Abstract
Objective
To evaluate the prognostic value of hemoglobin levels in critically ill patients with acute renal failure (ARF) requiring dialysis.
Design and setting
A prospective observational cohort study in two adult medical ICUs.
Patients
206 consecutive patients with ARF who required dialysis. Overall 28-day mortality was 48%.
Measurements and results
At ICU admission mean hemoglobin level was 9.1±2.1 g/dl. By ROC curve analysis the threshold value of hemoglobin with the highest sensibility/specificity was 9 g/dl. At baseline 63% of patients had anemia, defined as initial hemoglobin below 9 g/dl. Kaplan-Meier analysis showed that these patients had lower survival rate than those with hemoglobin above 9 g/dl. By multivariable analysis three factors were independently associated with 28-day death: hemoglobin lower than 9 g/dl (adjusted odds ratio 2.4, 95% CI 1.1–5.2), age, and SOFA score. Based on age and SOFA a matched cohort analysis of 67 pairs of ARF patients with or without anemia found similar results regarding the negative impact of anemia on outcome. Finally, a multivariable logistic regression analysis on matched cohort identified hemoglobin level below 9 g/dl (adjusted odds ratio 1.32, 95%CI 1.15–1.46), continuous renal replacement therapy, and vasoactive therapy as independent predictors of 28-day death.
Conclusions
These results suggest that initial hemoglobin level could be helpful in identifying patients with ARF requiring dialysis at high risk of death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The reported incidence of acute renal failure (ARF) varies from 3% to 16% in patients admitted to intensive care units (ICUs) [1, 2]. Despite improvement in hemodynamic tolerance during hemodialysis [3] the mortality rate in ARF remains high, ranging from 20% to more than 50% [4, 5]. Multiple organ system failure and other comorbidities contribute to its high mortality rate; however, ARF independently also increases morbidity and mortality [5].
Anemia is very common in critically ill patients [6, 7, 8], in particular in those with ARF [9]. Hemoglobin concentration frequently falls rapidly in the first few days of ARF, followed by profound and protracted anemia [10, 11]. Multiple causes of anemia may be involved in these severe patients, such as increased red blood cell (RBC) destruction and loss, or decreased RBC production [9]. Furthermore, critically ill patients have impaired erythropoiesis as a consequence of blunted erythropoietin (EPO) production and direct inhibitory effects of inflammatory cytokines. This also induces a related decrease in RBC production [10, 11, 12, 13, 14]. Anemia can pose a threat to the kidneys, which can be magnified by blood loss due to complications of renal replacement therapy (RRT). The segment S3 of the proximal tubule lives in a relative ischemic “penumbra” and is extremely sensitive to changes in oxygen delivery [15]. Thus one can suppose that hypoxia-related anemia would increase the severity of renal tubular cell damage and thus contribute to outcome impairment. However, the prognostic importance of anemia in patients with ARF-induced dialysis is not well defined.
We undertook a prospective multiple-unit observational cohort study to determine the incidence of anemia in patients with severe ARF, defined as the need for RRT, and to assess factors associated with mortality in this specific population of critically ill patients, taking special interest in hemoglobin level at baseline.
Methods
Study cohort
This study was conducted over a 3-year period (January 2001 to December 2003) in two 12-bed adult medical intensive care units in the university hospital of Caen. All consecutive adult patients admitted to the ICUs with ARF requiring RRT or who developed ARF and required dialysis within first week in the ICU were included in the analysis and were followed up by the clinical research team until day 28 or death. A total of 2,421 patients were admitted to the two medical ICUs during the study period, 226 of whom (9.3%) developed ARF requiring dialysis and were prospectively included in the analysis. Twenty patients were excluded because of erythropoietin therapy before initiation of RRT (n=9) or hematological malignancies (n=11). Mean age was 59±15 years, and hemoglobin concentration at ICU admission was 9.1±2.1 g/dl; basic demographic and clinical characteristics at ICU admission of overall population are presented in Table 1. Detailed information was obtained prospectively; data collection began on day 1. Analysis of recorded data respected patient confidentiality and anonymity. Vital status of those patients discharged from ICU before day 28 was ascertained by telephone contact with family members, or registry office if necessary. Overall 28-day mortality was 48%. Because the study did not involve any new intervention, ethics committee approval was not required nor was information consent of patient or next of kin.
Renal replacement therapy directives
Department protocol for RRT indications followed standard recommendations [16, 17]. Continuous renal replacement therapy (CRRT) was the technique of choice for hemodynamically unstable patients suffering from severe sepsis or severe cardiac dysfunction and suspected for hemodialysis-induced hypotension, and CRRT was then switched to intermittent hemodialysis (IHD) as soon as possible. In patients stable enough to tolerate either form of RRT, IHD was most frequently used. In all cases IHD prescription was guided by the goal of achieving a urea reduction ratio of more than 60% [18], with respect to hemodynamic tolerance, as described elsewhere [3]. IHD was performed with dialysis membranes in polysulfone and low molecular weight heparin anticoagulation. Systemic heparin or saline flushes were variably employed for anticoagulation in CRRT, depending on the treating physician’s judgment and department protocol. During the study period the number of days in ICU before RRT, of dialysis session, and of episodes of filter clotting, and the urea reduction ratio were recorded.
Transfusion strategy
During the patient’s ICU stay a restrictive strategy of RBC transfusion was used based on the findings of Hebert and colleagues [19]. Briefly, patients were transfused with leuko-depleted blood when hemoglobin level dropped below 7 g/dl. The goal of transfusion practice was to maintain hemoglobin levels at 7–9 g/dl. A subset of patients with active ischemic cardiac disease as stated in the study cited above required a higher hemoglobin level and received RBC transfusion when hemoglobin fell below 9 g/dl. Daily and pretransfusion hemoglobin levels, the need of RBC transfusion, and the number of transfused units per patients were recorded. Patients with hematological malignancies and those receiving EPO were excluded from the analysis.
Clinical and laboratory data
Demographic and clinical data collected at enrollment included age, sex, origin (home or medical/surgical department), admission categories (medical or surgery), comorbidity conditions, the chronic health status (McCabe and Jackson [20]), and primary diagnosis. Considering initial hemoglobin level, the severity of the illness assessed by the Simplified Acute Physiology Score II (SAPS II) [21], and the number of organ dysfunction at admission assessed by the Sequential Organ Failure Assessment (SOFA) score [22], the worst reading of the first 24 h in the ICU was recorded. In addition, blood samples were collected at admission including serum iron, transferrin saturation, serum ferritin, and C reactive protein concentration to assess the nature of anemia. RBC loss was assessed principally by acute bleeding events (gastrointestinal, intra-abdominal, intrathoracic, intracranial, and others), or extracorporeal blood loss (phlebotomies, surgical procedure, or dialysis circuit clotting) during ICU stay.
Statistical analysis
Values are expressed as mean ±SD, as median and range, or as percentage where appropriate. Normal distribution was assessed by the Kolmogorov-Smirnov test. Qualitative variables were compared using Fisher’s exact test or the χ2 test, and quantitative variables were compared using parametric Student’s t test or nonparametric Mann-Whitney tests as appropriate. We used a receiver operating characteristic (ROC) curve to determine the threshold value of hemoglobin level at admission with the highest sensibility/specificity to predict mortality. Survival curves were prepared according to the Kaplan-Meier method. The dependent variable (28-day mortality) was defined as failure if the patient died before or at day 28. Survival status on day 28 was recorded for all patients, even when they came out of the ICU. We also performed a matched cohort analysis to ensure that our findings were robust. We matched each ARF patients with hemoglobin level below 9 g/dl (anemic) to ARF patients with hemoglobin level above 9 g/dl (nonanemic) for baseline variables found to be predictive of 28-day mortality among these ARF patients. Thus each pair had to fulfill two conditions: anemic patients should have the same age (±3 years) and the same SOFA score (±2 points) at ICU admission as nonanemic patients. We analyzed this subset of ARF patients using McNemar’s χ2 test and the pair-matched Mantel-Haenszel adjusted relative risk (RR). Finally, to adjust for baseline imbalances in covariates between study groups on the overall cohort and on the matched cohort we performed backward deletion logistic regression analyses to identify predictors of 28-day death. We used the p value level of 0.1 to enter and remove variables from the regression. The performance of final model on the test set was assessed using the c-index. All analyses were performed using Epi-info version 6 (Centers for Disease Control, Atlanta, Ga., USA) and SAS 8.2 statistical software (SAS Institute, Cary, N.C., USA). The two-tailed significance level was set at p<0.05.
Results
Patients characteristics
Univariate analysis revealed that nonsurvivors were older and suffered more frequently from comorbid conditions, such as diabetes or coronary artery disease, than those who were still alive at day 28. Primary admission diagnoses differed between groups, with a higher prevalence of infection in nonsurvivors. Nonsurvivors were more severely ill as illustrated by the higher SAPS II and SOFA score at ICU admission, and by the greater need for vasocative therapy and mechanical ventilation. Finally, initial hemoglobin level differed significantly between groups of survivors and nonsurvivors (Table 1).
Characteristics of patients according to hemoglobin level
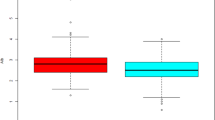
ROC curve analysis (Fig. 1) ascertained that the threshold value of hemoglobin with the highest sensibility/specificity was 9, with 81.7% and 66.7%, respectively. Patients were compared according to hemoglobin level of 9 g/dl or higher vs. a level below 9 g/dl at ICU admission (Table 2). We observed a low hemoglobin level in 129 patients (63%). Groups were similar in baseline characteristics except for age and diabetes. The proportion of preexisting renal insufficiency and of coronary artery disease as comorbidities and the proportion of patients admitted to ICU with cardiological primary diagnosis or infection did not differ between groups. Patients with anemia had greater SOFA score and were more frequently treated with CRRT. However, no difference was observed between groups in the need for mechanical ventilation or vasoactive therapy. Finally, low hemoglobin level was associated with death.
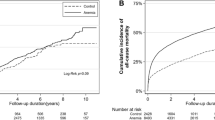
Variables related to anemia and RBC transfusion are reported in Table 3. Iron metabolism showed signs of severe inflammation without significant difference between the two groups of ARF patients segregated according to baseline hemoglobin level: low serum iron, low transferrin saturation, and high serum ferritin, which were in agreement with the high C reactive protein levels. Regarding reasons of RBC transfusion during ICU stay, data were similar between groups for overt bleeding events, extracorporeal blood loss, and cardiac ischemia. Patterns of hemoglobin levels over the study period segregated according to the presence or absence of anemia at baseline showed a convergence of hemoglobin levels over time (Fig. 2). There were 131 patients (65%) with ARF requiring RRT who received RBC during their 28-day following period. Pretransfusion hemoglobin levels were similar between groups. Since violation of the transfusion protocol was only noted in nine patients (4%), i.e., RBC transfusion in patients without active ischemic heart disease with hemoglobin less than 7 g/dl, transfusion practice was consistent with recommendations over the study period. A total of 696 RBC units were transfused over the 28-day period. The proportion of transfused patients and the number of RBC units transfused per transfused patients were higher in patients with anemia at ICU admission. Finally, groups were similar in the number of day(s) between ICU admission and dialysis (Table 2), number of dialysis sessions, number of episodes of clotting (patients with lower hemoglobin, 187 times in 812 days of treatment, 23%; patients with higher hemoglobin, 117 times in 582 days of treatment, 20%) and the urea reduction ratio (Table 3).
Predictors of survival
The cumulative observed survival rate of ARF patients with initial higher hemoglobin was better than this of patients with lower hemoglobin level (57% vs. 32%; Fig. 3). By multivariable analysis (Table 5) only three variables remained independent predictors to death: age, SOFA score, and lower hemoglobin level below at ICU admission.
Matched case-control subgroup analysis
Matching was possible for 134 patients (65% of those in the main analysis). Table 4 compares the 67 pairs of ARF patients at a 1:1 ratio according to hemoglobin level at admission. Anemic patients were well matched to nonanemic patients for gender, primary diagnosis at admission, SAPS II, need for mechanical ventilation, and vasoactive therapy. More nonanemic patients had chronic obstructive pulmonary disease whereas more anemic patients needed CRRT and RBC transfusion. There were 30 and 19 pairs for survival and death, respectively; 15 and 3 pairs were only nonsurvivors in ARF patients with lower hemoglobin level and those with higher hemoglobin level, respectively. The number of conflicting pairs was statistically significant (McNemar’s χ2=6.7; p=0.01), and higher hemoglobin level was associated with a reduced risk of death than in those with lower hemoglobin level (adjusted RR 0.20, 95% CI 0.06–0.69, p=0.01). Multivariable analysis identified anemia, CRRT, and vasocative therapy as factors independently associated with death (Table 5). Following restrictive transfusion strategy there was no association between RBC transfusion and mortality in the covariate adjusted analysis. The discriminatory performance of the composite logistic model demonstrated an excellent c-index for death of 0.793, suggesting that observed and predicted values based on the model did not differ significantly.
Discussion
The negative impact of anemia in the ICU has been recently described in the CRIT study [8] and by Vincent et al. [7] in a large prospective observational study. Both studies observed an association between low hemoglobin level, transfusion, decrease in organ function, and mortality, but the authors failed to comment upon ARF-related anemia. Our cohort study using matched cohorts found an increased risk of death related to low initial hemoglobin level in ARF patients. The exact role of anemia in increasing mortality in ARF dialyzed patients is not currently understood. Adaptive mechanisms to maintain adequate tissue oxygen delivery in heart, brain, lungs, and other organs are triggered by anemia, even at low hemoglobin level [23]. However, the susceptibility of the renal medulla to injury depends on combination of multiple insults. Anemia at baseline may contribute to outpacing the adaptive homeostatic mechanisms controlling medullary oxygen balance and may predispose patients to focal injury at important sites in the kidney.
We observed a high prevalence of low hemoglobin level at ICU admission among ARF critically ill patients requiring RRT. This may be explained by the following: most patients came from the ward or had already signs of severe inflammation, and anemia was at least in part a marker of hemodilution, consequence of volume expansion in hemodynamically unstable patients. However, raising the hemoglobin goals is still a very controversial issue [23]. By contrast with recommendations for the management of anemia in chronic kidney disease [24], guidelines do not propose a specific value or range of values at which to consider transfusion for patients with ARF requiring RRT, citing the lack of data concerning hemoglobin or hematocrit threshold to support recommendations of transfusion in ARF patients. The recent multicenter, randomized controlled clinical trial of transfusion requirement in critical care reported an overall lower hospital mortality in patients assigned to a restrictive strategy [19]. By subgroup analysis the authors showed that restrictive transfusion strategy should be considered with caution in patients with acute myocardial infarction or unstable angina, but failed to consider explicitly ARF patients. Of note, although we found a strong association between anemia and risk of death, RBC transfusion following recent recommendations was not associated with death after adjustment to confounding factors in the logistic regression based on matched cohorts. These data on a specific population of patients with severe ARF are encouraging, but the best strategy to guide clinical practice aimed at increasing hemoglobin level in this subset of ICU patients remains to be determined. Furthermore, since it has recently been demonstrated in an established rat model of ischemic ARF that recombinant EPO can rapidly increase hematocrit and improve mortality during ARF [25], may early infusion of EPO be helpful to increase RBC production in ARF patients?
With a 48% mortality rate, our study also confirmed the poor outcome of ARF patients treated with RRT. Two predictors of death conformed to earlier findings, namely age and SOFA score, were also identified. Changes in the ICU population, as reflected in a greater proportion of elderly patients, have been associated with the lack of improvement in mortality rate of ARF in recent decades [26]. Our study confirms advanced age as a factor associated with worse outcome in critically ARF patients. Furthermore, the high observed mortality rate associated with increased SOFA score, as reported by others in critically ill patients [27, 28], is an illustration of the accuracy of this tool to predict mortality in this subgroup of ICU patients. Interestingly, in multivariable analysis diabetes was not a predictor of death after adjustment to covariates despite an association with anemia and nonsurvivors in univariate anlyses. Until December 2001 all patients in both units were subjected to glycemic control by insulin protocol that aimed to maintain blood glucose below 180 mg/dl; thereafter the level was changed below 150 mg/dl after decreased mortality was reported with intensive insulin therapy in critically ill patients [29]. On matched cohort, vasoactive therapy and CRRT were independently associated with death. Since CRRT was the technique of choice in patients hemodynamically unstable, the association between anemia, CRRT, and poor outcome may be explained at least in part by the negative impact on renal function of lowest hematocrit due to hemodilution, as has recently been reported in patients who underwent cardiac surgery [30].
The main strength of this study was the large number of ARF patients enrolled. All consecutive patients were admitted to two similar medical ICUs during a short 3-year period, and transfusion strategy and management of ARF followed recent recommendations [3, 19]; thus it reflects routinely clinical practice. To our knowledge, this is the first report of a strong association between hemoglobin at baseline and short-term survival in a specific population of critically ill patients with ARF requiring dialysis. However, interpretation of the impact of outcome-related anemia in ICU patients with ARF can be limited by the observational design of the study. Because no intervention was implemented, and no attempt to control was made, this study only identified and described the association between variables of interest. Some confounded factors that may have influenced the outcome were not recorded. Therefore despite multivariable and matched analyses we may have overestimated the effect of anemia at baseline on outcome.
In conclusion, anemia is common in critically ill patients who developed ARF and required dialysis. In this subset of patients hemoglobin concentration below 9 g/dl at ICU admission is an independent and potentially modifiable risk factor to death.
References
Thadhani R, Pascual M, Bonventre JV (1996) Acute renal failure. N Engl J Med 334:1448–1460
Singri N, Ahya SN, Levin ML (2003) Acute renal failure. JAMA 289:747–751
Schortgen F, Soubrier N, Delclaux C, Thuong M, Girou E, Brun-Buisson C, Lemaire F, Brochard L (2000) Hemodynamic tolerance of intermittent hemodialysis in critically ill patients: usefulness of practice guidelines. Am J Respir Crit Care Med 162:197–202
Levy EM, Viscoli CM, Horwitz RI (1996) The effect of acute renal failure on mortality. A cohort analysis. JAMA 275:1489–1494
Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, Le Gall JR, Druml W (2002) Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med 30:2051–2058
Rodriguez RM, Corwin HL, Gettinger A, Corwin MJ, Gubler D, Pearl RG (2001) Nutritional deficiencies and blunted erythropoietin response as causes of the anemia of critical illness. J Crit Care 16:36–41
Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, Meier-Hellmann A, Nollet G, Peres-Bota D (2002) Anemia and blood transfusion in critically ill patients. JAMA 288:1499–1507
Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Abraham E, MacIntyre NR, Shabot MM, Duh MS, Shapiro MJ (2004) The CRIT Study: anemia and blood transfusion in the critically ill-current clinical practice in the United States. Crit Care Med 32:39–52
Hales M, Solez K, Kjellstrand C (1994) The anemia of acute renal failure: association with oliguria and elevated blood urea. Ren Fail 16:125–131
Nielsen OJ, Thaysen JH (1989) Erythropoietin deficiency in acute renal failure. Lancet I:624–625
Lipkin GW, Kendall R, Haggett P, Turney JH, Brownjohn AM (1989) Erythropoietin in acute renal failure. Lancet I:1029
Iperen CE van, Gaillard CA, Kraaijenhagen RJ, Braam BG, Marx JJ, van de Wiel A (2000) Response of erythropoiesis and iron metabolism to recombinant human erythropoietin in intensive care unit patients. Crit Care Med 28:2773–2778
Hobisch-Hagen P, Wiedermann F, Mayr A, Fries D, Jelkmann W, Fuchs D, Hasibeder W, Mutz N, Klingler A, Schobersberger W (2001) Blunted erythropoietic response to anemia in multiply traumatized patients. Crit Care Med 29:743–747
Elliot JM, Virankabutra T, Jones S, Tanudsintum S, Lipkin G, Todd S, Bion J (2003) Erythropoietin mimics the acute phase response in critical illness. Crit Care 7:R35–R40
Brezis M, Rosen S (1995) Hypoxia of the renal medulla-its implications for disease. N Engl J Med 332:647–655
Murray P, Hall J (2000) Renal replacement therapy for acute renal failure. Am J Respir Crit Care Med 162:777–781
DuBose TD Jr, Warnock DG, Mehta RL, Bonventre JV, Hammerman MR, Molitoris BA, Paller MS, Siegel NJ, Scherbenske J, Striker GE (1997) Acute renal failure in the 21st century: recommendations for management and outcomes assessment. Am J Kidney Dis 29:793–799
Owen WF Jr, Lew NL, Liu Y, Lowrie EG, Lazarus JM (1993) The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med 329:1001–1006
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 340:409–417
McCabe WR, Jackson GG (1962) Gram negative bacteremia. I. Etiology and ecology. Arch Intern Med 110:847–855
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Hameed SM, Aird WC, Cohn SM (2003) Oxygen delivery. Crit Care Med 31:S658–S667
Members of the task force on Reuse of Dialyzers (1997) National Kidney Foundation report on dialyzer reuse. Council on Dialysis, National Kidney Foundation. Am J Kidney Dis 30:859–871
Nemoto T, Yokota N, Keane WF, Rabb H (2001) Recombinant erythropoietin rapidly treats anemia in ischemic acute renal failure. Kidney Int 59:246–251
Brivet FG, Kleinknecht DJ, Loirat P, Landais PJ (1996) Acute renal failure in intensive care units-causes, outcome, and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med 24:192–198
Moreno R, Vincent JL, Matos R, Mendonca A, Cantraine F, Thijs L, Takala J, Sprung C, Antonelli M, Bruining H, Willatts S (1999) The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis Related Problems of the ESICM. Intensive Care Med 25:686–696
Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Berghe G van den, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R (2001) Intensive insulin therapy in the critically ill patients. N Engl J Med 345:1359–1367
Swaminathan M, Phillips-Bute BG, Conlon PJ, Smith PK, Newman MF, Stafford-Smith M (2003) The association of lowest hematocrit during cardiopulmonary bypass with acute renal injury after coronary artery bypass surgery. Ann Thorac Surg 76:784–791
Acknowledgements
We thank Drs. William Marie, Anne Lesage, Abdel Ouchikhe, Michel Ramakers, Virginie Verrier, and Sophie Vincent for their contribution in the management of patients.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article refers to the editorial http://dx.doi.org/10.1007/s00134-005-2738-6
Rights and permissions
About this article
Cite this article
du Cheyron, D., Parienti, JJ., Fekih-Hassen, M. et al. Impact of anemia on outcome in critically ill patients with severe acute renal failure. Intensive Care Med 31, 1529–1536 (2005). https://doi.org/10.1007/s00134-005-2739-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2739-5