Abstract
Objective
To compare the effects of arginine-vasopressin (AVP) and norepinephrine (NE) on hemodynamic variables, organ dysfunction, and adverse events in early hyperdynamic septic shock.
Design and setting
Randomized, controlled, open-label trial.
Patients and participants
Twenty-three patients with early (12 h) hyperdynamic septic shock in two teaching hospitals.
Interventions
AVP (0.04–0.20 U min–1, n = 13) as a single agent or NE (0.1–2.8 μg kg–1 min–1, n = 10) infusion for 48 h to achieve mean arterial pressure at or above 70 mmHg.
Measurements and results
Hemodynamic parameters and Sequential Organ Failure Assessment (SOFA) score were measured. AVP and NE equally increased mean arterial pressure over 48 h, but NE was required in 36% of AVP patients at 48 h. Compared to baseline, AVP increased systemic vascular resistance, decreased exposure to NE, decreased cardiac output by decreasing heart rate, increased creatinine clearance, and improved SOFA score. The PrCO2 – PaCO2 difference remained stable throughout the study. One AVP patient developed acute coronary syndrome with dose-dependent ECG changes. Three patients in both groups died during their ICU stay.
Conclusion
In early hyperdynamic septic shock, the administration of high-dose AVP as a single agent fails to increase mean arterial pressure in the first hour but maintains it above 70 mmHg in two-thirds of patients at 48 h. AVP decreases NE exposure, has no effect on the PrCO2 – PaCO2 difference, and improves renal function and SOFA score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe sepsis is the tenth leading cause of death in the United States [1], with an incidence rate of 3.0 per 1,000 persons/year [2]. The mortality rate remains high (up to 30%) [2] and may reach 55% in septic shock [3].
Fluid management, antibiotics, source control, vasopressors, inotropes, activated protein C, and low-dose corticosteroids in selected patients are the foundations of septic shock treatment. Recently, early goal-directed therapy [4] has also figured among the most important components of initial septic shock management. However, no particular vasopressor in the early resuscitation phase of septic shock has proven to be superior in improving clinical outcome [5].
The use of exogenous arginine-vasopressin (AVP) infusion in catecholamine-refractory shock has become popular since the description of relative vasopressin depletion in patients with septic shock compared to cardiogenic shock [6]. Subsequently, vasopressin deficiency was shown to occur approx. 36 h after the onset of septic shock [7]. Uncontrolled trials and retrospective cohort studies have provided some understanding of the pharmacological effects of a replacement dose of AVP [8, 9, 10, 11, 12, 13, 14, 15, 16]. AVP has been reported to (a) increase mean arterial pressure [9, 10, 12, 13, 14, 15, 16], (b) slightly decrease [10, 11, 12, 13, 15] or maintain [12, 14] cardiac output, (c) improve short-term urine output [14, 15, 16] and creatinine clearance, (d) enhance gastric-arterial PCO2 (PrCO2 – PaCO2) difference [11, 12], and (e) decrease catecholamine requirements [13, 15, 16]. The catecholamine-sparing properties [17, 18, 19] and possible renoprotective [18] effects of AVP have also been confirmed in small randomized controlled trials [17, 18, 19], although the safety of AVP on cardiac output and splanchnic perfusion remains a matter of debate.
To date, no trial has examined the value of AVP as part of early management of hyperdynamic septic shock. The purpose of this study was therefore to evaluate the effects of AVP on mean arterial pressure, other hemodynamic variables, and organ dysfunction when used to replace norepinephrine (NE) in the early resuscitation phase of hyperdynamic septic shock.
Materials and methods
Patients
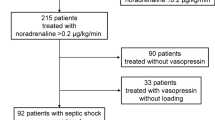
The study was performed at the Centre Hospitalier Universitaire de Sherbrooke, Hôpital Fleurimont (Sherbrooke, Canada) and the Centre Hospitalier Universitaire de Nancy, Hôpital Central, Service de Réanimation Médicale (Nancy, France) between August 2000 and June 2004. The second recruiting center experienced temporary inability to recruit because AVP was retired for intravenous use in France. Local institutional ethics committees approved the study, and informed consent was obtained from the next of kin. Patients were eligible if they (a) met criteria for septic shock [20], (b) had at some point a mean arterial pressure of 60 mmHg or less after at least a 1000-ml crystalloid bolus, (c) were on vasopressors for less than 12 h before randomization, (d) had pulmonary artery occlusion pressure of 12 mmHg or higher, and (e) had a cardiac index of 3 l min–1 m–2 or higher. If informed consent was rapidly obtained, hypotensive patients were randomized prior exposure to any vasoactive drug. Patients younger than 16 years old, receiving chronic dialysis, not expected to survive longer than 48 h, and pregnant patients were excluded.
Twenty-three patients participated in the study, 18 in Canada and 5 in France; 13 received AVP (6 men, 7 women; 51.2 ± 17.2 years old; body mass index 25.7 ± 6.7) and 10 NE (8 men, 2 women; 58.1 ± 17.5 years old, body mass index 25.0 ± 3.8; Table 1). No significant differences were observed between the study groups at randomization except for higher bilirubin levels in the AVP group, and patients enrolled in Canada and in France were also similar. One patient originally allocated to the NE group did not provide consent; because the next of kin refused to give consent for the insertion of pulmonary arterial catheter, this patient was excluded. No patients required continuous renal replacement therapy throughout the study. Eight patients in each group received corticosteroids. Although not statistically significant, patients in the AVP group (n = 5) than in the NE group (n = 2) were more often receiving chronic corticosteroids for medical reasons before randomization, while patients in the NE group (n = 6) than in the AVP group (n = 3) developed relative adrenal insufficiency within the first 24 h of septic shock. Resuscitation fluid amounts infused prior to inclusion were similar in the two groups (AVP 4.37 l, interquartile range, 2.20–4.54; NE 3.87 l, 3.22–5.72).
Protocol
A computer-generated block randomization list for each center was prepared by a pharmacist not involved in patient recruitment. Randomization was concealed using numbered, opaque sealed envelopes. Patients were allocated to open-label AVP (0.04–0.20 U/min; Ferring, Toronto, Ontario) or NE bitartrate (0.1–2.8 μg kg–1 min–1; Sabex, Boucherville, Quebec), which was infused in a central venous catheter to maintain a mean arterial pressure above 70 mmHg. Other vasopressive drugs were tapered and weaned as the experimental drug was increased. When maximal dosage of the experimental drug was reached (AVP 0.20 U min–1; NE 2.8 μg kg–1 min–1), administration of the other drug (either NE or AVP) was allowed as rescue therapy if the mean arterial pressure was still below 70 mmHg. Dobutamine was used if cardiac index decreased below 3 l min–1 m–2 despite adequate volume resuscitation. Either colloids (albumin 25%, Bayer, Toronto, Ontario; pentastarch 10%, Bristol-Myers-Squibb Canada, Montreal, Quebec) or crystalloids were used to maintain pulmonary artery occlusion pressure greater than 12 mmHg. Within 24 h after randomization an ACTH stimulation test was performed in all patients by injecting 250 μg ACTH and by measuring cortisol before and 30 and 60 min after the injection. Relative adrenal insufficiency was defined by a response of 9 μg dl–1 or less. Nonresponders and chronic corticosteroid users were treated with hydrocortisone 50 mg intravenously every 6 h for at least 1 week [21]. Antibiotic use, surgical management of infection, insulin, sedation, analgesia, transfusions, and other supportive treatments were at the discretion of the ICU team.
Hemodynamic monitoring included radial and pulmonary arterial catheters (Edwards Life Sciences, Irvine Calif., USA). Parameters were measured at 0, 1, 6, 12, 24, and 48 h after protocol initiation. Since all patients were mechanically ventilated, pressures were measured at end-expiration. Cardiac index was obtained by thermodilution. Mean cardiac index was calculated after performing three measurements with 10 ml dextrose water (5%) at room temperature (<22 °C) injected in less than 2 s. Gastric tonometry was performed after insertion of a TRIP catheter (16 F) by nasogastric route (Tonocap, Tonometrics, Datex-Omheda, Madison Wisc., USA). Enteral nutrition was not allowed for the first 24 h and was discontinued 8 h prior to the last tonometric measurement at 48 h.
Arterial blood gases, pulmonary artery blood gases, and lactate concentration were obtained for each cardiac index measurement. The PaO2/FIO2 ratio, creatinine clearance, bilirubin, platelet count, and modified Sequential Organ Failure Assessment (SOFA) score were measured at 0, 12, 24, and 48 h. Modified SOFA score was determined without considering the neurological component as all patients were sedated. While the cardiovascular component of the SOFA score considers catecholamine (but not AVP) use as a marker of organ dysfunction, additional points were prospectively assigned to AVP patients not on NE to avoid a vasopressor-selection bias (2 points if AVP infusion was at or below 0.04 U/min and 3 points if at or below 0.04 U/min). Creatinine clearance was based on 2-h urine collection.
Adverse reactions such as acute coronary syndromes, arrhythmias, clinically significant gut and skin ischemia were prospectively and systematically recorded in each group by a physician not involved in the study. Acute coronary syndrome was a priori defined as an increase in troponin I level above the normal threshold combined with electrocardiographic (ECG) changes (ST segment elevation or depression of ≥ 1 mV or a T wave inversion of ≥ 2 mV).
Statistical analysis
We respected the intention-to-treat principle by analyzing all patients according to their initial assignment. Data are expressed as mean ± SD or median with interquartile range. Normality was assessed by the Shapiro-Wilks test for each variable. Baseline characteristics were compared using the unpaired Student's t test for quantitative variables and Fisher's exact test for categorical variables. Differences within groups were analyzed by one-way analysis of variance for parametric variables. We used the Dunnett's method for comparisons with baseline when time-effect was significant. For nonparametric variables (vasoactive drugs requirements and alanine transaminase levels) we used the Kruskal-Wallis test for comparison within groups and the Mann-Whitney U test with Bonferroni's adjustment for comparisons between pairs. Differences between groups were analyzed by linear mixed-effects models to consider death-related dropouts. All comparisons with a p value less than 0.05 were considered as statistically significant.
Results
Hemodynamic parameters
Hemodynamic parameters and vasoactive drug requirements were similar at the beginning of drug infusion (Table 2). Central venous pressure, pulmonary artery occlusion pressure, and mean pulmonary artery pressure remained stable over time and were similar in each group. In both groups the mean arterial pressure increased over time and differed significantly at the end of the study compared with baseline (AVP p = 0.004, NE p = 0.02). No differences were observed between groups (p = 0.74). There was a transient decrease in cardiac index vs. baseline among patients receiving AVP, which was significant at 1, 6, and 12 h (p = 0.02) and was associated with a sustained increase in systemic vascular resistance (p = 0.002; Table 2). In addition, there was a decrease in O2 delivery at 48 h in the AVP group (p = 0.01; Table 3). There was no overall difference in cardiac index, O2 delivery, or consumption in the NE group. The NE dose was lower in the AVP group at the end of the study compared to baseline (p = 0.04; Table 4), but 85% of AVP-infused patients received NE at some point because their mean arterial pressure was less than 70 mmHg despite maximal dose of AVP (0.2 U/min). No patients in the NE group received rescue AVP therapy. Three patients in both groups required dobutamine.
Organ dysfunction
Organ dysfunction measurements are shown in Table 3. AVP patients exhibited a lower modified SOFA score at the end of the experiment than NE patients (p = 0.04). This was associated with an improvement in creatinine clearance at 24 h in the AVP group (p = 0.04) that was not observed in the NE group (p = 0.46). Baseline bilirubin levels was higher in the AVP group than the NE group (p = 0.03), but this gap remained unchanged throughout the study and was not associated with a difference in alanine transaminase levels. No difference was observed either between or within groups in terms of PrCO2 – PaCO2 difference or platelet count.
Adverse events
Overall three patients in both groups died during ICU stay (ICU mortality rate: AVP group 23.1%, NE group 30%; p = 1.00, Fisher's exact test). Three patients died during the study protocol: two in the AVP group and one in the NE group. In each case death was attributed to refractory shock. In one instance, a marked increase in PrCO2 – PaCO2 difference was observed while the patient was receiving AVP at 0.2 U/min. However, an autopsy limited to the abdomen and performed by a pathologist unaware of group assignment reported neither macroscopic nor microscopic evidence of mesenteric ischemia. No such event occurred among the other patients. No cutaneous ischemia was observed in either group.
One case of acute coronary syndrome occurred during the protocol in each group, with a maximal troponin I level of 0.8 μg/l in the AVP patient and of 0.6 μg/l in the NE patient. The latter patient had stable coronary artery disease. Coronary angiography demonstrated severe right coronary and circumflex stenosis. The AVP patient had no cardiovascular disease prior to admission, and angiography performed during infusion of AVP at 0.2 U/min revealed an occlusion of a small marginal artery. ECG changes (ST segment depression in lateral precordial leads) subsequently disappeared after tapering the AVP infusion to 0.04 U/min. None of these patients developed Q waves and creatine kinase levels remained normal. No tachyarrhythmia was observed during the first 48 h.
Discussion
In this randomized trial high-dose AVP alone did not maintain the mean arterial pressure above 70 mmHg in the early resuscitation phase of hyperdynamic septic shock in most patients. Although patients were exposed to relatively lower doses of NE, no exquisite sensitivity to AVP was observed. More than one-half of AVP-infused patients were still on NE and required the maximal dose of AVP after 1 h, and one-third were still on NE at 48 h. Patients enrolled in this trial were in septic shock for less than 12 h. Since vasopressin depletion is believed to occur 36 h from the onset of septic shock [7], enrolled patients may have not been AVP depleted. We did not measure AVP levels, and the dose used probably led to supranormal AVP levels. On the other hand, the relationship between circulating vasoactive hormones and pharmacological effects is complex. Jochberger et al. [22] recently demonstrated that there is no correlation between AVP serum levels and hemodynamic parameters in critically ill patients. Moreover, decreased AVP sensitivity, partly related to receptor downregulation [23], has recently been demonstrated during septic shock [24].
However, this trial demonstrates that the infusion of AVP, in contrast to NE, improves SOFA scores in early septic shock. Rapid improvement in SOFA score has been associated with lower mortality rates [25, 26, 27]. More specifically, improvement in renal dysfunction from baseline to day 1 is an independent predictor of 28-day survival [25]. In this trial improved SOFA score in AVP-treated patients was due mainly to its effect on renal function. Vasopressin-induced favorable effects on renal function have previously been reported in a randomized double-blind trial [18] and are supported by experimental data [28]. AVP increases renal blood flow in endotoxic animals [28, 29] independently of its effect on mean arterial pressure [18, 29]. Unlike NE, AVP exhibits selective vasoconstrictive properties on the efferent arteriole [30] and vasodilatory effects on the afferent arteriole which are thought to be related to nitric oxide production [31]. As for NE, this overall effect on renal microperfusion can be blunted by using higher doses of AVP [32].
AVP increased systemic vascular resistance and was a valuable NE-sparing agent. It decreased cardiac index by lowering heart rate rather then stroke volume. It also reduced O2 delivery without affecting mixed venous oxygen saturation or lactate levels. These results are consistent with those of Albanèse et al. [33], who used 1 mg terlipressin, a AVP analog with 6-h half-life. Three small randomized trials [17, 18, 19] found no adverse effect of AVP on cardiac output, in opposition to case series [11, 12, 13, 15]. Luckner et al. [8] recently reported decreased cardiac index induced by AVP mainly in patients with hyperdynamic circulation, as was the case in our patients. On contrast to to Holmes et al. [15], who used AVP a dose as high as 0.6 U/min in some cases, no life-threatening decrease in cardiac index was observed after initiation of high-dose AVP in this trial. On the other hand, one patient developed AVP-induced acute coronary syndrome, although ischemic ECG changes disappeared upon reduction in the amount of AVP infused, which is consistent with dose-dependent coronary vasoconstriction observed in experimental models [34, 35].
As opposed to Luckner et al. [8], we did not find that AVP impaired liver function by inducing cholestasis and increasing liver enzymes. No PrCO2 – PaCO2 difference deterioration was observed, as opposed to the findings of Klinzing et al. [11] who used similar AVP doses previously described to reduce bleeding from ruptured esophageal varices [36] (mean dose 0.47 /min, maximal 1.8 U/min). In this respect our results confirm those observed previously in two randomized controlled trials [17, 18]. Furthermore, deleterious effects of AVP on splanchnic perfusion may be explained by inadequate fluid resuscitation [37].
Even with large doses of AVP mean pulmonary artery pressure and resistance did not change over time in this trial compared to those in the NE group. Animal experiments demonstrate that low-dose AVP, which activates endothelial isoforms of nitric oxide synthase via endothelial oxytocin receptors [38], induces pulmonary vasodilatation [39] and decreases lung hyperpermeability induced by endotoxin [28]. The former effect is not sustained with higher levels of AVP (>300 pg/ml) [40], whereas recent clinical data show that an AVP dose of 0.04–0.1 U/min does not change or slightly decreases pulmonary artery pressure [13, 14, 15, 17], in contrast to terlipressin which enhances it [33].
To our knowledge, this is the first trial evaluating the effects of AVP infusion in the first 12 h of hyperdynamic septic shock. Previous trials used AVP as a rescue therapy for refractory septic shock [17, 18, 19] or after equivocal delay from sepsis onset [11]. This study has several limitations. The unblinded design may have introduced confounders and affected measurements despite the fact that many measured variables are not prone to subjective interpretation. Also, the small sample size precludes definitive conclusions about the potential effect of AVP on clinically important benefits (such as less need for renal replacement or lower mortality suggested by improved renal function and SOFA scores) or clinically important harms (such as splanchnic and coronary adverse effects).
Conclusion
This multicenter, open-label randomized trial in early hyperdynamic septic shock found that initial management with high-dose AVP used as a single vasopressor agent initially failed to maintain the mean arterial pressure above 70 mmHg. Nevertheless AVP is a NE-sparing agent that decreases cardiac index mainly by decreasing heart rate rather then cardiac contractility. AVP may have favorable effects on renal function that translate into a lower modified SOFA score at 48 h. Although not designed to comprehensively assess gastrointestinal effects, no deterioration in the PrCO2 – PaCO2 difference was observed in the AVP group. Before becoming a standard of care in the management of early hyperdynamic septic shock, AVP needs to be further evaluated in a large double-blind randomized controlled trial to determine its effects on overall morbidity and mortality.
References
Hoyert DL, Kung HC, Smith BL (2005) Deaths: preliminary data for 2003. Natl Vital Stat Rep 53:1–48
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D (2006) Sepsis Occurrence in Acutely Ill Patients Investigators. Crit Care Med 34:344–353
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, for the Early Goal-Directed Therapy Collaborative Group (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Müllner M, Urbanek B, Havel C, Losert H, Waechter F, Gamper G (2004) Vasopressors for shock. Cochrane Database of Systematic Reviews, issue 3: CD003709
Landry DW, Levin HR, Gallant EM, Ashton RC Jr, Seo S, D'Alessandro D, Oz MC, Oliver JA (1997) Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation 95:1122–1125
Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D (2003) Circulating vasopressin levels in septic shock. Crit Care Med 31:1752–1758
Luckner G, Dunser MW, Jochberger S, Mayr VD, Wenzel V, Ulmer H, Schmid S, Knotzer H, Pajk W, Hasibeder W, Mayr AJ, Friesenecker B (2005) Arginine vasopressin in 316 patients with advanced vasodilatory shock. Crit Care Med 33:2659–2666
Hall LG, Oyen LJ, Taner CB, Cullinane DC, Baird TK, Cha SS, Sawyer MD (2004) Fixed-dose vasopressin compared with titrated dopamine and norepinephrine as initial vasopressor therapy for septic shock. Pharmacotherapy 24:1002–1012
Obritsch MD, Jung R, Fish DN, MacLaren R (2004) Effects of continuous vasopressin infusion in patients with septic shock. Ann Pharmacother 38:1117–1122
Klinzing S, Simon M, Reinhart K, Bredle DL, Meier-Hellmann A (2003) High-dose vasopressin is not superior to norepinephrine in septic shock. Crit Care Med 31:2646–2650
Haren FMP van, Rozendaal FW, van der Hoeven JG (2003) The effect of vasopressin on gastric perfusion in catecholamine-dependent patients in septic shock. Chest 124:2256–2260
Dunser MW, Mayr AJ, Ulmer H, Ritsch N, Knotzer H, Pajk W, Luckner G, Mutz NJ, Hasibeder WR (2001) The effects of vasopressin on systemic hemodynamics in catecholamine-resistant septic and postcardiotomy shock: a retrospective analysis. Anesth Analg 93:7–13
Tsuneyoshi I, Yamada H, Kakihana Y, Nakamura M, Nakano Y, Boyle WA (2001) Hemodynamic and metabolic effects of low dose vasopressin infusions in vasodilatory septic shock. Crit Care Med 29:487–493
Holmes CL, Walley KR, Chittock DR, Lehman T, Russell JA (2001) The effects of vasopressin on hemodynamics and renal function in severe septic shock: a case series. Intensive Care Med 27:1416–1421
Landry DW, Levin HR, Gallant EM, Seo S, D'Alessandro D, Oz MC, Oliver JA (1997) Vasopressin pressor hypersensitivity in vasodilatory septic shock. Crit Care Med 25:1279–1282
Dunser MW, Mayr AJ, Ulmer H, Knotzer H, Sumann G, Pajk W, Friesenecker B, Hasibeder WR (2003) Arginine vasopressin in advanced vasodilatory shock: a prospective, randomized, controlled study. Circulation 107:2313–2319
Patel BM, Chittock DR, Russell JA, Walley KR (2002) Beneficial effects of short-term vasopressin infusion during severe septic shock. Anesthesiology 96:576–582
Malay MB, Ashton RC Jr, Landry DW, Townsend RN (1999) Low-dose vasopressin in the treatment of vasodilatory septic shock. J Trauma 47:699–703
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, Chaumet-Riffaut P, Bellissant E (2002) Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288:862–871
Jochberger S, Mayr VD, Luckner G, Wenzel V, Ulmer H, Schmid S, Knotzer H, Pajk W, Hasibeder W, Friesenecker B, Mayr AJ, Dünser MW (2006) Serum vasopressin concentrations in critically ill patients. Crit Care Med 34:293–299
Bucher M, Hobbhahn J, Taeger K, Kurtz A (2002) Cytokine-mediated down-regulation of vasopressin V1A receptors during acute endotoxemia in rats. Am J Physiol Regul Integr Comp Physiol 282:R979–R984
Leone M, Boyle WA (2006) Decreased vasopressin responsiveness in vasodilatory septic shock-like conditions. Crit Care Med 34:1126–1130
Levy MM, Macias WL, Vincent JL, Russell JA, Silva E, Trzaskoma B, Williams MD (2005) Early changes in organ function predict eventual survival in severe sepsis. Crit Care Med 33:2194–2201
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Moreno R, Vincent JL, Matos R, Mendonca A, Cantraine F, Thijs L, Takala J, Sprung C, Antonelli M, Bruining H, Willatts S (1999) The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Intensive Care Med 25:686–696
Lévy B, Vallée C, Lauzier F, Plante GE, Mansart A, Mallie JP, Lesur O (2004) Comparative effects of vasopressin, norepinephrine, and L-canavanine, a selective inhibitor of inducible nitric oxide synthase, in endotoxic shock. Am J Physiol Heart Circ Physiol 287:H209–H215
Albert M, Losser MR, Hayon D, Faivre V, Payen D (2004) Systemic and renal macro- and microcirculatory responses to arginine vasopressin in endotoxic rabbits. Crit Care Med 32:1891–1898
Edwards RM, Trizna W, Kinter LB (1989) Renal microvascular effects of vasopressin and vasopressin antagonists. Am J Physiol 256:F274–F278
Rudichenko VM, Beierwaltes WH (1995) Arginine vasopressin-induced renal vasodilation mediated by nitric oxide. J Vasc Res 32:100–105
McVicar AJ (1988) Dose-response effects of pressor doses of arginine vasopressin on renal haemodynamics in the rat. J Physiol (Lond) 404:535–546
Albanese J, Leone M, Delmas A, Martin C (2005) Terlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized study. Crit Care Med 33:1897–1902
Boyle WA III, Segel LD (1986) Direct cardiac effects of vasopressin and their reversal by a vascular antagonist. Am J Physiol 251:H734–H741
Walker BR, Childs ME, Adams EM (1988) Direct cardiac effects of vasopressin: role of V1- and V2-vasopressinergic receptors. Am J Physiol 255:H261–H265
Imperiale TF, Teran JC, McCullough AJ (1995) A meta-analysis of somatostatin versus vasopressin in the management of acute esophageal variceal hemorrhage. Gastroenterology 109:1289–1294
Asfar P, Pierrot M, Veal N, Moal F, Oberti F, Croquet V, Douay O, Gallois Y, Saumet JL, Alquier P, Cales P (2003) Low-dose terlipressin improves systemic and splanchnic hemodynamics in fluid-challenged endotoxic rats. Crit Care Med 31:215–220
Thibonnier M, Conarty DM, Preston JA, Plesnicher CL, Dweik RA, Erzurum SC (1999) Human vascular endothelial cells express oxytocin receptors. Endocrinology 140:1301–1309
Okamura T, Toda M, Ayajiki K, Toda N (1997) Receptor subtypes involved in relaxation and contraction by arginine vasopressin in canine isolated short posterior ciliary arteries. J Vasc Res 34:464–472
Wallace AW, Tunin CM, Shoukas AA (1989) Effects of vasopressin on pulmonary and systemic vascular mechanics. Am J Physiol 257:H1228–H1234
Acknowledgements
The authors thank Dr. Deborah Cook for reviewing the manuscript and Drs. Julie Abel, Dominique Bérard, Claude Cyr, Eric Deland, Sophie Laflamme, Marcel Martin, and Catherine St-Pierre for their help in recruiting patients.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Cardiovascular Critical Care research Network FRSQ and departmental funding.
Rights and permissions
About this article
Cite this article
Lauzier, F., Lévy, B., Lamarre, P. et al. Vasopressin or norepinephrine in early hyperdynamic septic shock: a randomized clinical trial. Intensive Care Med 32, 1782–1789 (2006). https://doi.org/10.1007/s00134-006-0378-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0378-0