Abstract
Objectives
During the acute treatment of diabetic ketoacidosis we (a) determined the temporal incidence of hyperchloraemia, and (b) quantified the influence of hyperchloraemia on interpretation of common blood gas derived acid base parameters, namely base deficit and bicarbonate.
Designand setting
Retrospective chart review in two regional paediatric intensive care units.
Measurements and Results
Stewart's physicochemical theory was used to develop regression equations quantifying the acidifying effect of hyperchloraemia on both base deficit and bicarbonate. These were then applied retrospectively to blood chemistry results from 18 children (median age 12.7 years, weight 43 kg) with diabetic ketoacidosis. Plasma ketonaemia was estimated using the albumin-corrected anion gap. The incidence of hyperchloraemia, as documented by a ratio of plasma chloride to sodium of greater than 0.79, increased from 6% at admission to 94% after 20 h of treatment. Correction for chloride produced a dramatic improvement in the relationship between changes in the anion gap vs. both base deficit (from R 2 = 0.55 to R 2 = 0.95) and bicarbonate (from R 2 = 0.51 to R 2 = 0.96) during treatment. After 20 h of treatment the mean base deficit had decreased from 24.7 mmol/l to 10.0 mmol/l however, the proportion that was due to hyperchloraemia increased from 2% to 98%.
Conclusions
It is now possible using a simple correction factor to quantify the confounding effect of hyperchloraemia on both base deficit and bicarbonate in diabetic ketoacidosis. This bedside tool may be a useful adjunct to guide therapeutic interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic ketoacidosis (DKA) is a common, life-threatening complication of diabetes mellitus in children. The metabolic acidosis at presentation is often profound, and is typically due to elevated blood ketones. Early treatment involves fluid resuscitation with isotonic fluid (such as normal saline) and insulin therapy [1]. The importance of acid-base monitoring during therapy is widely acknowledged, yet many guidelines do not provide detailed instructions on how to interpret and act upon acid-base abnormalities in this setting [1]. A reduction in blood ketones with therapy should be accompanied by a decrease in the anion gap [2]. It is our experience, however, that many clinicians use the base deficit in preference to the anion gap for this purpose. This may be for a variety of reasons, including ease of measurement at the bedside and the fact that the anion gap has been downplayed in DKA because of lack of a tight correlation with calculated bicarbonate [3, 4, 5, 6, 7].
A limitation of the base deficit is that, although an accurate measure of the total metabolic component of an acidosis, it cannot differentiate between co-existent causes, notably ketosis and hyperchloraemia [2]. This may be important in the setting of DKA, as the presence of hyperchloraemia has been documented, although surprisingly its effect on acid-base balance has not been quantified [3]. Thus our first aim was to document the incidence and temporal profile of the development of hyperchloraemia during treatment. Secondly, we have recently validated a formula that allows partitioning of the base deficit into chloride and non-chloride components [8]. We hypothesised that application of this formula to a cohort of children with severe DKA would quantify the influence of hyperchloraemia on the base deficit.
Our final hypothesis concerned the rejection by several authors of the anion gap as a monitoring tool in DKA on the basis of its relationship with bicarbonate. Adrogue et al. [3, 7] and others [5] postulated that a fall in ketoacids (and hence the anion gap) during treatment would be reflected by a compensatory equimolar rise in bicarbonate. However, in practice these investigators found the correlation between change in anion gap and bicarbonate to be poor, leading them to conclude that the anion gap was unreliable [3, 4, 5, 7, 9, 10]. A major flaw with this conclusion involved failure to appreciate the influence of hyperchloraemia on bicarbonate, despite the authors documenting its presence [11, 12]. We have thus applied a similar methodology to bicarbonate, partitioning the effect of chloride and non-chloride elements on its final value. We hypothesised that an equimolar relationship between bicarbonate and anion gap would be revealed after partitioning. If a substantial chloride effect occurs on base deficit and bicarbonate in DKA, this may affect the interpretation of these traditional acid-base parameters, and may have implications for treatment.
Methods
We reviewed the case records of all patients admitted with diabetic ketoacidosis to two regional paediatric intensive care units (Guy's Hospital, London and Alder Hey Hospital, Liverpool) from January 2001 to December 2003. Diagnosis of diabetic ketoacidosis included hyperglycaemia (glucose greater than 11 mmol/L), venous pH less than 7.30 and bicarbonate less than 15 mmol/L [2]. Venous blood gases and electrolytes were recorded at 4-h intervals commencing from initiation of therapy at the referring hospital. The study concluded after 20 h, as this represented the time of the first patient discharge from the intensive care unit. Patients with incomplete biochemical and acid-base profiles during the study were excluded, as these measurements are necessary for the Stewart equations.
Of the 28 patient episodes identified (26 patients) 10 were excluded due to plasma chloride not being recorded on presentation to the referring hospital. The median (interquartile range) age and weight of the remaining 18 patients was 12.7 years (10.1–14.9) and 43 kg (32–55), respectively. Our local ethics committee waives the need for informed consent for retrospective chart reviews, when patients are non-identifiable.
Blood chemistry profiles
Venous blood gases and chemistry were measured using the Instrumentation laboratory 1640 blood gas analyser (Lexington Mass., USA) and Synchron LX20 (Beckman Coulter, Buckinghamshire, UK) at Guy's Hospital, and the Rapidlab 845 gas analyser (Bayer, Germany) and Integra 700 (Roche, Switzerland) at Alder Hey Hospital. Sodium was measured using an ion selective lithium sodium aluminium silicate glass electrode. Sodium ions undergo an exchange process with the sodium ions in the electrode causing a change in potential which is referenced to the glass electrode. Potassium was measured using an ion selective electrode with a valinomycin polyvinylchloride membrane. Potassium ions complex with the valinomycin causing a change in potential which is detected by the reference electrode. Chloride was measured using a solid-state silver chloride membrane electrode. Chloride ions in the sample react to cause a change in potential which is detected by the reference electrode.These electrodes operate with indirect ion selective methodology (Beckman Instruments Manual 1997).
Serum bicarbonate was expressed as total carbon dioxide content (TCO2) using the formula: actual bicarbonate + pCO2 (mmHg) × 0.03. The standard base deficit was calculated in all samples according to the algorithm of the 1640 gas analyser. Plasma albumin was measured by bromocresol green dye binding, and whole blood lactate by the enzymatic method (YSI 2300 STAT plus analyser, Yellow Springs Instruments, Ohio, USA). The precision values for the above analysers were as follows: pH 0.009–0.005 (at pH of 7.15 and 7.66, respectively), PCO2 2.74–2.78%, ion specific electrodes all less than 2%, albumin 6.2% and 3.0% (at albumin concentrations of 13 and 37 g/L, respectively), lactate 2.0%. The anion gap was corrected for albumin as follows: anion gap = (Na + K) − (Cl + TCO2) + 0.25 × [40 − albumin (g/L)] [13]. The reference range for the anion gap in our laboratory is 11 to 17 mmol/L. Hyperchloraemia was defined as a ratio of chloride to sodium (Cl:Na) > 0.79 [14]. The strong ion gap was calculated as {[Na+] + [K+] + [Mg2+] + [Ca2+] − [Cl−] − [lactate−]} − {[1000 × 2.46 ×10−11 × (pCO2/10−ph) + ([albumin g/L] × (0.123 × pH − 0.631) + [phosphate] × (0.309 × pH − 0.469)}.
Quantifying the contribution of chloride to bicarbonate and base deficit
A detailed description of the Stewart methodology is beyond the scope of this contribution, and is available elsewhere [11, 12, 13, 15] Briefly, this concept applies the laws of mass action, mass conservation and preservation of electroneutrality (see “Appendix”) to all components of human plasma that influence the hydrogen ion concentration. The chief source of hydrogen ions is via water dissociation, which is in turn affected by three independent variables: pCO2, total amount of weak acids and the strong ion difference. Strong ions are defined as those from molecules which are completely dissociated at physiological pH, the predominant components being sodium and chloride. When the strong ion difference decreases (for example, a rise in chloride relative to sodium), water dissociation increases and pH falls. This effect can only be quantified by solving simultaneously all of the required Stewart equations (including three equilibrium reactions for carbonic acid, two equilibrium reactions for phosphate, one for albumin, the strong ion difference and the preservation of electroneutrality). Customised software (AcidBasics II version 1.3, University of South Carolina, USA) [15] utilising the standard Stewart and Figge equations was used to quantify the influence of chloride on pH, base deficit and bicarbonate. This software has been validated both in vitro and in vivo [13, 15].
We used AcidBasics II to theoretically vary the plasma chloride relative to sodium over a wide range (chloride 70 to 130 mmol/L) whilst keeping all other variables that contribute to pH constant (pCO2 40 mmHg, albumin 40 g/L, phosphate 1.3 mmol/L, calcium 2.3 mmol/L, and unmeasured anions 2 mmol/L; “Appendix”). Thus the resultant changes in pH, base deficit and bicarbonate are due purely to the differences between chloride and sodium. We were thus able to construct regression equations to predict how much base deficit and bicarbonate varied with changes in chloride. The regression equations were as follows: chloride-induced base deficit = 0.99 × (Na-Cl) − 31.9, R 2 = 0.99, chloride-induced bicarbonate = 0.92 × (Na-Cl) − 5.8, R 2 = 0.99.
To illustrate how the regression equations are used to correct for chloride, we consider a hypothetical patient with the following values: Na 140 mmol/L Cl 116 mmol/L, pH 7.25, pCO2 16 mmHg, actual bicarbonate 7 mmol/L, base deficit 18 mEql/L. The base deficit was partitioned by application of the first regression equation. This demonstrates that 8 mEql/L ([0.99 × (140 − 116) − 31.9] of the total base deficit is due to the chloride effect. Derivation of the chloride-corrected bicarbonate involves a two-step process. First, from the second regression equation, the predicted bicarbonate accounted for solely by this chloride level is 16 mmol/L, representing a fall of 11 mmol/L from the normal venous value of 27 mmol/L (Fig. 1, left bar). Second, we then add the fall in bicarbonate due to chloride to the patient's actual bicarbonate, i.e. 11 mmol/L plus 7 mmol/L = 18 mmol/L (Fig. 1, right bar).
Two-step procedure for calculating the chloride-corrected bicarbonate concentration. The regression equation [0.92 × (Na-Cl) − 5.8] is used to calculate the predicted bicarbonate value (16 mmol/L) at the measured levels of both sodium and chloride. The difference between this value and a normal venous value of 27 mmol/L (left) is then added to the actual bicarbonate to derive the chloride-corrected bicarbonate (18 mmol/L, right). Note that in cases of relative hypochloraemia, the regression equation will produce a predicted bicarbonate value above 27 mmol/L. If so, the difference is then subtracted from the measured bicarbonate concentration
Patient treatment
All patients were resuscitated initially with 0.9% saline, receiving a median (interquartile) fluid volume of 39 ml/kg (32–48) over the first 4 h. Either 0.9% or 0.45% saline was used thereafter, and dextrose added when blood glucose approximated 15 mmol/L. The cumulative fluid input at 20 h was 91 ml/kg (78–106). The median (interquartile) insulin dose per hour was initially 0.1 U/kg (0.09–0.1), decreasing to 0.05 U/kg (0.04–0.05) by 20 h.
Results
The acid-base and electrolyte changes over the study period are shown in Table 1. Metabolic acidosis persisted at 20 h (mean pH 7.31, base deficit 10.0 mmol/L), although normalisation of the anion gap (from 25 to 16 mmol/L) suggested resolution of ketosis. A mean bias of 6.3 (95% limits of agreement −0.5 to 13.3) was observed when the albumin corrected anion gap was compared with the strong ion gap. There was a strong correlation between the strong ion gap and albumin corrected anion gap (y = 0.98x + 9.8, R 2 0.97). The mean blood lactate concentration was below 2 mmol/L for all time points. The incidence of hyperchloraemia increased progressively from 6% at start of treatment to 94% at 20 h.
We partitioned the base deficit into its chloride and non-chloride components (Fig. 2). It can be seen that chloride accounts for an increasing proportion of the base deficit with time, escalating from 2% at initiation of therapy to 98% by 20 h. Conversely, the resolution of the non-chloride (presumably ketotic) component of the base deficit was mirrored by a reduction in the anion gap. The strength of this association is shown in Fig. 3. Not surprisingly the association between total base deficit and anion gap improved markedly after correction of the former for the chloride effect (R 2 = 0.55 − 0.95, Fig. 3b).
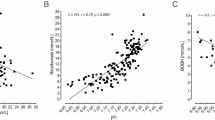
Our secondary hypothesis concerned the relationship between the anion gap and bicarbonate. Figure 4a shows a similar relationship to that demonstrated by Adrogue et al. [3, 7]. Of note the anion gap decreases at a faster rate than bicarbonate increases (slope −0.45). However after adjustment for the chloride effect on bicarbonate, an equimolar relationship is revealed (slope 0.99, Fig. 4b).
Regression plots for albumin-corrected anion gap versus plasma bicarbonate before (a) and after correction for chloride (b). Data are pooled from all patients at all time points. Closed symbols represent the relationship after correction for chloride. Plasma bicarbonate is represented by the total carbon dioxide content (TCO2)
Discussion
There are three major findings from this study. First, we have documented a high incidence of hyperchloraemia during the treatment of DKA that increases with time. Although not present at admission, hyperchloraemia develops rapidly, increasing to 50% by 4 h, thereafter showing a slower but consistent rise to an incidence of 94% by 20 h. Interestingly the most rapid rise in hyperchloraemia coincided with the period of greatest fluid (and hence chloride) administration; approximately 40% of total fluid was given within the first 4 h.
Secondly, resolution of ketoacidosis is masked by the acidifying effect of chloride when the total base deficit is used (Fig. 2). It is our experience that clinicians involved in the treatment of DKA often call the tertiary referral centre for advice when the base deficit is slow to resolve. However, we have shown that hyperchloraemia is the dominant metabolic component of the acidosis after twelve h of treatment, and accounts for 98% of the base deficit by 20 h. The causes of this may be due to chloride-rich fluids used during treatment, combined with preferential renal excretion of ketones over chloride [3, 7]. The clinical significance of hyperchloraemic acidosis in this setting is uncertain; however there is evidence suggesting that hyperchloraemia may influence the resolution of ketoacidosis [16]. We are not suggesting a change in the established fluid regimes for diabetic ketoacidosis as a consequence of this study, but rather recognition that resolution of ketosis may be masked by the development of hyperchloraemia.
Third, we have shown that, during the treatment of DKA, an equimolar relationship is revealed between changes in the anion gap and bicarbonate only after correction of the latter for chloride. In other words, the corrected bicarbonate will rise as the anion gap falls in a one-for-one manner. Prior to this many authors have attempted to explain the apparent lack of an equimolar relationship by postulating a difference between the volume of distribution of ketoacids and bicarbonate, or loss of “potential” bicarbonate with ketonuria [3, 5, 6, 7]. However, all have overlooked the important contribution of chloride, despite recognising hyperchloraemia as a common entity in DKA. This is not surprising, as the Henderson-Hasselbalch methodology does not ascribe a direct role for chloride in acid-base balance, and the Stewart method was not widely appreciated until recently [12, 13, 15]. The Henderson-Hasselbalch equation dictates that bicarbonate changes independently of CO2, a relationship that is not seen in practice because a change in CO2 directly influences carbonic acid content and hence bicarbonate as it dissociates at physiological pH. Interestingly, the concept of correcting bicarbonate to improve its value as a marker of metabolic acidosis is not new. The “standard bicarbonate”, which corrects bicarbonate to a normal pCO2 of 40 mmHg, has been in use for almost 50 years [17]. The Stewart technique used in this study follows a similar principle; correcting the bicarbonate for changes in chloride relative to sodium. This has provided a simple explanation for the acid-base phenomena seen in DKA, in contrast to the previous complex theories that have lacked in vivo verification [3, 5, 6, 7].
These findings have several clinical implications. A persisting base deficit or low bicarbonate may be interpreted erroneously as being due to ongoing ketosis or hypovolaemia, prompting a change in insulin dose and/or increased fluid administration. Both therapies may be deleterious: high-dose insulin may be associated with greater mortality [17, 18], while several studies have suggested that excess fluid may increase the risk of cerebral oedema [18, 19] as well as propagating an acidosis [20].
The limitations of traditional methods for acid-base interpretation in DKA are highlighted by a recent trans-Atlantic consensus statement [1]. The statement suggests performing “blood-gas analysis” 2-hly yet provides no advice on interpretation of the values obtained, a potential role for bicarbonate therapy is discussed in relation to pH only, and the existence of hyperchloraemic acidosis is acknowledged without guidance on how to diagnose this entity. The document does, however, suggest a role for the anion gap as a means to track resolution of ketosis [1]. However, two limitations of the anion gap in this setting are (a) an inability to differentiate a mixed metabolic acidosis (hyperchloraemic and ketotic), and (b) the degree of hyperchloraemic acidosis is not quantifiable. Partitioning the base deficit overcomes this.
We suggest that the utilisation of a simplified version of our regression equation to partition the chloride component of the base deficit, namely (plasma sodium–plasma chloride −32) would allow clinicians a rapid bedside tool to track the resolution of ketoacidosis. This mandates the measurement of plasma chloride, which should be available routinely in most district general hospitals. To confirm this we telephoned 43 laboratories from district general hospitals in our region of which 91% had the facility to measure plasma chloride. However, in our study chloride was not requested at presentation for 10 of 28 (36%) patients suggesting a failure to appreciate its importance by the attending staff. In addition, plasma chloride is not currently available from the majority of point-of-care devices.
A limitation of this study involves the assumption that ketoacids comprise the principal component of an elevated anion gap. Although we did not measure blood ketones, Adrogue et al. [3] has shown that the degree of ketonaemia follows the anion gap closely, and resolves over a time period similar to our study (serum β-hydroxybutyrate 22.1–2.2 mmol/l) [3]. It is unlikely that other sources of tissue acid were present in significant quantities in our study, as hyperlactataemia was not demonstrated. We demonstrated a tight correlation between anion gap (albumin corrected) and strong ion gap (R 2 = 0.97) with almost complete resolution of the SIG by 20 h (24.9 to 7.1 mEq/L), supporting the observation that the metabolic acidosis at 20 h was almost exclusively due to hyperchloraemia.
In conclusion, we have demonstrated that hyperchloraemia is a common entity in DKA; furthermore the incidence increases with time during treatment. The acidifying effect of hyperchloraemia reduces the accuracy of the base deficit in quantifying ketosis. A simple modification of the base deficit requiring simultaneous measurement of plasma chloride and sodium may overcome this limitation.
References
Dunger DB, Sperling MA, Acerini CL, Bohn DJ et al. (2004) ESPE/LWPES consensus statement on diabetic ketoacidosis in children and adolescents. Arch Dis Child 89:188–194
Emmett M, Narins RG (1977) Clinical use of the anion gap. Medicine (Baltimore) 56:38–54
Adrogue HJ, Wilson H, Boyd AE, III, Suki WN, Eknoyan G (1982) Plasma acid-base patterns in diabetic ketoacidosis. N Engl J Med 307:1603–1610
Oh MS, Banerji MA, Carroll HJ (1981) The mechanism of hyperchloraemic acidosis during the recovery phase of diabetic ketoacidosis. Diabetes 30:310–313
Halperin ML, Bear RA, Hannaford MC, Goldstein MB (1981) Selected aspects of the pathophysiology of metabolic acidosis in diabetes mellitus. Diabetes 30:781–787
Paulson WD (1986) Anion gap-bicarbonate relation in diabetic ketoacidosis. Am J Med 81:995–1000
Adrogue HJ, Eknoyan G, Suki WK (1984) Diabetic ketoacidosis: role of the kidney in the acid-base homeostasis re-evaluated. Kidney Int 25:591–598
O'Dell E, Tibby SM, Durward A, et al. (2005) Validation of a method to partition the base deficit in meningococcal sepsis: a retrospective study. Crit Care 9:R464–470
Hammeke M, Bear R, Lee R, Goldstein M, Halperin M (1978) Hyperchloraemic metabolic acidosis in diabetes mellitus: a case report and discussion of pathophysiologic mechanisms. Diabetes 27:16–20
Oh MS, Carroll HJ, Goldstein DA, Fein IA (1978) Hyperchloraemic acidosis during the recovery phase of diabetic ketosis. Ann.Intern.Med 89:925–927
Stewart PA (1983) Modern quantitative acid-base chemistry. Can J Physiol Pharmacol 61:1444–1461
Gilfix BM, Bique M, Magder S (1993) A physical chemical approach to the analysis of acid-base balance in the clinical setting. J Crit Care 8:187–197
Figge J, Jabor A, Kazda A, Fencl V (1998) Anion gap and hypoalbuminemia. Crit Care Med 26:1807–1810
Durward A, Skellet S, Mayer A, Taylor D, et al. (2001) The value of the Cl:Na ratio in differentiating the aetiology of metabolic acidosis. Intensive Care Med 27:828–835
Wilkes P (1998) Hypoproteinaemia, strong ion difference and acid-base status in critically ill patients. J Appl Physiol 84:1740–1748
Hood VL, Tannen RL (1998) Protection of acid-base balance by pH regulation of acid production. N Engl J Med 339:819–826
Astrup P (1956) A simple electrometric technique for the determination of carbon dioxide tension in blood and plasma, total content of carbon dioxide in plasma and bicarbonate content in ‘separated’ plasma at a fixed carbon dioxide tension. Scand Clin Lab Invest 8:33
Wagner A, Risse A, Brill HL, et al. (1999) Therapy of severe diabetic ketoacidosis. Zero-mortality under very-low-dose insulin application. Diabetes Care 22:674–677
Mahoney CP, Vlcek BW, DelAguila M (1999) Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol 21:721–727
Roberts MD, Slover RH, Chase HP (2001) Diabetic ketoacidosis with intracerebral complications. Paediatric Diabetes 2:109–114
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Law of mass action
When a weak acid dissociates incompletely in an aqueous solution, the relationship between the dissociated and undissociated components is constant. The Henderson equation is a well-known modification of this law, namely k = [H+] [HCO3 −]/[H2CO3], where k is defined as the hydrogen ion concentration at which half of the carbonic acid is dissociated. The Stewart approach also applies the law of mass action to carbonic acid but includes other major weak acids found in human plasma (albumin, phosphate), as well as incorporating the dissociation equilibrium for water: K w = [H+] [OH−]/[H2O].
Mass conservation
In an aqueous solution the amount of each component substance remains constant unless (a) a substance is added or removed or (b) the substance is generated or destroyed.
Preservation of electroneutrality
In an aqueous solution, the sum of all positively charged ion concentrations always equals the sum of all negatively charged ion concentrations.
AcidBasics II software uses the Stewart equations to calculate pH from its three independent variables, namely pCO2, strong ion difference ([Na+] + [K+] + [Mg2+] + [Ca2+] − [Cl−] − [lactate−]) and total weak acid (phosphate and albumin charge) at a temperature of 37°C. If pH is known and all variables other than sodium and chloride are kept constant the magnitude of pH change as chloride is varied relative to sodium can be calculated. Since bicarbonate is dependent on pH, its theoretical charge (mEq/L) can be accurately calculated using across varying degrees of hypo/hyperchloraemia (chloride 70–130 mmol/L) by keeping all other variables in Stewart's equation constant. A linear regression equation can be plotted between (Na-Cl) and calculated bicarbonate to explain the degree to which bicarbonate is directly influenced by hyperchloraemia. For example sodium of 140 mEq/L and chloride 120 mEq/L (difference 20 mEq/L) will result in a bicarbonate concentration of 0.93 × 20 mEq/L − 5.9 = 12.7 mEq/L using this regression equation. A similar approach can be used to calculate the influence of hyperchloraemia on the base deficit. For example a difference of 20 mEq/L between Na and Cl results in a base deficit of −1.2 × 20 mEq/L + 42.5 = −18.5 mEq/L. Stewart's methodology is necessary since the traditional Henderson-Hasselbalch model assumes bicarbonate is an independent variable and is not influenced by chloride, hence it offers no method for the quantification of hyperchloraemic acidosis.
Rights and permissions
About this article
Cite this article
Taylor, D., Durward, A., Tibby, S.M. et al. The influence of hyperchloraemia on acid base interpretation in diabetic ketoacidosis. Intensive Care Med 32, 295–301 (2006). https://doi.org/10.1007/s00134-005-0009-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-0009-1