Abstract
Objective
Calcium desensitization plays an important part in the pathophysiology of septic myocardial depression. We postulated that levosimendan, a new calcium sensitizer, would be beneficial in sepsis-induced cardiac dysfunction.
Design and setting
Prospective, randomized, controlled study in two university hospital intensive care units
Patients and participants
Twenty-eight patients with persisting left ventricular dysfunction related to septic shock after 48 h of conventional treatment including dobutamine (5 µg/kg per minute).
Interventions
After 48 h of conventional treatment patients were randomized to receive a 24-h infusion of either levosimendan (0.2 µg/kg per minute, n=15) or dobutamine (5 µg/kg per minute, n=13).
Measurements and results
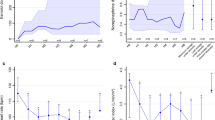
Data from right heart catheterization, echocardiography, gastric tonometry, laser-Doppler flowmetry, and lactate concentrations and creatinine clearance were obtained before and after the 24-h drug infusion. Dobutamine did not change systemic or regional hemodynamic variables. By contrast, at the same mean arterial pressure levosimendan decreased pulmonary artery occlusion pressure and increased cardiac index. Levosimendan decreased left ventricular end-diastolic volume and increased left ventricular ejection fraction. Levosimendan increased gastric mucosal flow, creatinine clearance, and urinary output while it decreased lactate concentrations.
Conclusions
These findings show that levosimendan improves systemic hemodynamics and regional perfusion in patients with septic cardiac dysfunction under conditions where administration of 5 µg/kg dobutamine per minute is no longer efficacious. Accordingly, our results suggest that levosimendan can be an alternative to the strategy of increasing the dose of dobutamine under such conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial depression expressed as biventricular decreased ejection fraction and dilatation typically peaks within the first days of septic shock and then returns to normal values in survivors within 10 days [1, 2]. Among several factors proposed to cause sepsis-induced myocardial depression [3, 4, 5] cytokines play a major role [5] probably by altering intracellular calcium homeostasis in the cardiomyocyte [6, 7]. Administration of lipopolyasaccharide (LPS) has been shown to impair cardiac contractility and the contractile response to β-adrenergic stimulation by nitric oxide–cyclic guanosine monophosphate mediated decrease in myofilament responsiveness to Ca2+. Tavernier et al. [8] showed in an experimental model of sepsis that cardiac mitochondrial and creatine kinase systems remain unaltered, whereas protein phosphorylation decreases myofibrillar Ca2+ sensitivity and may contribute to the depression of cardiac contractility. The reduced myofilament Ca2+ sensitivity is also associated with increased length in single cardiac myocytes and may cause the acute ventricular dilation observed during sepsis [3, 9, 10].
Dobutamine is generally considered as the inotropic treatment of choice for sepsis-related myocardial depression [11]. However, because of sepsis-related myocardial hyporesponsiveness to β-adrenergic stimulation [4] incremental doses of dobutamine may be required to achieve therapeutic goals. As decreased myofilament responsiveness to Ca2+ is a major determinant of septic myocardial depression, calcium sensitization may offer an attractive therapeutic approach to counteract septic myocardial depression, as already shown in animal experiments [12]. Levosimendan is a new calcium sensitizer that has been shown to be even more potent than dobutamine on isolated human atrial trabeculae [13].
The hypothesis that levosimendan administration can be an alternative to the strategy of increasing the dose of dobutamine when the usual dose of 5 µg kg−1 min−1 is no longer efficacious to counteract the septic dysfunction has not as yet been tested. This alternative approach could be particularly attractive since one advantage of levosimendan over catecholamines would be to increase the force of contraction without enhancing the influx of Ca2+ into the cytosol and thus without increasing the risk of arrhythmias related to this ionic alteration [14]. The aim of our prospective, randomized controlled study was to evaluate the effects of levosimendan on systemic and regional hemodynamics in patients with septic cardiac dysfunction occurring and progressing despite administration of 5 µg kg−1 min−1 dobutamine.
Materials and methods
Patients
The study was approved by the local institutional ethics committee, and consent was obtained from the closest relative of each patient. We included only patients with septic shock criteria and initially preserved left ventricular function (left ventricular ejection fraction, LVEF >45%), whose hypotension failed to respond to volume resuscitation (pulmonary artery occlusion pressure, PAOP, ≥12 mmHg). To avoid the enrollment of patients with non-sepsis-related cardiac dysfunction we excluded patients with: echocardiographic LVEF less than 45% before study entry, a history of ischemic or significant valvular heart disease, or confirmed or suspected acute coronary syndrome. We originally enrolled 74 patients, but at the end of the first 48 h 44 patients were excluded because of myocardial ischemia (n=2), significant mitral valve regurgitation (n=4), or still preserved left ventricular function (n=38). The remaining 30 patients, all of whose LVEF was less than 45% at this time, included 23 men and 7 women with a mean age of 62.4±7.4 years and a mean Acute Physiology and Chronic Health Evaluation II score of 23.7±1.2 before study entry.
Protocol
Following volume resuscitation to reach a PAOP of at least 12 mmHg all patients received norepinephrine to maintain mean arterial pressure (MAP) between 70 and 80 mmHg. Following our institutional policy in septic shock we added 5 µg kg−1 min−1 dobutamine to norepinephrine infusion in the aim of improving gut mucosal perfusion [15]. This therapeutic regimen was maintained during the first 48 h of the study. At the end of this period and thus during dobutamine infusion we performed a second echocardiographic examination to measure LVEF again; only patients with a value less than 45% were randomized. The dobutamine infusion was then stopped for a short time necessary to start the syringe-pumps containing either dobutamine or levosimendan. The patients were randomized to receive in a blind fashion for 24 h either an infusion of levosimendan (0.2 µg kg−1 min−1) without an initial bolus loading dose (treated group, n=15) or dobutamine (5 µg kg−1 min−1; control group, n=15). A continuous fluid infusion (hydroxyethyl starch 6%), was given to maintain a PAOP level of at least 12 mmHg during the study while norepinephrine was titrated to maintain MAP between 70 and 80 mmHg. All patients were mechanically ventilated in the controlled mode, with tidal volume of 9 ml/kg, respiratory rate of 12–16 cycles/min, level of positive end-expiratory pressure of 6.3±1.9 cmH2O, and plateau pressure of 20±2 cmH2O, and were sedated with sufentanil and midazolam. All measurements, including cardiac troponin I, arterial lactate concentration, creatinine clearance, urinary output, and the amount of fluid infused, were performed before (baseline) and at the end of the 24-h drug infusion period (Fig. 1). Two of the control patients died before completing the study and were excluded from the analysis; thus 28 patients completed the study (Table 1). Baseline hemodynamic values were similar in the two groups, except for PAOP which was significantly lower in the dobutamine group.
Cardiovascular monitoring included pulmonary (Arrow International, Reading, Pa., USA) and radial artery catheters. Right atrial, mean pulmonary arterial pressure, PAOP and MAP were measured at end-expiration, and cardiac index was obtained by thermodilution (Solar M8000, Marquette Hellige, Milwaukee, Wis., USA). Heart rate was analyzed from continuous electrocardiographic recordings. Stroke index, systemic vascular resistance index), pulmonary vascular resistance index, left ventricular stroke work index, oxygen delivery index, and oxygen consumption index were calculated.
Three-dimensional transesophageal echocardiography was performed with a 5/7 MHz multiplane probe using an ultrasound machine (Philips Sonos 5500, Eindhoven, The Netherlands) equipped with a software that enabled rotational two-dimensional images to be acquired for dynamic three-dimensional reconstruction. Data were analyzed off-line by the three-dimensional system (Tomtec System, Munich, Germany) to calculate end-diastolic (EDVI) and end-systolic (ESVI) volume index. Gastric mucosal perfusion (GMP) was evaluated by a laser-Doppler flowmeter [15] using a gastric probe (Periflux 5000, P 424, Perimed, Stockholm, Sweden). As GMP is measured in arbitrary perfusion units, results are expressed as a proportional change from baseline. We calculated the gradient between gastric mucosal and arterial PCO2 (Pg-aCO2) using an air-tonometer (Tonocap, Datex-Ohmeda, Helsinki, Finland) inserted via a nasogastric route. Enteral feeding and histamine-2 receptor antagonists were discontinued 8 h before and during the period of study.
Statistical analysis
Data are expressed as mean ±SD. Baseline was defined as the end of the first 48-h period. Demographic data were compared between groups using Student’s t test or Mann-Whitney U test. Categorical variables were analyzed by χ2 test when necessary. Between-group differences between baseline and posttreatment values were evaluated by Student’s t test for unpaired data once normality was demonstrated (Shapiro-Wilks test); otherwise the Mann-Whitney U test was used. Within-group comparisons before and after treatment were tested by Student’s t test for paired data once normality was demonstrated (Shapiro-Wilks test); otherwise the Wilcoxon test was used. Differences at a p value less than 0.05 were considered statistically significant (SPSS, version 9, Chicago, Ill., USA).
Results
Levosimendan significantly decreased mean pulmonary arterial pressure, right atrial pressure, PAOP and increased stroke index, cardiac index, oxygen delivery index, oxygen consumption index, and left ventricular stroke work index (overall p ≤0.01) whereas no significant differences were found with dobutamine treatment except that PAOP was increased (p=0.02). Comparison between the two groups after 24 h of treatment showed a difference in PAOP, mean pulmonary arterial pressure, and left ventricular stroke work index (p<0.01; Table 2). Levosimendan decreased EDVI and ESVI and increased LVEF (p<0.01) while these parameters did not change significantly in the dobutamine group (Table 3); at baseline these parameters were similar in the two groups. Compared to both the dobutamine group and to baseline values GMP was increased and ΔPg-aCO2 decreased at the end of levosimendan infusion (p<0.01) whereas no changes were found in the dobutamine group. Compared to dobutamine and to baseline, levosimendan increased both urinary output and creatinine clearance (p≤0.01) and decreased arterial lactate concentrations (p<0.01). Compared to baseline, the amount of fluid infused was higher in the levosimendan group than in the dobutamine group (p<0.01). The groups did not differ in norepinephrine infusion rate (Table 4). During the 24-h comparative period no patient exhibited an acute episode of coronary disease as demonstrated by the absence of significant elevation in cardiac troponin I (Table 4) and of electrocardiographic and/or echocardiographic aspects of myocardial ischemia. Most patients had minor supraventricular tachyarrhythmias, which did not change after treatment. One episode of atrial fibrillation occurred in each group.
Discussion
This study shows that levosimendan improves systemic hemodynamic and regional perfusion in patients with septic cardiac dysfunction under conditions where 5 µg kg−1 min−1 of dobutamine is no longer efficacious. Our results suggest that levosimendan offers an alternative to the strategy of increasing the dose of dobutamine under such conditions. Decreased contractility is a major abnormality of septic myocardial depression, although a decrease in myocardial compliance may also play a role [2, 16]. Dobutamine, a β-agonist agent, is considered the drug of choice in this setting [11]. However, there is considerable evidence for decreased responsiveness of the myocardium to β-adrenergic stimulation during septic shock [4, 17, 18, 19]. This may account for the attenuated hemodynamic effects of 5 µg kg−1 min−1 dobutamine infusion in severe septic shock [4, 15, 20] in comparison with less severe sepsis [21] and nonseptic heart failure [22]. Our findings are in accordance with those reported in severe septic shock patients [4, 15, 20] since neither heart rate, stroke index, nor LVEF increased with dobutamine.
On the other hand, calcium desensitization could play an important role in the pathophysiology of septic myocardial depression [5, 6, 7, 8, 17, 23]. Levosimendan sensitises troponin C to calcium in a calcium concentration-dependent manner. The effects of calcium on cardiac myofilaments during systole are thus enhanced, improving contraction at low energy cost [24]. By showing beneficial cardiac effects of levosimendan our findings are in accordance with those reported in experimental sepsis studies [12, 25]. The increase in LVEF with levosimendan may be due either to an increase in contractility or to a decrease in afterload. Arterial pressure, a major component of left ventricular afterload, did not change with levosimendan. Although we cannot strictly rule out some degree of decrease in left ventricular afterload with this drug, it is likely that improved contractility played a role in the levosimendan-induced increase in LVEF, stroke index, and left ventricular stroke work index. In this regard, previous clinical studies have shown that levosimendan probably improves cardiac function through an inotropic effect [26, 27]. Levosimendan is even reported to be more a potent inotropic agent than dobutamine in isolated human cardiac fibers [13]. Volume resuscitation is most often necessary in septic shock, and in our protocol volume infusion was considered until achieving a PAOP of at least 12 mmHg. Despite randomization the baseline value of PAOP was significantly higher in the levosimendan group than in the dobutamine group. In contrary to dobutamine, levosimendan was decreased PAOP despite a higher baseline PAOP and a higher amount of fluid infused at the end of the 24-h infusion than with dobutamine. We cannot rule out that the increased amount of fluid infused contributed to the beneficial effects levosimendan, especially if patients suffered from some degree of preexisting hypovolemia. This hypothesis is unlikely since EDVI was higher than normal before levosimendan infusion and decreased after levosimendan infusion. Finally, we did not observe any significant decrease in the systemic vascular resistance index or pulmonary vascular resistance index, as previously reported [28]. The global vasodilatory effect of levosimendan is generally attributed to its opening effects on ATP-sensitive potassium channels in vascular smooth muscle [29]. The absence of any marked effect in our patients could be explained by the study design which allowed maintaining MAP by adjusting the norepinephrine dose. Although the pulmonary vascular resistance index did not decrease, the large decrease in PAOP was responsible for the decrease in mean pulmonary arterial pressure and thus probably for the decrease in right ventricular afterload that is often elevated in septic shock [30]. In the setting of right ventricular depression [2, 31] unloading the right ventricle may contribute to further increase right ventricular output. Otherwise, despite simultaneous administration of norepinephrine there was a trend for the calculated global vascular resistance to decrease, albeit not statistically significant (p=0.06). This leaves open the possibility of vasodilatation in some local or regional areas.
In this regard, levosimendan increased GMP flowmetry by increasing systemic blood flow and/or by a direct, local vasodilatory effect. Although our study was not designed to elucidate the precise mechanisms, the large increase in GMP despite a slight increase in cardiac output strengthens the hypothesis of a vasodilatory effect of levosimendan at the level of the gastric microcirculationa. This may be a highly pertinent effect since gut mucosal hypoxia may play a key role in the pathogenesis of multiple organ dysfunction [32]. The addition of dobutamine (5 µg kg−1 min−1) to norepinephrine has previously been shown to increase GMP after a 1-h infusion [15] presumably via blood flow redistribution within the intestinal wall toward the mucosa [33] by β2-adrenergic receptor stimulation [34]. In the present study dobutamine did not increase GMP. This may be related to timing, for in our protocol as well as in another study [35] dobutamine was evaluated after 72 h infusion. It is unlikely that norepinephrine accounted for any gastric perfusion differences between groups, as norepinephrine infusion rates were similar in the two groups.
Beneficial effects of levosimendan were also found at the renal level. The increase (64%) in creatinine clearance with levosimendan could be related to a direct effect of the drug on renal perfusion since MAP was unchanged, and cardiac index increased in a smaller extent. In nonseptic animals levosimendan has been shown to increase blood flow to the renal medulla and to decrease renal medullary and cortical vascular resistance at doses that increase cardiac output and decrease total systemic vascular resistance [36]. By contrast, in endotoxemic animals levosimendan did not prevent the decrease in renal blood flow while protected against the decrease in cardiac output [36]. In contrast to our study, renal perfusion pressure was not maintained constant since MAP decreased markedly in animals receiving levosimendan [25]. In our study the efficacy of levosimendan on renal function was confirmed the increase in urine output.
We found that dobutamine did not exert any effect on creatinine clearance, confirming previous other findings [20] and suggesting that dobutamine does not exert any vasodilatory effect on the renal vasculature. Whether the increase in systemic blood, renal and gastric mucosal flows with levosimendan is associated with improved cellular oxygenation is difficult to determine. However, the increase in oxygen consumption index and the decrease in arterial lactate associated with an increase in oxygen delivery index do suggest a global improvement in tissue oxygenation with the drug.
Our study has some limitations. We measured LVEF, but we did not assess cardiac contractility, a cardiac property that is difficult to approach at the bedside since almost the available indices are more or less dependent on the cardiac loading conditions (preload and/or afterload). Although we cannot verify that levosimendan improved cardiac contractility per se, we can at least conclude that this drug improved the overall left ventricular performance in our patients. We cannot strictly exclude potential hypovolemia having affected our results since we adjusted the volume infusion rate according to PAOP, a rough static marker of preload and of volume status. However, we chose a target PAOP value of 12 mmHg, a value generally considered to reflect a normal preload, except in patients with reduced left ventricular compliance in whom a PAOP of 12 mmHg could be associated with low EDVI. In our study we also measured EDVI and we found high values EDVI rather than low values. Therefore although some degree of hypovolemia cannot be excluded, profound hypovolemia was unlikely to be present in our patients at the time of the study.
Laser-Doppler flowmetry does not allow detailed characterization of microvascular blood flow [15]. However, the reduction in Pg-aCO2 with levosimendan suggests that this drug really improved gastric mucosal perfusion
The design of our study could be questioned and might have lowered its statistical power since we compared levosimendan to a dose of 5 µg kg−1 min−1 dobutamine rather than to a higher dose. Our goal was not to confirm the absolute superiority of levosimendan over dobutamine (whatever the dose) but rather to demonstrate that levosimendan at the usual dose can be efficacious on septic-related cardiac dysfunction under conditions of hyporesponsiveness of the heart to 5 µg kg−1 min−1 dobutamine, a dose usually efficacious in nonseptic heart failure [22]. In the light of our goal the design of our study seems reasonable. Although septic shock is associated with myocardial hyporesponsiveness to catecholamines, one could anticipate that a higher dose of dobutamine (10, 15, or 20 µg kg−1 min−1 or more) would have produced the same beneficial effects as levosimendan on hemodynamics. However, for safety reasons we preferred to avoid this kind of comparison in a clinical research study. Indeed, incremental doses of dobutamine may result in adverse effects (increased myocardial O2 demand, tachyarrhythmia, or decrease in MAP) that we preferred to avoid in those patients already tachycardic. Also for safety concerns we chose not to compare levosimendan to placebo after the 48-h period of dobutamine infusion. Although cardiac dysfunction developed while the patients already received 5 µg kg−1 min−1 dobutamine, it sounds to us unreasonable to replace dobutamine by placebo since it was not excluded that the hemodynamic condition would have further deteriorated with placebo.
Thus we cannot exclude equivalence of dobutamine and levosimendan—and even superiority of dobutamine—if the study had been differently designed. Moreover, it is possible that the absence of significant effect of dobutamine was related not only to a sepsis-induced hyporesponsiveness of the myocardium to β-adrenergic stimulation but also to the classical downregulation of β-adrenergic receptors that usually occurs after administration of β-agonist agent [37]. Although our conclusions must remain cautious owing to the small number of patients enrolled and to the design of the study, our results suggest that levosimendan can exert beneficial effects in terms of systemic and regional hemodynamics in the setting of septic cardiac dysfunction after a 48-h period of 5 µg kg−1 min−1 dobutamine administration. These results suggest that levosimendan offers a safe and efficacious alternative to the strategy of increasing the dose of dobutamine in such a clinical setting.
References
Parker MM, Shetlander J, Bacharach SL, Green MV, Natanson C, Frederick TM, Damske BA, Parrillo JE (1984) Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med 100:483–490
Parker MM, McCarthy KE, Ognibene FP, Parrillo JE (1990) Right ventricular dysfunction and dilatation, similar to left ventricular changes, characterize the cardiac depression of septic shock in humans. Chest 97:126–131
Parillo JE (1993) Pathogenetic mechanisms of septic shock. N Engl J Med 328:1471–1477
Silverman HJ, Peneranda R, Orens JB, Lee NH (1993) Impaired beta-adrenergic receptor stimulation of cyclic adenosine monophosphate in human septic shock: Association with myocardial hyporesponsiveness to catecholamines. Crit Care Med 21:31–39
Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE (1996) Tumor necrosis factor-alpha and interleukin 1-beta are responsible for depression of in vitro myocardial cell contractility induced by serum from humans with septic shock. J Exp Med 183:949–958
Yokoyama T, Vaca L, Rossen RD, Durante W, Hazarika P, Mann DL (1993) Cellular basis for the negative inotropic effects of tumor necrosis factor-alpha in adult mammalian heart. J Clin Invest 92:2303–2312
Goldhaber JI, Kim KH, Natterson PD, Lawrence T, Yang P, Weiss JN (1996) Effects of TNF-alpha on [Ca2+] and contractility in isolated adult rabbit ventricular myocytes. Am J Physiol 271 [Suppl 4]: H 1499–1505 g
Tavernier B, Mebazaa A, Mateo P, Sys S, Ventura-Clapier R, Veksler V (2001) Phosphorilation-dependent alteration in myofilament Ca2+ sensitivity but normal mitochondrial function in septic heart. Am J Respir Crit Care Med 163:362–367
Shah AM, Spurgeon HA, Sollott S, Talo A, Lakatta EG (1994) 8Bromo-cGMP reduces the myofilament response to Ca2+ in intact cardiac myocytes. Circ Res 74:970–978
Zhong J, Hwang T, Adams H, Rubin L (1997) Reduced L-type calcium current in ventricular myocites from endotoxemic guinea pigs. Am J Physiol 273:H2312–H2324
Hollenberg SM, Ahrens TS, Annane D, Astiz ME, Chalfin DB, Dasta JF, Heard SO, Martin C, Napolitano LM, Susla GM, Totaro R, Vincent JL, Zanotti-Cavazzoni S (2004) Practice parameters for hemodynamic support of sepsis in adult patient: 2004 update. Crit Care Med 32:1928–1948
Ming MJ, Hu DY, Chen HS, Liu LM, Nan X, Lu RO (2000) Effects of MCI-154, a calcium sensitizer on cardiac dysfunction in endotoxic shock in rabbits. Shock 13:459–463
Usta C, Puddu PE, Papalia U, De Santis V, Vitale D, Tritapepe L, Mazzesi G, Mirali F, Ozdem SS (2004) Comparison of the inotropic effects of levosimendan, rolipram and dobutamine on human atrial trabeculae. J Cardiovasc Pharmacol 44:622–625
Follath F, Cleland JG, Just H, Papp JG, Scholz H, Peuhkurinen K, Harjola VP, Mitrovic V, Abdalla M, Sandell EP, Lehtonen L; Steering Committee and Investigators of the Levosimendan Infusion versus Dobutamine (LIDO) Study (2002) Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet 360:196–202
Duranteau J, Sitbon P, Teboul JL, Vicaut E, Anguel N, Richard C, Samii K (1999) Effects of epinephrine, norepinephrine or combination of norepinephrine and dobutamine on gastric mucosa in septic shock. Crit Care Med 27:893–900
Poelaert J, Declerck C, Vogelaers D, Colardyn F, Visser CA (1997) Left ventricular systolic and diastolic function in septic shock. Intensive Care Med 23:553–560
Yasuda S, Lew WYW (1997) Lipopolysaccharide depresses cardiac contractility and β-adrenergic contractile response by decreasing myofilament response to Ca2+ in cardiac myocytes. Circulation Res 81:1011–1020
Bernardin G, Kisoka RL, Delporte C, Robberecht P, Vincent JL (2003) Impairment of beta-adrenergic signaling in healthy peripheral blood mononuclear cells exposed to serum from patients with septic shock: involvement of the inhibitory pathway of adenylyl cyclase stimulation. Shock 19:108–112
Matsuda N, Hattori Y, Akaishi Y, Suzuki Y, Kemmotsu O, Gando S (2000) Impairment of cardiac beta-adrenoceptor cellular signaling by decreased expression of G (s alpha) in septic rabbits. Anesthesiology 93:1465–1473
Levy B, Nace L, Bollaert PE, Dousset B, Mallie JP, Larcan A (1999) Comparison of systemic and regional effects of dobutamine and dopexamine in norepinephrine-treated septic shock. Intensive Care Med 25:942–948
Creteur J, De Backer D, Vincent JL (1999) A dobutamine test can disclose hepatosplanchnic hypoperfusion in septic patients. Am J Respir Crit Care Med 160:839–845
Teboul JL, Mercat A, Lenique F, Berton C, Richard C (1998) Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demands in humans: effects of dobutamine. Crit Care Med 26:1007–1010
Hung J, Lew WY (1993) Cellular mechanisms of endotoxin-induced myocardial depression in rabbits. Circ Res 73:125–134
Hasenfuss G, Pieske B, Castell M, Kretschmann B, Maier LS, Just H (1998) Influence of the novel inotropic agents levosimendan on isometric tension and calcium cycling in failing human myocardium. Circulation 98:2141–2147
Oldner A, Konrad D, Weitzberg E, Rudehill A, Rossi P, Wanacek M (2001) Effect of levosimendan a novel inotropic calcium-sensitizing drug, in experimental septic shock. Crit Care Med 29:2185–2193
Nieminen MS, Akkila J, Hasenfuss G, Kleber FX, Lehtonen LA, Mitrovic V, Nyquist O, Remme WJ (2000) Hemodynamic and neurohumoral effects of continuous infusion of levosimendan in patients with congestive heart failure. J Am Coll Cardiol 36:1903–1912
Slawsky MT, Colucci WS, Gottlieb SS, Greenberg BH, Haeusslein E, Hare J, Hutchins S, Leier CV, LeJemtel TH, Loh E, Nicklas J, Ogilby D, Singh BN, Smith W (2000) Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Circulation 102:2222–2227
Ukkonen H, Saraste M, Akkila J, Knuuti J, Karanko M, Iida H, Lehikonen P, Nagren K, Lehtonen L, Voipio-Pulkki LM (2000) Myocardial efficiency during levosimendan infusion in congestive heart failure. Clin Pharmacol Ther 68:522–531
Kaheinen P, Pollesello P, Levijoki J, Haikala H (2001) Levosimendan increases diastolic coronary flow in isolated guinea-pig heart by opening ATP-sensitive potassium channels. J Cardiovasc Pharmacol 37:367–374
Sibbald WJ, Paterson NA, Holliday RL, Anderson RA, Lobb TR, Duff JH (1978) Pulmonary hypertension in sepsis: measurement by the pulmonary artery diastolic-pulmonary wedge pressure gradient and the influence of passive and active factors. Chest 73:583–591
Kimchi A, Ellrodt GA, Berman DS, Riedinger MS, Swan HJ, Murata GH (1984) Right ventricular performance in septic shock: a combined radionuclide and hemodynamic study. J Am Coll Cardiol 4:945–951
Fiddian-Green RG (1993) Associations between intramucosal acidosis in the gut and organ failure. Crit Care Med 21 [Suppl]:S103–S107
Shepherd AP, Riedel GL, Maxwell LC, Kiel JW (1984) Selective vasodilators redistribute intestinal blood flow and depress oxygen uptake. Am J Physiol 247:G377–G384
Maynard ND, Bihari DJ, Dalton RN, Smithies MN, Mason RC (1995) Increasing splanchnic blood flow in the critically ill. Chest 108:1648–1654
Lebuffe G, Levy B, Nevière R, Chagnon JL, Perrigault PF, Duranteau J, Edouard A, Teboul JL, Vallet B (2002) Dobutamine and gastric-to-arterial carbon dioxide gap in severe sepsis without shock. Intensive Care Med 28:265–271
Pagel PS, Hettrick DA, Warltier DC (1996) Influence of levosimendan, pimobendan, and milrinone on the regional distribution of cardiac output in anesthetized dogs. Br J Pharmacol 119:609–615
Scarpace PJ, Abrass IB (1982) Desensitization of adenylate cyclase and down regulation of beta adrenergic receptors after in vivo administration of beta agonist. J Pharmacol Exp Ther 223:327–331
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by an independent research grant from the Department of Anesthesiology and Intensive Care of the University of Rome La Sapienza
Rights and permissions
About this article
Cite this article
Morelli, A., De Castro, S., Teboul, JL. et al. Effects of levosimendan on systemic and regional hemodynamics in septic myocardial depression. Intensive Care Med 31, 638–644 (2005). https://doi.org/10.1007/s00134-005-2619-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2619-z