Abstract
Objective
To investigate whether neuromuscular block can affect bispectral index (BIS) or cerebral hemodynamics under moderate or deep sedation produced by propofol.
Design and setting
Prospective, controlled study in a university hospital affiliated intensive care unit.
Patients
Seventeen surgical patients undergoing elective esophagectomy.
Interventions
After stabilization with either light or deep sedation we investigated whether the BIS, electromyographic activity (EMG), or cerebral and systemic hemodynamic parameters were affected by administration of muscle relaxant.
Measurements and main results
Neuromuscular block reduced the BIS during moderate sedation but not during deep sedation although the EMG at both levels of sedation was significantly reduced. No positive effects of neuromuscular block on cerebral hemodynamics were obtained with monitoring of regional cerebral oxygen saturation and middle cerebral artery blood velocity; however, significant effects on systemic hemodynamic parameters were observed only at moderate propofol sedation. The values of BIS and systemic hemodynamic variables with moderate sedation were also very similar to those with deep sedation and neuromuscular block although these values differed without neuromuscular block.
Conclusions
Neuromuscular block altered the BIS score in moderately sedated patients but not in deeply sedated patients although cerebral hemodynamics was not affected by neuromuscular block during either moderate or deep sedation. Muscular relaxant also enhanced cardiovascular stability with moderate sedation. These results suggest that level of consciousness may be decreased by neuromuscular block during moderate sedation but not affected during deep sedation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several objective methods have recently been evaluated for monitoring the depth of sedation based on processed electroencephalography (EEG) in critically ill patients [1, 2, 3, 4, 5, 6, 7, 8]. One of these is the bispectral index (BIS), an EEG-based objective scale ranging in value from 0 (isoelectric EEG) to 100 (fully awake) that is derived from power and frequency data by the fast Fourier transformation of the raw EEG and an algorithm statistically and empirically based on a large EEG database. It has been shown that this scale is correlated with subjective assessment of the depth of sedation in critically ill patients. However, reliability of the BIS as an objective monitoring method in the intensive care unit (ICU) is still a matter of debate [3, 4, 5, 6, 7, 8]. Several investigators have reported that muscular relaxants decrease the BIS score in fully awake or moderately sedated patients but does not alter it in those who are deeply sedated or anesthetized [9, 10, 11, 12]. Electromyographic activity (EMG) can interfere with EEG state in nonparalyzed persons, and it is therefore thought that alteration in the BIS score by neuromuscular block (NMB) is due to removal of the interference of EMG. It has therefore been concluded that the indirect effects of NMB on level of consciousness are negative [9, 10, 11, 12].
Originally proposed 50 years ago, the “afferent muscle spindle theory” states that signals from muscle stretch receptors stimulate arousal center in the brain [13, 14]. According to this theory, paralysis may reduce signals from muscle stretch receptors that normally contribute to arousal [9, 13]. In this was paralysis may indirectly affect cerebral activity and induce alteration in cerebral hemodynamics, although this may not be sufficient to affect the level of consciousness as assessed by the BIS.
It is possible that removing the interference of EMG by NMB would alter both cerebral hemodynamics and the BIS in moderately sedated patients, who appear to have substantial EMG interference. On the other hand, NMB may hardly affect either the BIS or cerebral hemodynamics in deeply sedated patients, who appears to have little EMG effect. This study was conducted to investigate whether NMB can affect BIS or cerebral hemodynamics at two different levels of sedation produced by propofol: nonresponsive and asleep but responsive to stimuli. We monitored BIS, EMG, regional cerebral oxygen saturation, and cerebral blood velocity as indirect indices for cerebral hemodynamics. Because muscular activity can also affect systemic hemodynamics, we also measured blood pressure, heart rate (HR), and cardiac output, and oxygen delivery and consumption.
Materials and methods
After institutional approval and informed consent 17 surgical ICU patients who underwent elective esophagectomy with thoracotomic approach were enrolled. One patient was excluded because of a blood gas sampling error; therefore 16 patients were evaluated in this study (13 men, 3 women; age 62 ± 9 years; weight 59 ± 5 kg; height 161 ± 8 cm). All patients were managed with propofol- and fentanyl-based anesthesia combined with epidural block during surgery. Patients with symptomatic ischemic heart and cerebral disease, hepatic or renal disease, or neuromuscular disease were excluded. Patients were included in this study only after confirming the lack of an effect of residual muscular relaxant. The lungs of these patients were mechanically ventilated and continuously sedated with propofol and epidural morphine (3 mg/day) and 1% lidocaine (2 ml/h) for 12–24 h after surgery according to the institutional standard protocol for the ICU patients. Propofol was started with continuous infusion at an initial hourly dose of 2 mg/kg, which was modulated in steps of 0.5 mg/kg per hour to maintain a sedation score on the Ramsay et al. [15] scale equal to 4 or 5. This scale has the following values: 1, the patient is anxious and agitated or restless, or both; 2, the patient is cooperative, oriented, and tranquil; 3, the patient responds to commands only; 4, the patient exhibits brisk response to light glabellar tap or loud auditory stimulus; 5, the patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus; and 6, the patient exhibits no response.
Upon arrival in the ICU patients were monitored with standard equipment including continuous electrocardiography, capnograpy, and pulse oximetry. Systemic and pulmonary artery pressure, continuous cardiac output, mixed venous oxygen saturation, and blood temperature were also monitored. In addition, BIS score, regional cerebral oxygen saturation (rSO2), and middle cerebral artery (MCA) blood velocity (VMCA), and effect of neuromuscular agents on muscular activity were continuously monitored. Regarding BIS the electrodes (BIS sensor, Aspect Medical, Newton, Mass., USA) were applied to the forehead as specified by the manufacturer. Before starting the recording the electrode impedance was verified to be below 5 kΩ. The BIS, signal quality index (SQI), and EMG were measured continuously with an Aspect A-2000 monitor (BIS version 3.4; Aspect Medical). The measurements of rSO2 were performed with the INVOS 3100 (Somanetic, Troy, Mich., USA). For the measurements of rSO2, the sensor of INVOS 3100 (somasensor no. 3100 S, Somanetic) was placed on the right or left forehead not to disturb the EEG recording. A 2-MHz pulsed Doppler ultrasound device (Companion TCD System, EME, Überlingen, Germany) was used for transcranial measurements of blood flow velocity of the right MCA. Insonation of the MCA was initiated at a depth of 45 mm. MCA identity was confirmed by increasing insonation depth to visualization of the bidirectional flow pattern typical of the bifurcation of the internal carotid artery into the MCA and anterior cerebral artery. After individual adjustment of Doppler variables such as gain, sample volume, and power of ultrasound the probe was fixed with a headband during the measurement. Using a train-of-four (TOF) guard accelerometer (Organon Teknika, Boxtel, The Netherlands); the effect of neuromuscular agents on muscular activity was monitored by stimulation of the ulnar nerve and acceleromyography at the adductor pollicis muscle. The stimulation electrodes were placed over the ulnar nerve of the wrist and acceleration transducer was placed at the distal part of the thumb. Stimuli in a TOF sequence at 2 Hz were applied and each sequence was repeated every 15 s. The first response in the TOF sequence was recorded and used as the control, to which all subsequent T1 responses were compared.
Experimental protocol
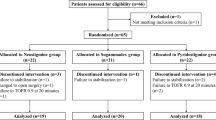
The experimental protocol is presented in Fig. 1. At least 2 h was allowed in the ICU after confirming lack of effect of residual muscular relaxant, which means a train-of-four (TOF) ratio greater than 0.90. The propofol infusion rate was adjusted to maintain a Ramsay score equal to either 4 or 5 or one of 6. To avoid declining effect of general anesthesia or awakening from the operative procedure all patients experienced two different levels of sedation (Ramsay score 4 or 5, or 6) in randomized order. Once the propofol dose was determined for either level of sedation, the infusion rate was not changed until one study period was completed. No noxious stimuli including endotracheal suctioning were given during the study; however, TOF stimuli were given as described above. TOF stimuli used in this study hardly affected any variables in the experimental settings. Because it is possible that problems with pulmonary hygiene due to the lack of endotracheal suctioning themselves are stimulating, endotracheal suctioning was performed before starting the study. After determining the propofol dose muscular relaxant (0.15 mg/kg vecuronium) was administered. The periods before and after and the recovery period from NMB were defined as the control period, neuromuscular period, and recovery period, respectively. The intervals including these three periods were defined as the low-dose period for a Ramsay score of 4 or 5 and the high dose period for a Ramsay score of 6. Fifteen minutes after determining propofol dose the BIS, SQI, EMG, rSO2, and VMCA were recorded for a 15-min period to determine the value of these variables in the absence of muscular relaxant. Simultaneously, other hemodynamic variables including mean systemic and pulmonary artery pressures (MPAP), central venous pressure, and HR were recorded. These variables were recorded each minute, and a 15-min average was calculated for every patients. Pulmonary capillary wedge pressure was recorded every 5 min and averaged. During the same period arterial and mixed venous blood samples for blood-gas analysis were collected, and cardiac output was measured. With these results oxygen delivery and consumption indices and oxygen extraction rate were calculated by standard formulas. After 15 min of the control period control twitch height was calibrated to set the T1 at 100% of control level. Then the muscular relaxant was administered. Ten minutes after T1 decreased to below 5% of control value, measurements for the NMB period were started. Ten minutes after T1 recovered to 90% of control level, measurements for the recovery period were started. A period of at least 2 h was allowed for complete recovery from NMB between completion of the first set of measurements and initiation of the second set of measurements.

Experimental protocol. VB Vecuronium; stabilization stabilization period to maintain each hypnotic status; control control period; NMB neuromuscular period; recovery recovery period
Statistical analysis
The study population size was determined by the following hypothesis. We assumed that NMB would decrease the BIS score by 20 in moderately sedated status, defined as a condition corresponding to BIS 70 ± 25. Based on the formula for normal theory and assuming a type I error probability of 0.05 and a power of 0.80, 17 patients were required. Values between the study periods were compared using analysis of variance with repeated measures followed by paired t test with Bonferroni's correction. The data are expressed as mean ± standard deviation; differences were considered significant at p < 0.05.
Results
The hourly propofol dose required the levels of sedation corresponding to Ramsay score 4 or 5 and 6 were 2.7 ± 0.6 and 4.7 ± 0.5 mg/kg, respectively. SQI was maintained throughout the study above 80%, which means that adequate EEG signals were obtained during the study periods. At the low dose, when sedated status was maintained for a Ramsay score of 4 or 5, NMB significantly decreased both the BIS (79 to 57; Fig. 2) and the EMG (46 to 30 dB; Fig. 3). These variables returned to control values during the recovery period (57 to 78 and 30 to 47 dB, respectively). At the high dose, when sedated status was maintained for a Ramsay score 6, NMB did not significantly change the BIS (55 to 53) although it decreased the EMG (41 to 30 dB) with the low dose, which returned to the control value after recovery from muscular relaxation (30 to 41 dB). NMB did not alter VMCA and rSO2 (Table 1) NMB at either dose. After recovery from muscular relaxation the Ramsay score was not changed compared to the control period with either study dose.

Changes in the bispectral index during the study period (mean ± standard deviation). During the low- and high-dose periods (Ramsay scores of 4 or 5, and 6, respectively) propofol infusion rates did not change once the propofol dose was determined at the start of the study. Control control period; NMB neuromuscular period; recovery recovery period. * p < 0.05 vs. control period, \dag p < 0.05 vs. neuromuscular block period, \ddag p < 0.05 vs. corresponding period with the low dose

Changes in electromyographic activity during the study period (mean ± standard deviation). During the low- and high-dose periods (Ramsay scores of 4 or 5, and 6, respectively) propofol infusion rates did not change once the propofol dose was determined at the start of the study. Control control period; NMB neuromuscular period; recovery recovery period. * p < 0.05 vs. control period, \dag p < 0.05 vs. neuromuscular block period, \ddag p < 0.05 vs. corresponding period with the low dose
Changes in physiological variables are presented in Table 1. With the low dose NMB significantly decreased HR, mean artery and pulmonary pressures, systemic vascular resistance (SVR), oxygen consumption, and oxygen extraction rate and increased mixed venous oxygen saturation. These variables returned to the control values during the recovery period. With the high dose NMB did not affect these variables.
Regarding baseline values at the two doses, values of several parameters, including BIS, EMG, HR, mean artery pressure (MAP), MPAP, and SVR were significantly higher with the low dose than the high dose of propofol. However, these differences were not statistically significant during the NMB period. The differences in BIS and HR declined although they were still observed during the NMB period. During the recovery period differences in BIS, EMG, HR, MAP, MPAP, and SVR values again increased significantly between the low-dose and high-dose periods. Regarding oxygen demand and supply low-dose propofol tended to increase oxygen consumption and extraction rate in the absence of muscular relaxant, although no statistically significant differences in these variables were detected. On the other hand, oxygen demand and supply were very similar in the presence of NMB. At discharge from the ICU no patients reported unpleasantness during the paralyzed status.
Discussion
NMB in this study reduced the BIS in moderately sedated status produced by propofol but did not affect that BIS in deep hypnotic status although EMG at both sedation levels was significantly reduced. No positive effects of NMB on cerebral hemodynamics were obtained by monitoring of rSO2 and VMCA; however, significant effects of NMB on systemic hemodynamic parameters were observed only during moderate propofol sedation. In addition, the BIS and systemic hemodynamic variables at moderate propofol sedation resembled the values at deep sedation in the presence of NMB, while these values were different in the absence of NMB. These results suggest that NMB can enhance cardiovascular stability under moderate sedation but has no effect during deep sedation, which may be mediated by alteration in consciousness due to NMB.
Messner et al. [10] reported that the BIS declined during NMB in fully awake persons. Vivien et al. [11] also observed that the BIS and EMG significantly decreased in sedated ICU patients after administration of a muscle relaxant. On the other hand, Greif et al. [12] found that muscle relaxation affected neither the BIS nor EMG in volunteers anesthetized with propofol. In addition, Ge et al. [9] reported that the BIS was unaltered after the administration of vecuronium in anesthetized surgical patients. These reports are consistent with results from the present study. Our findings thus confirmed these phenomena. As noted above, these phenomena are thought to occur because EMG can interfere with EEG state in nonparalyzed persons which can result in affecting BIS scores.
We also found that muscular relaxation altered systemic hemodynamic variables when moderate sedation was used but had no effect during deep sedation. Enhancement of cardiovascular stability has been considered an epiphenomenon of stably sedated status [16]. It is therefore possible in this study that muscular relaxation affected the level of consciousness under moderate sedation. As mentioned above, paralysis may reduce signals from muscle stretch receptors that normally contribute to arousal, according to the “afferent muscle spindle theory” [9, 13]. Therefore muscular relaxation could indirectly affect the level of consciousness. NMB by the nondepolarizing muscular relaxant pancuronium has been reported to reduce the minimum alveolar concentration by 25% in humans [14] although it is still a matter of debate whether clinical doses of nondepolarizing muscular relaxants can alter this concentration [17]. On the other hand, succinylcholine, which is a depolarizing muscular relaxant and induces a short period of muscular fasciculations, has been reported to produce a transient arousal effect on EEG in cats [13]. These reports are consistent with our present results.
However, cerebral hemodynamics were not altered by muscular relaxation although both BIS and systemic hemodynamic parameters were changed, which suggests that the level of consciousness was changed when the moderate sedation was used. A study with depolarizing muscular relaxants has reported that the administration of succinylcholine was accompanied by increased intracranial pressure (ICP) and cerebral blood flow (CBF) and EEG arousal in anesthetized dogs, and that prevention of fasciculations induced by succinylcholine with nondepolarizing muscular relaxants inhibited increase in ICP in humans [18, 19, 20]. In our experimental settings we investigated the opposite effect (depressant effect) of nondepolarizing muscular relaxants on the cerebral activity. In this situation the reduction in signals from muscle stretch receptors may not be sufficient to induce changes in cerebral hemodynamics compared with the effects of fasciculations on the cerebral activity. Indeed, one study in anesthetized dogs found no changes in cerebral oxygen metabolic rate, CBF, ICP, or EEG by pancuronium [21]. It may be difficult to detect changes in these cerebral parameters in our experimental settings. It is conceivable that other equipment or methods, however, may have detected small changes in cerebral hemodynamics.
Administration of vecuronium to deeply sedated patients did not affect the BIS or other hemodynamic variables, which suggests that muscular relaxation does not affect the level of consciousness. Greif et al. [12] also reported that BIS levels were not altered by mivacurium administration during propofol anesthesia. Their highly sedated status resembled that in our own study. They proposed two possible mechanisms by which muscular relaxation does not alter the BIS: (a) minimum EMG contamination in deeply sedated patients does not interfere BIS analyzing process, and (b) preexisting muscular relaxation in deeply sedated patients in the absence of muscular relaxants does not affect afferent discharges from muscle spindle. In either case muscular relaxation does not appear to affect the BIS or consciousness status in deeply sedated patients.
The question arises as to whether removal of EMG interference by muscular relaxants alters the BIS in moderately sedated patients. Several investigators have proposed this [10, 11]. We believe that removal of EMG interference can affect the BIS to some degree. However, we also believe that the BIS is affected, at least partially, by altered consciousness status due to muscular relaxation. BIS level in moderately sedated patient with NMB resembled that in deeply sedated patients. The difference was clinically insignificant at that time. A clinically significant difference in BIS level would have been detectable if consciousness had not been affected by NMB at all. In addition, our patients with reduced BIS also showed alterations in systemic hemodynamic variables. These cardiovascular responses can be regarded as supporting for the indirect effects of NMB on the level of consciousness [16]. Lanier et al. [22] demonstrated in lightly anesthetized dogs that paralysis diminishes changes not only in EEG activity but also in cerebral and systemic hemodynamic and metabolic status in response to a noxious stimulus. Therefore it is not unreasonable to think that NMB significantly alters the level of consciousness in moderately sedated patients. Other methods for assessing sedation in paralyzed patients would have detected altered consciousness status. Ge et al. [9] reported that NMB reduced the rapidly extracted auditory evoked potentials index during steady state anesthesia, although BIS was not changed. Accordingly, they could not disprove a positive relationship between the indirect effect of muscular relaxation on level of consciousness and this phenomenon. On the contrary, neither BIS score nor hemodynamic variables were affected by NMB in deeply sedated patients although a significant degree of EMG was removed. Here, we must consider that baseline EMG in the absence of NMB in moderately and deeply sedated patients differed significantly, although this difference was small. It appears that the smaller baseline EMG level, the less is the effect of muscular relaxation on BIS [11]. Therefore this small but significant difference in baseline values of EMG (46 vs. 41 dB) may have interferred minimally with the BIS in deeply sedated patients. However, it has been also reported that even small interference of EMG can affect the BIS [10, 11]. Thus it may be difficult to explain the discrepancy between our results and other reports. Differences in experimental design or situations might have affected study results to some extent.
The most significant limitation of this study is that the newest BIS platform, the BIS-XP algorism, was not used to evaluate sedation status. The BIS-XP was designed to improve identification and filtering of electro-oculographic (EOG) and EMG artifact and anomalous EEG patterns such as near-suppression and delta waves during periods of significant non-EEG artifact [6]. Therefore the BIS-XP would have been more suitable in this type of study; however, it has been reported that even the BIS-XP algorism is suboptimal in evaluating the level of consciousness in critically ill patients [6, 8]. Regarding this limitation, it would be pointed out that we provide no data to support our hypothesis. Apart from BIS value changes or cerebral parameter, NMB actually affected hemodynamic status during moderate sedation with propofol. Did propofol accumulation occur only during moderate sedation? However, the Ramsay score did not alter before and after NMB. Thus propofol accumulation did not occur, suggesting that NMB probably affected consciousness status. In addition, we do not think either that vecuronium significantly direct effects on systemic hemodynamics [23, 24]. We should also note that neuraxial aneesthesia may have affected our study results. Neuraxial (epidural) anesthesia can affect the BIS [25]. In our study we presumed that thoracic epidural anesthesia with the institutional protocol contributed to decreasing the BIS to some extent. However, we do not think that thoracic epidural anesthesia affected the study results significantly because the level of sedation according to the Ramsay score was adjusted mainly with propofol infusion rate.
Conclusions
NMB altered BIS score in moderately but not in deeply sedated patients although cerebral hemodynamics were not affected by NMB during either moderate or deep sedation. Muscular relaxant also affected systemic hemodynamic status and enhanced cardiovascular stability in the case of moderate sedation. These results suggest that level of consciousness can be decreased by NMB during moderate sedation but not affected during deep sedation.
References
Veselis RA, Reinsel R, Marino P, Sommer S, Carlon GC (1993) The effects of midazolam on the EEG during sedation of critically ill patients. Anaesthesia 48:463–470
Shearer ES, O'Sullivan EP, Hunter JM (1991) An assessment of the cerebrotrac 2500 for continuous monitoring of cerebral function in the intensive care unit. Anaesthesia 46:750–755
De Deyne C, Struys M, Decruyenaere J, Creupelandt J, Hoste E, Colardyn F (1998) Use of continuous bispectral EEG monitoring to assess depth of sedation in ICU patients. Intensive Care Med 24:1294–1298
Riker RR, Fraser GL, Simmons LE, Wilkins ML (2001) Validating the sedation-agitation scale with the bispectral index and visual analog scale in adult ICU patients after cardiac surgery. Intensive Care Med 27:853–858
Mondello E, Siliotti R, Noto G, Cuzzocrea E, Scollo G, Trimarchi G, Venuti FS (2002) Bispectral index in ICU: correlation with Ramsay score on assessment of sedation level. J Clin Monit Comput 17:271–277
Ely EW, Truman B, Manzi DJ, Sigl JC, Shintani A, Bernard GR (2004) Consciousness monitoring in ventilated patients: bispectral EEG monitors arousal not delirium. Intensive Care Med 30:1537–1543
Nasraway SA SA Jr, Wu EC, Kelleher RM, Yasuda CM, Donnelly AM (2002) How reliable is the bispectral index in critically ill patients? A prospective, comparative, single-blinded observer study. Crit Care Med 30:1483–1487
Tonner PH, Wei C, Bein B, Weiler N, Paris A, Scholz J (2005) Comparison of two bispectral index algorithms in monitoring sedation in postoperative intensive care patients. Crit Care Med 33:580–584
Ge SJ, Zhuang XL, He RH, Wang YT, Zhang X, Huang SW (2003) Neuromuscular block with vecuronium reduces the rapidly extracted auditory evoked potentials index during steady state anesthesia. Can J Anaesth 50:1017–1022
Messner M, Beese U, Romstock J, Dinkel M, Tschaikowsky K (2003) The bispectral index declines during neuromuscular block in fully awake persons. Anesth Analg 97:488–491
Vivien B, Di Maria S, Ouattara A, Langeron O, Coriat P, Riou B (2003) Overestimation of bispectral index in sedated intensive care unit patients revealed by administration of muscle relaxant. Anesthesiology 99:9–17
Greif R, Greenwald S, Schweitzer E, Laciny S, Rajek A, Caldwell JE, Sessler DI (2002) Muscle relaxation does not alter hypnotic level during propofol anesthesia. Anesth Analg 94:604–608
Motokizawa F, Fujimori B (1964) Arousal effect of afferent discharges from muscular spindles upon electroencephalograms in cats. Jpn J Physiol 14:344–353
Forbes AR, Cohen NH, Eger EI 2nd (1979) Pancuronium reduces halothane requirement in man. Anesth Analg 58:497–499
Ramsay MA, Savege TM, Simpson BR, Goodwin R (1974) Controlled sedation with alphaxalone-alphadolone. BMJ 2:656–659
Crippen DW (1990) The role of sedation in the ICU patient with pain and agitation. Crit Care Clin 6:369–392
Fahey MR, Sessler DI, Cannon JE, Brady K, Stoen R, Miller RD (1989) Atracurium, vecuronium, and pancuronium do not alter the minimum alveolar concentration of halothane in humans. Anesthesiology 71:53–56
Lanier WL, Milde JH, Michenfelder JD (1986) Cerebral stimulation following succinylcholine in dogs. Anesthesiology 64:551–559
Minton MD, Grosslight K, Stirt JA, Bedford RF (1986) Increases in intracranial pressure from succinylcholine: prevention by prior nondepolarizing blockade. Anesthesiology 65:165–169
Stirt JA, Grosslight KR, Bedford RF, Vollmer D (1987) “Defasciculation” with metocurine prevents succinylcholine-induced increases in intracranial pressure. Anesthesiology 67:50–53
Lanier WL, Milde JH, Michenfelder JD (1985) The cerebral effects of pancuronium and atracurium in halothane-anesthetized dogs. Anesthesiology 63:589–597
Lanier WL, Iaizzo PA, Milde JH, Sharbrough FW (1994) The cerebral and systemic effects of movement in response to a noxious stimulus in lightly anesthetized dogs. Possible modulation of cerebral function by muscle afferents. Anesthesiology 80:392–401
Booij LH, Edwards RP, Sohn YJ, Miller RD (1980) Cardiovascular and neuromuscular effects of Org NC 45, pancuronium, metocurine, and d-tubocurarine in dogs. Anesth Analg 59:26–30
Saxena PR, Dhasmana KM, Prakash O (1983) A comparison of systemic and regional hemodynamic effects of d-tubocurarine, pancuronium, and vecuronium. Anesthesiology 59:102–108
Ishiyama T, Kashimoto S, Oguchi T, Yamaguchi T, Okuyama K, Kumazawa T (2005) Epidural ropivacaine anesthesia decreases the bispectral index during the awake phase and sevoflurane general anesthesia. Anesth Analg 100:728–732
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inoue, S., Kawaguchi, M., Sasaoka, N. et al. Effects of neuromuscular block on systemic and cerebral hemodynamics and bispectral index during moderate or deep sedation in critically ill patients. Intensive Care Med 32, 391–397 (2006). https://doi.org/10.1007/s00134-005-0031-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-0031-3