Abstract
Objective
To analyze the costs of treating critically ill patients.
Design and setting
Multicenter, observational, prospective, cohort, bottom-up study on variable costs in 51 ICUs.
Patients and participants
A total of 1,034 patients aged over 14 years who either spent less than 48 h in the ICU or had multiple trauma, major abdominal surgery, ischemic stroke, chronic obstructive pulmonary disease, cardiac failure, isolated head injury, acute lung injury/adult respiratory distress syndrome (ALI/ARDS), nontraumatic intracranial hemorrhage or coronary surgery.
Interventions
Data recorded for each patient: length of ICU stay, and cost in euros of all diagnostic and therapeutic procedures, drugs and equipment used, and consultations by physicians from other units. To express cost-efficiency we calculated for each diagnostic group the cost per surviving patient (expenditure for all patients/number of surviving patients) and money loss per patient (expenditure for patients who died/total number of patients).
Measurements and results
Median costs for a multiple trauma patient were €4076 and for coronary surgery patient €380. The variability is largely due to different lengths of ICU stay. Cost per surviving patient was higher for ALI/ARDS, nontraumatic intracranial hemorrhage, multiple trauma, and emergency abdominal surgery. Money loss per patient was higher for ALI/ARDS and lower for multiple trauma. Planned coronary and major abdominal surgery and short-stay patients were treated most cost-efficiently.
Conclusions
Cost of treatment in an ICU varies widely for different types of patients. Strategies are needed to contain the major determinants of high costs and low cost-efficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cost containment is an important and demanding challenge in healthcare [1]. Concerns about costs also apply to critical care, which absorbs a large proportion of total hospital expenditure [2, 3, 4]. Cost issues cannot be dealt with properly unless both clinical and economical aspects of treating patients are considered [5]. Little is known about the factors affecting variability in patient-specific costs [2]. A Medline search over 2000–2004 for papers with major topic heading of “costs and cost analysis” and “critical care” yields only 46 reports, most of which are editorials, position papers, cost-effectiveness analyses of specific interventions, or papers on costs averaged across all patients or pertaining to intensive care unit (ICU) as a whole.
There are two approaches for determining costs: the “top-down” and the “bottom-up” methods [6]. The top-down approach calculates the average cost per patient or per patient-day by dividing total annual budget plus overheads for the entire ICU by the number of patients or patient-days [6, 7]. Although this method is straightforward, it is unsuitable for certain types of evaluations, as it assumes that expenditure of resources is the same for all patients, which is clearly unrealistic particularly in ICUs [8]. The bottom-up approach adds up costs of all items used for each patient [6, 7]. This facilitates economic evaluation of ICU resources but is time-consuming and expensive since it requires extensive data recording and accurate data-to-money conversion. Economic information useful for clinical decisions can only stem from multicenter bottom-up studies aimed at determining factors that affect patient-specific costs.
The present contribution reports the findings of a bottom-up study that comprised part of a multiannual project on costs in critical care carried out by the Gruppo Italiano per la Valutazione degli Interventi in Terapia Intensiva (GiViTI; Italian Group for the Evaluation of Interventions in Intensive Care Medicine) [9, 10]. The main aims of this study were: to identify the most important cost drivers in ICU to describe and compare the costs of treating different types of patients; to validate the Nine Equivalents of Nursing Manpower Use Score (NEMS) [11] and diagnosis-related-group. We here report the results of the first two of these aims.
Methods and materials
Fifty-one ICUs belonging to the GiViTI network took part in this observational, prospective cohort study. For each patient enrolled cost of care received was calculated as shown below. Between 1999 and 2000 a total of 1,034 patients were enrolled.
Data collection
A case record form was developed and validated by means of three independent data collection campaigns in samples of 2, 3, and 29 ICUs. Detailed data were collected regarding ICU admission and discharge (including diagnosis-related-group) and daily information about diagnostic and therapeutic procedures (including NEMS), drugs and equipment used, consultancies from other departments. For drugs we recorded the amount given and consumed, the former being the dose actually given to the patient and the latter as the sum of this plus any drug wasted or discarded. We limited data collection to resources costing more than €25 per week. Daily information was gathered until ICU discharge or for a maximum of 21 days.
Data were collected for patients above 14 years of age either (a) spending less than 48 h in the ICU or (b) with any of the following on admission: multiple trauma, major abdominal surgery, ischemic stroke, chronic obstructive pulmonary disease (COPD), cardiac failure, isolated head trauma, acute lung injury or acute respiratory distress syndrome (ALI/ARDS), nontraumatic intracranial hemorrhage, or coronary bypass. These are the most frequent admission categories reported in previous GiViTI studies [12]. The rationale for considering short-stay patients as a group by itself was that costs for them are more homogeneous, and the main source of variability would be illness severity, which in this circumstance is well represented by vital status at ICU discharge.
Each ICU was asked to enroll: (a) 5–10 consecutive patients staying less than 48 h plus (b) 5–10 consecutive patients from at least two of the above diagnostic groups. In this way each ICU enrolled 15–30 patients. Since each diagnostic group was simultaneously entrusted to ten ICUs, we expected 50–100 patients for each diagnostic group and about 500 patients with an ICU stay shorter than 48 h. During data collection, age, gender, diagnosis, dates of ICU admission and discharge, and ICU outcome were also collected for all nonenrolled patients admitted to participating ICUs to standardize overall estimates (see below). The expected number of patients was enrolled in almost all diagnostic groups (Table 1).
A number of validity checks were carried out concurrently during data entry by our computer-based case record form. These checks were of four sorts: inconsistency per se (e.g., wrong date), inconsistency relative to other variables (e.g., gynecological interventions in males), implausibility per se (e.g., less than 500 mg amoxicillin per day), implausibility relative to other variables (e.g., 1-day mechanical ventilation in ALI/ARDS patients with longer stay). The system refrained from saving inconsistent data, while keeping implausible data after user confirmation. Data were also reviewed by the coordinating center, and doubts were discussed with the individual ICUs. Most of the queries concerned patients with outlier costs. If confirmed as outliers, these patients were kept in the analysis.
Costing strategy
The monetary cost of each item considered was recorded. Drug costs were one-half retail prices (which is what hospitals are charged in Italy). The 2000 national price list provided by the Ministry of Health was used to cost laboratory and imaging tests. For all the other 235 items ICUs were asked to provide the prices actually paid in 2000. Since only 32 ICUs (63%) were able to provide these, we calculated the mean price for each item from the available data and applied this to all ICUs. In some cases (21.9%) such as pulmonary artery catheters we found outliers (ICUs paying disproportionately high prices compared to others). When this happened and the data were not corrected after the proper query, we computed trimmed means.
We then subdivided the cost structure for each single patient into seven headings: drugs, where the cost was related to the quantity consumed; nutrition, excluding nutritional devices; infusions, including blood and blood products; consumables, including nutritional devices, catheters, and all kinds of kits (e.g., for ventilation, dialysis); imaging; laboratory tests; and consultations from other intra- or extrahospital departments.
Statistical analyses
Patients enrolled in each diagnostic group were fully representative of the population belonging to that group, but the data collection design meant that the relative sizes of the groups were not representative of the overall population admitted to the ICUs. For example, our protocol yielded the same number of patients with nontraumatic intracranial hemorrhage and with major abdominal surgery, while the former are much rarer than the latter in a general ICU population. Therefore for estimates referring to the overall population we could not simply add what we had obtained in the patients collected because this would have overweighted the contribution of rarer diagnostic groups. To remove this bias data were directly standardized to the diagnostic group structure of the overall population admitted [13].
By this fundamental epidemiological approach we expected the standardized description of the present population to be similar to an independent sample of patients admitted to Italian ICUs [12]. This was actually true (data not shown), giving evidence of the validity of the process. All estimates that refer to the overall population were thus standardized, while estimates that refer to individual diagnostic groups were left as crude parameters. Since patients undergoing major abdominal surgery can differ widely depending upon the type of intervention, we split this group into scheduled and unscheduled abdominal surgery.
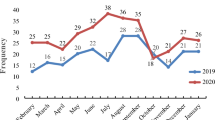
To better describe the financial burden of the various diagnostic groups of patients we developed two further measures: cost per surviving patient, i.e., money spent for all patients divided by the number of patients who survived, and money loss per patient, i.e., money spent for patients who died divided by the total number of patients. These two measures were plotted together yielding a graph of the efficiency of resource consumption.
Categorical and ordinal variables are presented as percentages and continuous variables as mean and standard deviation. Multiple regression analysis using a step-by-step backward approach was used to identify independent predictors of the cost per patient. All available patient characteristics were entered into the model. The backward approach compared different models by the likelihood ratio test, using 0.05 as the threshold of statistical significance. Collinearity, i.e., interrelationship between independent variables, was assessed using variance inflation factors (VIF) and condition number (CN) [14]. A VIF greater than 10 or a CN greater than 30 was considered suggestive of moderate to severe collinearity, a problem that could affect the accuracy of regression calculations. Normality and homoscedasticity of the dependent variable distribution were assessed by the normal probability plot and Spearman's correlation coefficient between predicted and absolute values of residuals, using data transformation, where appropriate. Data were analyzed by the SAS system 8.02.
Results
As expected, we found wide variability in variable costs, both within and between diagnostic groups (Fig. 1). The mean cost of treating a multiple trauma patient was €4717 and that for a coronary bypass surgery was €576. Much of the variability was due to the difference in the length of stay (LOS), and therefore daily costs vary much less (Fig. 2). Table 1 shows different variable costs for each diagnostic group, ICU mortality and LOS.
Fig. 3 plots the two measures: cost per surviving patient and money loss per patient. Cost per surviving patient was higher in ALI/ARDS, nontraumatic intracranial hemorrhage, multiple trauma, and unscheduled major abdominal surgery, but these conditions differed widely in terms of money loss per patient, which was higher for ALI/ARDS and lower for multiple trauma. Coronary bypass, scheduled major abdominal surgery, and short-stay patients were treated most cost-efficiently.
Two-dimensional representation of the relative cost of treating different conditions in terms of cost per surviving patient and money loss per patient. Vertical, horizontal lines First and third quartiles of costs per surviving patient and money loss per patient. Row A The most expensive conditions (per surviving patient); row C least expensive conditions; column 1 most efficiently treated conditions; column 3 least efficiently treated conditions. The challenge is to shift diseases from the top to the bottom of the graph, and from right to left. COPD Chronic obstructive pulmonary disease; ALI/ARDS acute lung injury or acute respiratory distress syndrome; LOS length of stay
Log-transformation of the cost was adopted to fulfill the normality and homoscedasticity assumptions for the linear regression model (Table 2). Eight variables proved to be significantly correlated with variable costs: diagnostic group, Simplified Acute Physiology Score II (SAPS-II), coma on admission, sepsis classification, length of ICU stay, respiratory failure on admission, cardiac failure on admission, and vital status at ICU discharge. The latter was important only for patients staying less than 48 h. VIF and CN ruled out collinearity. The correlation coefficient was 0.71 (p < 0.0001). Having adopted the log-transformation, the exponential of β for dichotomous variables corresponds to the relative increment in costs. For example, patients with respiratory failure on admission cost about 19% more than patients without failure, other covariates in the model being the same.
Discussion
This multicenter study took the bottom-up approach for estimating costs. No bottom-up study, to our knowledge, has collected data on a sample as large as ours. To make this feasible we restricted the analysis to the costs related to resources consumed at bedside. This means that we took into account only direct variable costs. Direct costs are those fully attributable to a single patient and not shared by more than one, while variable costs are those affected by the level of activity during the period considered [6]. Thus personnel costs were considered fixed since they are not affected by the level of activity required by patients during the study period. This can be seen as a limitation, particularly considering that personnel costs account for up to 60% of ICU costs [15]. However, we were interested mainly in studying the cost drivers that are under direct and exclusive control of intensive care staff itself. Staff size and salaries were therefore not considered.
Our results show how widely costs can differ across ICU patient groups. Much of this variability is due to differences in length of ICU stay, but many other cost drivers play a role, even after adjusting for LOS. The two new measures of costs, cost per surviving patient and money loss per patient, especially when considered together, gave a better picture of the financial burden of each disease entity.
These kinds of measures are not to be confused with the outputs of classical economic evaluation studies (i.e., cost-minimization, cost-effectiveness, cost-benefit, or cost-utility analysis) where the focus is on comparison of alternative courses of treatment [16]. Here we limited the analysis to the efficiency of treatments. Thus, as shown in Fig. 3, diseases in row A are the most expensive (per surviving patient) while those in row C involve lower costs. Similarly, diseases in column 1 are those most efficiently treated and those in column 3 the most inefficiently treated. The challenge is therefore to shift diseases from the top to the bottom of the graph, and from right to left.
Obviously much of this challenge depends on research, which should strive to provide more effective treatments, if possible inexpensive ones. However, clinicians have a key role as well. To move a disease from top to bottom, waste of resources should be minimized by more cost-conscious use of expensive ones. This seems especially important for patients with ALI/ARDS, nontraumatic intracranial hemorrhage, multiple trauma, and unscheduled major abdominal surgery. These results are in agreement with reports in the literature [17]. Analysis of the cost structure (Table 1) helps to indicate the best strategy for this task. Thus when treating ALI/ARDS close attention should be paid to laboratory tests and drugs; for nontraumatic intracranial hemorrhage patients laboratory tests and imaging are the most important items, while in multiple trauma and unscheduled major abdominal surgery patients laboratory tests and infusions (including blood and blood products) call for highest priority.
To move a disease from right to left, apart from improving the general effectiveness of treatment (especially for ALI/ARDS, nontraumatic intracranial hemorrhage, and unscheduled major abdominal surgery) better awareness of a poor prognosis needs to be stressed. This implies avoiding the admission of patients who are too ill and all forms of treatment obstinacy. The short LOS of patients who died compared with surviving ones for nontraumatic intracranial hemorrhage and isolated head trauma suggests that selection can be improved. The longer LOS for COPD and ALI/ARDS patients may indicate the need for continuous assessment of the patient's prognosis to prevent useless obstinacy. Nevertheless, although the idea that early identification of terminally ill patients who can be transferred to less expensive settings is intuitively appealing, many authors argue that it would not reduce costs [18].
Our multivariate model identified numerous factors that explain the variability in costs: ICU LOS, diagnostic group, SAPS II score, presence and severity of sepsis, respiratory failure, cardiac failure, and coma upon admission. That the length of stay affects patient costs is obvious [8]. We confirmed this in a multivariate analysis, which further stresses the importance, at least from the perspective of costs, of prompt detection and appropriate treatment of long-stay patients.
Diagnostic group is another important determinant of costs. Multiple trauma, isolated head trauma, nontraumatic intracranial hemorrhage, ALI/ARDS, and unscheduled major abdominal surgery were the most expensive patient groups in the multivariate model. Since the model includes many covariates, including LOS, septic complications, and severity of illness, this result possibly reflects either a more aggressive approach, specifically adopted in these patients, or the use of costly treatments. When costs are mainly related to consumables and laboratory tests, the former hypothesis is probably true. This happens in ALI/ARDS, isolated head trauma, and nontraumatic intracranial hemorrhage (Table 1). When costs are explained mainly by infusions and drugs, the latter is more likely. This is the case in multiple trauma, unscheduled major abdominal surgery, and ALI/ARDS (Table 1). This provides another clue for a more conscious use of resources.
As expected, patients who stay in ICUs less than 48 h cost the least, particularly if they survive, as testified by the positive interaction between outcome and LOS less than 48 h. Apart from coma, all the other variables in the model representing the severity of the patient tell us that the greater the severity, the higher the costs. Similar results are reported elsewhere [17, 19, 20, 21].
Two considerations seem particularly noteworthy. First, although significant, SAPS II is not crucial in determining the cost of ICU patients. The second consideration refers to the classification of sepsis. The concept of systemic inflammatory response syndrome, which has been criticized from a clinical perspective [22], seems relevant from an economic point of view, as it increases costs by 150%. The results on sepsis (which doubled costs) and severe sepsis or septic shock (which tripled costs) are also important and, together with findings by others [23], call for further effective prevention and appropriate treatment of such conditions [24].
Coma deserves a final comment: why do patients admitted with coma cost less than those admitted without coma? Other studies with an approach different from that taken here have also found this [17]. In all groups considered coma is a strong negative prognostic factor. One possible explanation is that it is easier to withhold treatment for comatose patients. Again, this calls for a better prognostic evaluation of all patients to avoid obstinacy and wastes.
A potential limitation of our study derives from the application of the same average cost per item to all ICUs. If, for example, a drug is cheap in an ICU but expensive otherwise, the use of this drug in the ICU may be improperly viewed as technically inefficient. In a simulation study which always replaced resources becoming expensive by cheaper alternatives, Raikou et al. [25] found that the calculation based on the use of average costs, as opposed to center-specific costs, systematically overestimated treatment costs. This is of course diluted in the real world, where switching to the cheapest alternative is not always done [26], and we therefore considered it relatively unimportant in our analyses. Furthermore, the aim of the present study was not to compare the technical efficiency of different ICUs nor to carry out a cost-effectiveness analysis nor to provide “true” estimates of treatment costs. We were interested in describing and comparing costs of different diagnostic groups of patients. In this sense, since a similar bias exists in all groups, its impact on the differences between groups and on the relative importance of factors influencing costs should be small. Thus, although single cost estimates from our study may not necessarily apply to other situations, the message behind the differences we identified is clear.
Another potential limitation is related to the inclusion criteria, which left out some types of patients. From the list of nonenrolled patients we saw that the eligibility criteria which we adopted covered 83% of admissions. Clearly, the exclusions may have influenced only the estimates referring to the overall population, which are in fact the results of the multivariate model. Since there are a few atypical conditions, at least from the costing perspective, that were excluded from our study (e.g., transplant patients), interpretation of the results should take this into account.
According to the design, each of the nine types of conditions considered was enrolled by at least ten ICUs, and short-stay patients were collected by all ICUs. This further enhances the general applicability of the results. However, since comparable studies are lacking in the literature, it is difficult to say how far our findings apply to other countries. Nevertheless, the key messages could easily be validated and possibly refined by single ICUs. This would be an important contribution to more efficient management of ICUs and, possibly, of ICU patients too.
References
Guyatt G, Yalnizyan A, Devereaux PJ (2002) Solving the public health care sustainability puzzle. Can Med Assoc J 167:36–38
Heyland DK, Kernerman P, Gafni A, Cook DJ (1996) Economic evaluations in the critical care literature: do they help us improve the efficiency of our unit? Crit Care Med 24:1591–1598
Bloomfield E (2003) The impact of economics on changing medical technology with reference to critical care medicine in the United States. Anesth Analg 96:418–425
Weber RJ, Kane SL, Oriolo VA, Saul M, Skledar SJ, Dasta JF (2003) Impact of intensive care unit (ICU) drug use on hospital costs: a descriptive analysis, with recommendations for optimizing ICU pharmacotherapy. Crit Care Med 31:S17–S24
Heyland DK, Gafni A, Kernerman P, Keenan S, Chalfin D (1999) How to use the results of an economic evaluation. Crit Care Med 27:1195–1202
Jegers M, Edbrooke DL, Hibbert CL, Chalfin DB, Burchardi H (2002) Definitions and methods of cost assessment: an intensivist's guide. ESICM section on health research and outcome working group on cost effectiveness. Intensive Care Med 28:680–685
Gyldmark M (1995) A review of cost studies of intensive care units: problems with the cost concept. Crit Care Med 23:964–972
Jacobs P, Edbrooke D, Hibbert C, Fassbender K, Corcoran M (2001) Descriptive patient data as an explanation for the variation in average daily costs in intensive care. Anaesthesia 56:643–647
Brazzi L, Bertolini G, Arrighi E, Rossi F, Facchini R, Luciani D (2002) Top-down costing: problems in determining staff costs in intensive care medicine. Intensive Care Med 28:1661–1663
Bertolini G, Rossi C, Brazzi L, Radrizzani D, Rossi G, Arrighi E, Simini B (2003) The relationship between labour cost per patient and the size of intensive care units: a multicentre prospective study. Intensive Care Med 29:2307–2311
Reis Miranda D, Moreno R, Iapichino G (1997) Nine equivalents of nursing manpower use score (NEMS). Intensive Care Med 23:760–765
Bertolini G, D'Amico R, Apolone G, Cattaneo A, Ravizza A, Iapichino G, Brazzi L, Melotti RM (1998) Predicting outcome in the intensive care unit using scoring systems: is new better? A comparison of SAPS and SAPS II in a cohort of 1:393 patients. GiViTi Investigators (Gruppo Italiano per la Valutazione degli interventi in Terapia Intensiva). Simplified Acute Physiology Score. Med Care 36:1371–1382
Rothman KJ, Greenland S (1998) Modern epidemiology, 2nd edn. Lippincott, Philadelphia
Kleinbaum D, Kupper L, Muller K (1988) Applied regression analysis and other multivariable methods. PWS-KENT, Boston
Edbrooke DL, Ridley SA, Hibbert CL, Corcoran M (2001) Variations in expenditure between adult general intensive care units in the UK. Anaesthesia 56:208–216
Drummond M, O'Brien B, Stoddart G, et al (1997) Methods for the economic evaluation of health care programmes, 2nd edn. Oxford University Press, New York
Sznajder M, Aegerter P, Launois R, Merliere Y, Guidet B, CubRea (2001) A cost-effectiveness analysis of stays in intensive care units. Intensive Care Med 27:146–153
Luce JM, Rubenfeld GD (2002) Can health care costs be reduced by limiting intensive care at the end of life? Am J Respir Crit Care Med 165:750–754
Stevens VG, Hibbert CL, Edbrooke DL (1998) Evaluation of proposed casemix criteria as a basis for costing patients in the adult general intensive care unit. Anaesthesia 53:944–950
Edbrooke DL, Stevens VG, Hibbert CL, Mann AJ, Wilson AJ (1997) A new method of accurately identifying costs of individual patients in intensive care: the initial results. Intensive Care Med 23:645–650
Ridley S, Biggam M, Stone P (1994) A cost-utility analysis of intensive therapy. II: Quality of life in survivors. Anaesthesia 49:192–196
Vincent JL (1997) Dear SIRS, I'm sorry to say that I don't like you. Crit Care Med 25:372–374
Moerer O, Schmid A, Hofmann M, Herklotz A, Reinhart K, Werdan K, Schneider H, Burchardi H (2002) Direct costs of severe sepsis in three German intensive care units based on retrospective electronic patient record analysis of resource use. Intensive Care Med 28:1440–1446
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150
Raikou M, Briggs A, Gray A, McGuire A (2000) Centre-specific or average unit costs in multi-centre studies? Some theory and simulation. Health Econ 9:191–198
Conti G, Dell'Utri D, Pelaia P, Rosa G, Cogliati AA, Gasparetto A (1998) Do we know the costs of what we prescribe? A study on awareness of the cost of drugs and devices among ICU staff. Intensive Care Med 24:1194–1198
Acknowledgements
The complete list of participants in the Gruppo Italiano per la Valutazione degli Interventi in Terapia Intensiva is as follows: Barberis Bruno, Rivoli; Biancofiore Gianni, Pisa; Carnevale Livio, Pavia; Cesaro Paolo, Giugliano in Campania; Ciceri Gabriella, Desio; Ciceri Rita, Lecco; Cirillo Francesco Maria, Legnago; Del Sarto Paolo, Massa; Digito Antonio, Vicenza; Doldo Giuseppe, Reggio Calabria; Franco Gabriele, Castellana Grotte; Fulgenzi Giuliano, Pesaro; Garelli Alberto, Ravenna; Giannoni Stefano, Empoli; Gorietti Adonella, Perugia; Guadagnucci Alberto, Massa; Lagomarsini Ginetta, Pisa; Lavacchi Luca, Pistoia; Maitan Stefano, Faenza; Malacarne Paolo, Pisa; Mancinelli Annetta, Chieti; Mantovani Giorgio, Ferrara; Marafon Silvio, Vicenza; Marcora Barbara, Monza; Melis Piergiorgio, Lucca; Muttini Stefano, Vimercate; Negri Giovanni, Pavia; Neri Massimo, Bologna; Paternesi Nazareno, Macerata; Pecunia Laura, Genova; Pennacchioni Silvio, Ancona; Pergolo Augusto, Genua; Pessina Carla, Rho; Postiglione Maurizio, Naples; Quattrocchi Pasqualino, Catania; Radrizzani Danilo, Legnago; Rossi Giancarlo, Livorno; Rotelli Stefano, Milano; Salvi Giovanni, Imperia; Segala Vincenzo, Torino; Siviero Silvano, Rovigo; Solinas Giommaria, Lanusei; Spadini Elisabetta, Parma; Tavola Mario, Lecco; Terragni Pierpaolo, Torino; Todesco Livio, Cittadella; Trivella Patrizia, Bergamo; Visconti Maria Grazia, Cernusco sul Naviglio; Zanforlin Giancarlo, Milano; Zappa Sergio, Brescia. We are indebted to J.D. Baggott for revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Gruppo Italiano per la Valutazione degli Interventi in Terapia Intensiva. GiViTI is the recipient of educational grants from: AstraZeneca Italy, Sanofi-Aventis Italy, and Draeger Italia. A complete list of study participants is presented under Acknowledgements.
Rights and permissions
About this article
Cite this article
Rossi, C., Simini, B., Brazzi, L. et al. Variable costs of ICU patients: a multicenter prospective study. Intensive Care Med 32, 545–552 (2006). https://doi.org/10.1007/s00134-006-0080-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0080-2