, single-centre, and included mixed medical/surgical adult populations. Few focused solely on septic AKI and all had notable limitations. Retrieved articles included data on low-molecular-weight proteins (β2-microglobulin, α1-microglobulin, adenosine deaminase binding protein, retinol binding protein, cystatin C, renal tubular epithelial antigen-1), enzymes (N-acetyl-β-glucosaminidase, alanine-aminopeptidase, alkaline phosphatase; lactate dehydrogenase, α/π-glutathione-S-transferase, γ-glutamyl transpeptidase), cytokines [platelet activating factor (PAF), interleukin-18 (IL-18)] and other biomarkers [kidney injury molecule-1, Na/H exchanger isoform-3 (NHE3)]. Increased PAF, IL-18, and NHE3 were detected early in septic AKI and preceded overt kidney failure. Several additional biomarkers were evident early in AKI; however, their diagnostic value in sepsis remains unknown. In one study, IL-18 excretion was higher in septic than in non-septic AKI. IL-18 also predicted deterioration in kidney function, with increased values preceding clinically significant kidney failure by 24–48 h. Detection of cystatin C, α1-microglobulin, and IL-18 predicted need for renal replacement therapy (RRT).
Conclusions
Few clinical studies of urinary biomarkers in AKI have included septic patients. However, there is promising evidence that selected biomarkers may aid in the early detection of AKI in sepsis and may have value for predicting subsequent deterioration in kidney function. Additional prospective studies are needed to accurately describe their diagnostic and prognostic value in septic AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a common clinical problem in critically ill patients [1, 2]. Sepsis is now recognized as the most important contributing factor for AKI in this population [1]. Epidemiologic studies have reported AKI requiring renal replacement therapy (RRT) in 43–50% of patients with septic shock [3–5]. In addition, mortality in septic AKI remains exceedingly high [6–8].
AKI has traditionally been defined and detected by measuring surrogates of kidney function such as serum creatinine and urea [9]. However, these markers are insensitive and non-specific for both acute changes to kidney function and kidney injury. They also increase late in the injury process. As a consequence, they may not detect an acute insult or potentially ongoing injury to the kidney.
On the other hand, several novel biomarkers (i.e. antigens, peptides, enzymes, cytokines) have been detected in the urine in AKI and have been characterized as potential early, non-invasive, and more sensitive indicators of AKI [10–12]. Moreover, the pattern of urinary excretion of these biomarkers may potentially aid in understanding the pathophysiology of AKI, allow for localization of injury to specific segments of the nephron, be used to correlate outcome with both the onset and severity of initial injury, and potentially provide added prognostic information.
Accordingly, we systematically reviewed the literature in order to describe the urinary biomarkers detected when the principal stimulus for AKI was sepsis. The primary objectives of our review were: (1) to document those urinary biomarkers that have been detected in septic AKI; (2) to determine the diagnostic value of these biomarkers in septic AKI; and (3) to determine whether these biomarkers have prognostic value in septic AKI.
Methods
Search strategy
Two individuals (S. M. B. and C. L.) independently identified published articles of urinary biomarkers in septic AKI by use of both electronic and manual search strategies. An initial screen of identified abstracts was performed followed by a full text screen of each article identified. Our search was supplemented by scanning the bibliographies of all recovered articles. This comprehensive search was performed in September 2005 and updated in December 2006.
The databases MEDLINE (1966 through August, 2005), EMBASE (1980 through 2005, Week 38), CINAHL (1982 through 2005, September Week 2) were searched. PubMed was also searched. Articles in any language were considered.
Three comprehensive search themes were derived. The first search theme was compiled by using the term “OR” with the following medical subject headings (MeSH) and textwords: “acute renal failure”, “acute kidney failure”, “acute tubular necrosis”, “kidney dysfunction”. The second search theme was put together by using the term “OR” with the following MeSH headings and textwords: “sepsis”, “septicemia”, “septic shock”, “bacteremia”, “lipopolysaccharide”, “endotoxin”, and “gram negative”. The final search theme used the term “OR” with the following MeSH headings and textwords: “urinary biomarker”, “kidney injury molecule-1”, “cystatin C”, “sodium-hydrogen exchanger isoform 3 (NHE3)”, “neutrophil gelatinase-associated lipocalin (NGAL)”, “cytokine”, “interleukin-18 (IL-18)”, “β2-microglobulin”, “urinary retinol binding protein (RBP)”, “enzymuria”, and “aminoaciduria”. These three search themes were then combined using the Boolean operator “AND”.
Study selection
Two individuals independently evaluated all identified articles for eligibility on the basis of four criteria: (1) articles reported original data from a primary publication; (2) articles reported on human subjects; (3) articles made specific mention of urinary biomarkers in AKI; and (4) articles included subjects with sepsis syndrome or septic shock and this represented the principal cause for AKI. Agreement on article inclusion was quantified by the kappa statistic, with disagreements resolved by discussion.
Data extraction and synthesis
Data extracted included: study methods, number of patients and proportion with sepsis, patient population (i.e. adult, critically ill, surgical); details of sepsis, haemodynamic profile, baseline/enrolment kidney function, use of renal replacement therapy (RRT); and mortality outcome. Data were also extracted on specific urinary biomarkers and included: mean/median and peak urinary concentrations detected, timing of detection, operative characteristics when available and the presence of potential confounder factors.
Results
Study selection
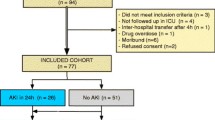
The combined computerized and bibliographic search yielded 175 unique citations, of which only 67 were identified as potentially relevant and reviewed further. In all, 14 unique articles fulfilled all inclusion criteria. Agreement was good between reviewers for inclusion. Actual agreement was 91% (chance corrected, kappa 0.81 ± 0.07) and all discrepancies were resolved by consensus.
Study characteristics
Study characteristics are shown in Table 1. Ten (71%) studies were in adults. Four (29%) were focused solely in critically ill patients. Most studies (71%) were performed in mixed medical/surgical patients. Only four studies exclusively enrolled patients with documented or suspected sepsis and in three of these, the focus was on detection of aminoglycoside toxicity. Most studies were small, single-centre, prospective, observational and included a control group for comparison (Table 1). Few studies provided data on patient haemodynamics, use of vasopressors, or mortality.
Measures of kidney function
Details of kidney function across studies are displayed in Table 2. The occurrence of AKI varied between studies, and few provided complete data on estimated glomerular filtration rate, serum creatinine, or urine output. Only two studies (14%) reported on the proportion of patients that received RRT.
Limitations of included studies
Inferences on the value of urinary biomarkers in septic AKI described in this review may be limited due to: (1) not all patients described across reports had sepsis; (2) not all patients described across reports had AKI; (3) several studies had potential confounding factors (Table 3); (4) several reports had potential weaknesses in study design (i.e. single centre and/or tertiary referral centre, small sample size, no control group); and (5) several reports were prone to selection bias due to study inclusion/exclusion criteria. For example, studies excluded patients based on radiographic evidence of small bilateral kidneys, those with biochemically defined pre-renal failure (i.e. FeNa < 1%), those not fulfilling sufficient criteria to be classified as having acute tubular necrosis (ATN) or those requiring RRT within 48 h [13–15].
Urinary biomarkers
The urinary biomarkers described in septic AKI are outlined in Tables 4 and 5. As a general rule, the detection of urinary biomarkers was considered a surrogate for evidence of structural injury to renal tubular epithelial cells occurring before and/or during overt acute renal failure (ARF), specifically ATN. In selected instances, biomarker detection occurred prior to clinically evident increases in serum creatinine and/or urea [16–19].
Low-molecular-weight proteinuria
β 2 -Microglobulin (β 2 -M) is an endogenous 12-kDa protein that forms part of the class I major histocompatibility complex. β2-M is freely filtered at the glomerulus and subsequently reabsorbed and catabolized by proximal renal tubular cells. It is not normally detected in the urine. Urinary β2-M excretion was described in four studies (29%) [14, 17–19]. In three of these studies, it was used for detection of tubular damage attributed to aminoglycosides rather than sepsis [17–19]. However, in one study, 90% of critically ill neonates had significant increases in urinary detection of β2-M, while only 17% exhibited evidence of abnormal serum creatinine values [17]. Moreover, the highest detected β2-M levels were in septic neonates. However, Cabrera et al. found no difference in β2-M levels between septic and non-septic patients when tubular injury was arbitrarily defined by β2-M values > 3,000 μg/l [18]. In a small observational study, Herget-Rosenthal et al. found that urinary β2-M performed poorly at predicting need for RRT [area under receiver operating characteristic curve (AuROC) 0.51] [14].
α 1 -Microglobulin (α 1 -M) is a 31-kDa protein produced by the liver and associated with immunoglobulin A. Similar to β2-M, α1-M is freely filtered at the glomerulus and is completely reabsorbed when tubular function is normal. Only two studies (14%) including septic patients assessed urinary α1-M excretion [14, 19]. In one study of neonatal sepsis treated with aminoglycosides, α1-M was found to be significantly increased at > 3 days [19]. Herget-Rosenthal et al. found that early detection of increased urinary α1-M was an excellent discriminator for future need of RRT (AuROC 0.86) [14].
Adenosine deaminase binding protein (ABP) is a120-kDa glycoprotein found in the brush border of proximal renal tubular cells. Increased ABP detection in the urine is considered indicative of AKI; however, most studies have only described ABP in non-septic patients with ischaemic, nephrotoxic or post-transplant AKI [20, 21]. ABP was described in only one study of neonatal sepsis [19]. Urinary excretion of ABP was found to be a superior and earlier marker of AKI than both β2-M and α1-M [19].
Retinol binding protein (RBP) is a 21-kDa protein synthesized primarily in the liver and bound in serum with pre-albumin and vitamin A. RBP is freely filtered and reabsorbed by proximal tubular cells. Detection of urinary RBP is considered indicative of tubular damage. Urinary RBP was described in two studies (14%) that included septic patients [14, 22]. Du Cheyron et al. found that urinary RBP was significantly increased in AKI compared with non-AKI controls; however, levels of RBP were unable to discriminate pre-renal AKI and ATN [22]. Increased urinary RBP was intermediately discriminatory for need of RRT (AuROC 0.80) [14].
Cystatin C is an endogenous cysteine proteinase inhibitor synthesized at a relatively constant rate and released into plasma by all nucleated cells in the body. It is freely filtered at the glomerulus, not secreted or reabsorbed, and nearly completely catabolized by proximal renal tubular cells and thus not normally detected in the urine [23]. Herget-Rosenthal et al. found that urinary cystatin C was predictive for need of RRT (AuROC 0.92), performing better than several other urinary biomarkers (i.e. β2-M, RBP, γ-GT, LDH, α-GST, NAG) [14].
Proximal renal tubular epithelial antigen (HRTE-1) is a proximal tubular brush border peptide that is sloughed into the tubular lumen and detected in the urine following kidney injury [24]. While Zager et al. described an increase in urinary HRTE-1 excretion in ATN that was not evident in pre-renal AKI, only nine patients in this study were septic. Consequently, no inferences were possible for septic versus non-septic AKI.
Enzymuria
Numerous urinary enzymes have been studied as early and non-invasive biologic indicators of AKI [11, 12]. We found five studies (35%) that described the detection of urinary enzymes and included septic patients [13, 14, 16, 25, 26]. Two were in neonatal/paediatric populations that focused on aminoglycoside toxicity rather than sepsis and had limited value [25, 26]. Several urinary enzymes were detected, including alanine aminopeptidase (AAP), alkaline phosphatase (ALP), N-acetyl-β-glucosaminidase (NAG), lactate dehydrogenase (LDH), α-glutathione S-transferase (α-GST), π-glutathione S-transferase (π-GST), and γ-glutamyl transpeptidase (γ-GT). These enzymes are released from various sites in the nephron (i.e. proximal tubule, loop of Henle, distal tubule) and may reflect different patterns of subcellular injury (i.e. lysosomal, cytoplasmic, brush border membrane).
Chew et al. described the urinary detection of ALP and NAG in a cohort of 50 non-critically ill patients with ARF, of which 38% had probable sepsis as a contributing factor [13]. Both higher urinary ALP and NAG at the time of diagnosis and higher peak NAG, despite similar serum creatinine values, were associated with a poor prognosis, defined as death or RRT dependence at hospital discharge [13]. Regrettably, no data were available on the time to peak urinary measures or on values in the septic subgroup. Interestingly, urinary ALP and NAG failed to discriminate pre-renal ARF from ATN when classified by traditional biochemical criteria.
Westhuyzen et al. described the detection of several urinary enzymes (γ-GT, ALP, NAG, LDH, α/π-GST) in a small cohort of critically ill patients [16]. All urinary enzymes (except LHD) were significantly higher at ICU admission in those who developed ARF (defined as an increase of at least 50% in baseline serum creatinine to a value ≥ 150 μmol/l) than in controls and preceded evidence of ARF by serum creatinine criteria by a median 36 h. All urinary enzymes (except LHD) had excellent discrimination (AuROC > 0.80) for predicting ARF and were superior in this respect to serum creatinine and calculated creatinine clearance (AuROC 0.79). Regrettably, in this study there were only four patients who developed ARF, only one of whom was septic; thus, inferences are limited.
Recently, Herget-Rosenthal assessed whether patterns of the urinary low-molecular-weight protein and enzyme excretion could predict the need for RRT in 73 non-critically ill patients with ATN (defined by traditional biochemical criteria), of which 26% had sepsis [14]. RRT was required in 36% after a median 4 days. Of the enzymes measured, NAG had the greatest discrimination for need for RRT (AuROC 0.81), yet performed less well than cystatin C and α1-M. The remaining urinary enzymes were less predictive of need for RRT.
Cytokines
Platelet activating factor (PAF) is a phospholipid mediator of inflammation that has been shown to participate in the pathophysiology of septic AKI [27]. Mariano et al. described significant early elevations in urinary PAF in 12 critically ill patients with septic shock and AKI [28]. Furthermore, urinary PAF correlated with other serum and urine inflammatory cytokines, specifically serum IL-6, serum IL-8 and urine IL-6. Serum PAF was also found to correlate with serum creatinine concentration. This study suggests that PAF may contribute to the pathophysiology of septic AKI and that urinary PAF may predict the clinical course and correlate with severity of AKI. In this study, the urinary concentration of cytokines IL-1β or TNF-α added little information.
Interleukin-18 (IL-18) has been shown to be a potent mediator of ischaemia-induced AKI in experimental models [29, 30]. Early detection of urinary IL-18 has been shown to predict delayed graft failure after kidney transplantation and late increases (48–72 h) in serum creatinine after cardiac surgery with cardiopulmonary bypass [31, 32]. Parikh et al. found that urinary IL-18 levels were significantly elevated in patients with ATN compared with patients with pre-renal azotaemia, urinary tract infection, or chronic kidney disease or with healthy controls [31]. This study found that a cut-off urinary IL-18 to serum creatinine ratio of 500 pg/mg creatinine had sensitivity and specificity of 85% and 88% for the diagnosis of ATN, respectively. Unfortunately, of the 22 patients with ARF (pre-renal and ATN), only 27% had sepsis, and the timing of measurement of urinary IL-18 was not specified. However, despite similar serum creatinine concentrations in septic and non-septic AKI patients (281 ± 114 μmol/l vs. 291 ± 142 μmol/l, p = 0.86), urinary IL-18 was significantly higher in those with a diagnosis of sepsis (1010 ± 763 pg/mg creatinine vs. 411 ± 382 pg/mg creatinine, p = 0.02). More recently, in a nested case–control study of mostly septic critically ill patients with acute respiratory distress syndrome (ARDS), an elevated urinary IL-18 value preceded clinical evidence of overt ARF by 24–48 h [33]. Moreover, an increased urinary IL-18 to creatinine ratio > 100 pg/mg creatinine had a 6.5-fold increase in odds of AKI within 24 h (odds ratio 6.5, 95% confidence interval 2.1–20.4). Finally, a high urinary IL-18 at the time of enrolment was also an independent predictor of mortality.
Additional Biomarkers
Kidney injury molecule-1 (KIM-1) is a type 1 transmembrane glycoprotein that is markedly up-regulated in proximal renal tubular cells in response to ischaemic or nephrotoxic AKI [34–36]. The ectodomain segment of KIM-1 is shed from proximal cells and detected in the urine by immunoassay [15]. KIM-1 levels are higher for ATN defined by abnormal sediment compared with other AKI (2.0 ng/ml vs. 0.22 ng/ml). Increased urinary detection of KIM-1 was found superior to urinary ALP and γ-GT for the diagnosis of ATN [15]. Moreover, kidney biopsies from patients with ATN show significantly greater KIM-1 tissue expression than other acute and chronic kidney diseases. However, no biopsy specimens were taken from septic patients. Moreover, of those with ischaemic ATN, only four had sepsis, and there was no significant difference in KIM-1 levels between the septic and non-septic patients.
Urinary Na+/H+ exchanger isoform 3 (NHE3) is the most abundant sodium transporter in the renal tubule and is responsible for the reabsorption of large quantities of filtered sodium from the urine. NHE3 is not normally detectable in the urine; however, abnormal elevations have been described in critically ill patients with AKI [22]. Du Cheyron et al. found urinary NHE3 was higher in those with ATN than with pre-renal ARF (6.1 vs. 0.92, p< 0.0001) and undetectable in controls or those with other causes of intrinsic ARF (i.e. glomerulonephritis or vasculitis). In addition, NHE3 was shown to be superior to RBP in discriminating pre-renal AKI and ATN and correlated positively with serum creatinine concentration. Urinary NHE3 was serially followed in two patients admitted to ICU with septic shock and normal initial kidney function who later developed AKI. At baseline, urinary NHE3 was undetected in these two patients; however, both later showed acute increases in the urine membrane fractions of NHE3 that corresponded with clinical evidence of AKI. Moreover, the NHE3 became undetectable again upon recovery of kidney function.
Novel biomarkers not described in septic AKI
There are several additional novel urinary biomarkers that have been characterized in AKI, including neutrophil gelatinase-associated lipocalin (NGAL) [37–39]; cysteine-rich protein 61 (Cyr61) [40]; perforin and granzyme B [41]; CXCR3-binding chemokines [42]; urinary endothelin; and urinary SSAT [43]. Regrettably, however, most of these biomarkers have been characterized in ischaemic or nephrotoxic AKI, following kidney transplant, or have been restricted to experimental studies and have yet to be evaluated in AKI associated with sepsis.
Discussion
We performed a systematic review of all human studies describing urinary biomarkers to assess their diagnostic and prognostic value in septic AKI. We found there are numerous biomarkers that have been characterized for the early and non-invasive detection of AKI. However, relatively few clinical studies have documented their urinary excretion in septic AKI. Moreover, several recently characterized urinary biomarkers have yet to be described in patients with septic AKI. We also found that studies included in our review showed marked heterogeneity, specifically in terms of patient populations, severity of illness, study inclusion/exclusion criteria, proportion with sepsis, and the presence of potential confounding factors. Due to these features, inferences regarding the diagnostic and prognostic value of urinary biomarkers in septic AKI are limited and problematic.
On the other hand, we found that urinary IL-18 excretion was higher in septic than in non-septic AKI patients; increased urinary excretion of IL-18 was a predictor for subsequent deterioration in kidney function preceding clinically significant AKI by 24–48 h. These observations suggest that IL-18 may represent a useful early marker of AKI. We also found evidence that selected biomarkers (i.e. PAF, IL-18, NHE3) may aid in the detection of early kidney injury in sepsis prior to the development of overt kidney failure characterized by elevated serum creatinine and/or urea. Several additional low-molecular-weight proteins (i.e. β2-M, α1-M, ABP) and enzymes (i.e. γ-GT, ALP, NAG, α/π-GST) may be evident early in the urine of patients with AKI and precede clinical evidence of ARF; however, their value in sepsis remains unclear. Finally, we found that an increase in urinary excretion of selected biomarkers (i.e. cystatin C, α1-M, IL-18) may have prognostic importance and forecast the need for RRT and mortality.
We believe the findings of our review have particular importance for the septic critically ill patient. Sepsis is a highly prevalent syndrome in critical illness and is the leading precipitant of AKI [1], with mortality rates in excess of 70% [6–8]. Moreover, the distinction between septic and non-septic AKI may have clinical relevance. Experimental and clinical data suggest that septic AKI may be characterized by a distinct pathophysiology [44–47]. Thus, we believe septic AKI may be a unique condition. We further hypothesize that in septic AKI there may be distinguishing patterns in the urinary excretion of biomarkers. Our review presents some evidence to support this hypothesis by finding that urinary IL-18 excretion was higher in septic than in non-septic AKI [31]. In addition, selected biomarkers, such as PAF and IL-18, may directly or indirectly induce AKI, and a broader knowledge of their pattern of excretion in septic AKI may lead to further understanding of the pathophysiology of septic AKI. Regrettably, however, we still have little understanding of urinary biomarkers in this condition [48].
The availability of urinary biomarkers as a non-invasive tool to identify early AKI may provide important diagnostic and prognostic data for the septic critically ill patient. In particular, the detection of abnormally elevated urinary biomarkers consistent with AKI may provide lead time and allow for initiation of supportive therapies and/or interventions before the development of overt functional ARF [49–51]. Delay in diagnosis and in initiation of supportive care may adversely impact clinical outcome [49] while the early application of such care may show clinical benefit [52]. Urinary biomarkers (i.e. IL-18, NHE3, NGAL, KIM-1, cystatin C) may play an important role in future clinical trials by identifying early those patients most likely to benefit. Likewise, these urinary biomarkers, once characterized in larger studies, may represent ideal non-invasive markers for the stratification of septic critically ill patients with early AKI in future randomized clinical trials of novel interventions or changes in process of care.
The ideal urinary biomarker in AKI would have several characteristics, including reliable detection of AKI; being sufficiently sensitive to detect early subclinical injury; reflecting the location of kidney injury; reflecting time-dependent changes in the severity of injury (i.e. analogous to serum creatine kinase levels in acute myocardial infarction); and being simple, cheap and easy to measure. Unfortunately, no single urinary biomarker currently fulfils all these ideal traits. In addition, there are problems with the routine use of many of these urinary biomarkers. For example, there may be a low threshold of injury for many urinary enzymes (high sensitivity), while at the same time increased excretion with a variety of clinical conditions other than AKI (i.e. chronic glomerular diseases) (low specificity) that would limit their value. Moreover, many newer and more promising urinary biomarkers described in our review are at present not widely available or are too expensive, making their application outside of research settings limited. More importantly, perhaps, most studies to date have used these urinary biomarkers to simply discriminate pre-renal ARF from ATN [11]. Rather, future prospective investigations of urinary biomarkers in septic and non-septic AKI should aim to describe the timing of detection (i.e. onset of injury) and the peak and duration of excretion (i.e. severity of injury) and to correlate these findings with both traditional measures of kidney function (i.e. serum creatinine, urea) and clinically important outcomes (i.e. need for RRT, renal recovery, mortality). Moreover, future experimental models of septic AKI should correlate the detection and course of urinary biomarker excretion with kidney haemodynamics and kidney tubular cell histopathology [47, 53]. Finally, the performance of several urinary biomarkers should be assessed to determine whether any particular pattern of excretion has greater diagnostic and prognostic value than single urinary biomarkers alone. These uncertainties need to be examined in large prospective studies of critically ill patients with sepsis.
There are limitations to our study. First, despite a rigorous search, we may have missed some reports that fulfil our inclusion criteria. For example, we may have missed reports that focused solely on urinary biomarkers for the detection of aminoglycoside nephrotoxicity. In the end, however, we believe that our findings would not be significantly prejudiced as a consequence. Second, our findings have limited generalizability to the critically ill patient for the reasons discussed. Finally, few studies assessed the temporal profile of these urinary biomarkers and correlated their time to detection and peak value with traditional markers of kidney function, thus making inferences about diagnosis and prognosis difficult. Furthermore, despite normalization to urinary creatinine these biomarkers may in part be dependent on urine output and concomitant diuresis [14, 54].
Conclusion
While there are numerous urinary biomarkers that have been characterized for the early and non-invasive detection of AKI, few have been documented in septic AKI, and available studies have notable limitations. However, there is evidence to suggest that selected urinary biomarkers may aid in the early detection of AKI in sepsis and have predictive value. The early detection of AKI may facilitate the development of new therapies, as the early detection of myocardial ischaemia has done in cardiology. Thus, prospective studies are needed to accurately describe the role and course of these biomarkers in septic AKI and their significance for clinical practice.
References
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818
Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA (2006) RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care 10:R73
Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, Godinez-Luna T, Svenson LW, Rosenal T (2005) Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care 9:R700–R709
Cole L, Bellomo R, Silvester W, Reeves JH (2000) A prospective, multicenter study of the epidemiology, management, and outcome of severe acute renal failure in a “closed” ICU system. Am J Respir Crit Care Med 162:191–196
Silvester W, Bellomo R, Cole L (2001) Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit Care Med 29:1910–1915
Yegenaga I, Hoste E, Van Biesen W, Vanholder R, Benoit D, Kantarci G, Dhondt A, Colardyn F, Lameire N (2004) Clinical characteristics of patients developing ARF due to sepsis/systemic inflammatory response syndrome: results of a prospective study. Am J Kidney Dis 43:817–824
Neveu H, Kleinknecht D, Brivet F, Loirat P, Landais P (1996) Prognostic factors in acute renal failure due to sepsis. Results of a prospective multicentre study. The French Study Group on Acute Renal Failure. Nephrol Dial Transplant 11:293–299
Hoste EA, Lameire NH, Vanholder RC, Benoit DD, Decruyenaere JM, Colardyn FA (2003) Acute renal failure in patients with sepsis in a surgical ICU: predictive factors, incidence, comorbidity, and outcome. J Am Soc Nephrol 14:1022–1030
Bellomo R, Kellum JA, Ronco C (2004) Defining acute renal failure: physiological principles. Intensive Care Med 30:33–37
Rabb H (1998) Evaluation of urinary markers in acute renal failure. Curr Opin Nephrol Hypertens 7:681–685
Han WK, Bonventre JV (2004) Biologic markers for the early detection of acute kidney injury. Curr Opin Crit Care 10:476–482
Trof RJ, Di Maggio F, Leemreis J, Groeneveld AB (2006) Biomarkers of acute renal injury and renal failure. Shock 26:245–253
Chew SL, Lins RL, Daelemans R, Nuyts GD, De Broe ME (1993) Urinary enzymes in acute renal failure. Nephrol Dial Transplant 8:507–511
Herget-Rosenthal S, Poppen D, Husing J, Marggraf G, Pietruck F, Jakob HG, Philipp T, Kribben A (2004) Prognostic value of tubular proteinuria and enzymuria in nonoliguric acute tubular necrosis. Clin Chem 50:552–558
Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV (2002) Kidney Injury Molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int 62:237–244
Westhuyzen J, Endre ZH, Reece G, Reith DM, Saltissi D, Morgan TJ (2003) Measurement of tubular enzymuria facilitates early detection of acute renal impairment in the intensive care unit. Nephrol Dial Transplant 18:543–551
Mehta KP, Ali US, Shankar L, Tirthani D, Ambadekar M (1997) Renal dysfunction detected by beta-2 microglobulinuria in sick neonates. Indian Pediatr 34:107–111
Cabrera J, Arroyo V, Ballesta AM, Rimola A, Gual J, Elena M, Rodes J (1982) Aminoglycoside nephrotoxicity in cirrhosis. Value of urinary beta 2-microglobulin to discriminate functional renal failure from acute tubular damage. Gastroenterology 82:97–105
Gordjani N, Burghard R, Muller D, Mathai H, Mergehenn G, Leititis JU, Brandis M (1995) Urinary excretion of adenosine deaminase binding protein in neonates treated with tobramycin. Pediatr Nephrol 9:419–422
Tolkoff-Rubin NE, Thompson RE, Piper DJ, Hansen WP, Bander NH, Cordon-Cardo C, Finstad CJ, Klotz LH, Old LJ, Rubin RH (1987) Diagnosis of renal proximal tubular injury by urinary immunoassay for a proximal tubular antigen, the adenosine deaminase binding protein. Nephrol Dial Transplant 2:143–148
Tolkoff-Rubin NE, Cosimi AB, Delmonico FL, Russell PS, Thompson RE, Piper DJ (1988) Diagnosis of tubular injury in renal transplant patients by a urinary assay for a proximal tubular antigen, the adenosine-deaminase binding protein. Transplantation 41:593–597
Du Cheyron D, Daubin C, Poggioli J, Ramakers M, Houillier P, Charbonneau P, Paillard M (2003) Urinary measurement of Na+/H+ exchanger isoform 3 (NHE3) protein as new marker of tubule injury in critically ill patients with ARF. Am J Kidney Dis 42:497–506
Herget-Rosenthal S, Feldkamp T, Volbracht L, Kribben A (2004) Measurement of urinary cystatin C by particle-enhanced nephelometric immunoassay: precision, interferences, stability and reference range. Ann Clin Biochem 41:111–118
Zager RA, Rubin NT, Ebert T, Maslov N (1980) Rapid radioimmunoassay for diagnosing acute tubular necrosis. Nephron 26:7–12
Ehrich JH, Kirschstein M, Kehring N, Wurster U, Volkmann A, Kulpmann WR (1993) [Proteinuria and enzymuria as leading symptoms of renal and extrarenal diseases in childhood]. Monatsschr Kinderheilkd 141:59–69
Tessin I, Trollfors B, Thiringer K, Bergmark J, Hultberg B (1988) Enzymuria in neonates during treatment with tobramycin or ceftazidime. Pediatr Infect Dis J 7:142–143
Tolins JP, Vercellotti GM, Wilkowske M, Ha B, Jacob HS, Raij L (1989) Role of platelet activating factor in endotoxemic acute renal failure in the male rat. J Lab Clin Med 113:316–324
Mariano F, Guida G, Donati D, Tetta C, Cavalli PL, Verzetti G, Piccoli G, Camussi G (1999) Production of platelet-activating factor in patients with sepsis-associated acute renal failure. Nephrol Dial Transplant 14:1150–1157
Melnikov VY, Ecder T, Fantuzzi G, Siegmund B, Lucia MS, Dinarello CA, Schrier RW, Edelstein CL (2001) Impaired IL-18 processing protects caspase-1-deficient mice from ischemic acute renal failure. J Clin Invest 107:1145–1152
Melnikov VY, Faubel S, Siegmund B, Lucia MS, Ljubanovic D, Edelstein CL (2002) Neutrophil-independent mechanisms of caspase-1- and IL-18-mediated ischemic acute tubular necrosis in mice. J Clin Invest 110:1083–1091
Parikh CR, Jani A, Melnikov VY, Faubel S, Edelstein CL (2004) Urinary interleukin-18 is a marker of human acute tubular necrosis. Am J Kidney Dis 43:405–414
Parikh CR, Mishra J, Thiessen-Philbrook H, Dursun B, Ma Q, Kelly C, Dent C, Devarajan P, Edelstein CL (2006) Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int 70:199–203
Parikh CR, Abraham E, Ancukiewicz M, Edelstein CL (2005) Urine IL-18 is an early diagnostic marker for acute kidney injury and predicts mortality in the intensive care unit. J Am Soc Nephrol 16:3046–3052
Ichimura T, Bonventre JV, Bailly V, Wei H, Hession CA, Cate RL, Sanicola M (1998) Kidney injury molecule-1 (KIM-1), a putative epithelial cell adhesion molecule containing a novel immunoglobulin domain, is up-regulated in renal cells after injury. J Biol Chem 273:4135–4142
Ichimura T, Hung CC, Yang SA, Stevens JL, Bonventre JV (2004) Kidney injury molecule-1: a tissue and urinary biomarker for nephrotoxicant-induced renal injury. Am J Physiol Renal Physiol 286:F552–563
Vaidya VS, Ramirez V, Ichimura T, Bobadilla NA, Bonventre JV (2006) Urinary kidney injury molecule-1: a sensitive quantitative biomarker for early detection of kidney tubular injury. Am J Physiol Renal Physiol 290:F517–529
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, Mori K, Barasch J, Devarajan P (2005) Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet 365:1231–1238
Mishra J, Ma Q, Prada A, Mitsnefes M, Zahedi K, Yang J, Barasch J, Devarajan P (2003) Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol 14:2534–2543
Mishra J, Mori K, Ma Q, Kelly C, Barasch J, Devarajan P (2004) Neutrophil gelatinase-associated lipocalin: a novel early urinary biomarker for cisplatin nephrotoxicity. Am J Nephrol 24:307–315
Muramatsu Y, Tsujie M, Kohda Y, Pham B, Perantoni AO, Zhao H, Jo SK, Yuen PS, Craig L, Hu X, Star RA (2002) Early detection of cysteine rich protein 61 (CYR61, CCN1) in urine following renal ischemic reperfusion injury. Kidney Int 62:1601–1610
Li B, Hartono C, Ding R, Sharma VK, Ramaswamy R, Qian B, Serur D, Mouradian J, Schwartz JE, Suthanthiran M (2001) Noninvasive diagnosis of renal-allograft rejection by measurement of messenger RNA for perforin and granzyme B in urine. N Engl J Med 344:947–954
Hu H, Aizenstein BD, Puchalski A, Burmania JA, Hamawy MM, Knechtle SJ (2004) Elevation of CXCR3-binding chemokines in urine indicates acute renal-allograft dysfunction. Am J Transplant 4:432–437
Zahedi K, Wang Z, Barone S, Prada AE, Kelly CN, Casero RA, Yokota N, Porter CW, Rabb H, Soleimani M (2003) Expression of SSAT, a novel biomarker of tubular cell damage, increases in kidney ischemia–reperfusion injury. Am J Physiol Renal Physiol 284:F1046–1055
Rector F, Goyal S, Rosenberg IK, Lucas CE (1972) Renal hyperemia in associated with clinical sepsis. Surg Forum 23:51–53
Brenner M, Schaer GL, Mallory DL, Suffredini AF, Parrillo JE (1990) Detection of renal blood flow abnormalities in septic and critically ill patients using a newly designed indwelling thermodilution renal vein catheter. Chest 98:170–179
Langenberg C, Bellomo R, May C, Wan L, Egi M, Morgera S (2005) Renal blood flow in sepsis. Crit Care 9:R363–374
Langenberg C, Wan L, Egi M, May CN, Bellomo R (2006) Renal blood flow in experimental septic acute renal failure. Kidney Int 69:1996–2002
Wan L, Bellomo R, Di Giantomasso D, Ronco C (2003) The pathogenesis of septic acute renal failure. Curr Opin Crit Care 9:496–502
Bouman CSC, Oudemans-van Straaten HM, Tijssen JGP, Zandstra DF, Kesecioglu J (2002) Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: A prospective, randomized trial. Critical Care Medicine 30:2205–2211
Oudemans-van Straaten HM, Bosman RJ, van der Spoel JI, Zandstra DF (1999) Outcome of critically ill patients treated with intermittent high-volume haemofiltration: a prospective cohort analysis. Intensive Care Med 25:814–821
Ratanarat R, Brendolan A, Piccinni P, Dan M, Salvatori G, Ricci Z, Ronco C (2005) Pulse high-volume haemofiltration for treatment of severe sepsis: effects on hemodynamics and survival. Crit Care 9:R294–302
Gettings LG, Reynolds HN, Scalea T (1999) Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early vs. late. Intensive Care Med 25:805–813
Langenberg C, Wan L, Bagshaw SM, Egi M, May CN, Bellomo R (2006) Urinary biochemistry in experimental septic acute renal failure. Nephrol Dial Transplant 21(12):3389–3397
Jung K, Schulze G, Reinholdt C (1986) Different diuresis-dependent excretions of urinary enzymes: N-acetyl-beta-D-glucosaminidase, alanine aminopeptidase, alkaline phosphatase, and gamma-glutamyltransferase. Clin Chem 32:529–532
Acknowledgements
S. M. B. is supported by Clinical Fellowships from the Canadian Institutes for Health Research and the Alberta Heritage Foundation for Medical Research. C. L. is supported by a grant from the Else Kröner-Fresenius Foundation. M. H. is supported by a Feodor Lynen Research Fellowship from the Alexander von Humboldt Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bagshaw, S.M., Langenberg, C., Haase, M. et al. Urinary biomarkers in septic acute kidney injury. Intensive Care Med 33, 1285–1296 (2007). https://doi.org/10.1007/s00134-007-0656-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0656-5