Abstract
Objective
To evaluate various treatment strategies in critically ill patients with ischaemic acute renal failure, there is a need for reliable bedside measurements of total renal blood flow (RBF), glomerular filtration rate (GFR) and renal oxygen consumption without the need for urine collection.
Design
The continuous renal vein thermodilution method and the infusion clearance techniques were validated against the gold standard technique, the urinary clearance of paraaminohippurate (PAH) and chromium ethylenediaminetetraacetic acid, respectively.
Setting
University hospital cardiothoracic ICU.
Patients
Seventeen uncomplicated mechanically ventilated post-cardiac surgical patients.
Interventions
None.
Measurements and results
Renal blood flow, GFR and the renal filtration fraction (FF) were measured for two consecutive 30-min periods by urinary clearance and compared with simultaneous measurements made by the thermodilution and infusion clearance techniques. Urinary clearance for PAH was corrected for by renal extraction of PAH. The within-group error, repeatability coefficient and the coefficient of variation were highest for the thermodilution technique and lowest for the infusion clearance technique with regard to RBF, GFR and FF. The infusion clearance technique had a higher agreement with the urinary clearance method than the thermodilution method. For estimations of RBF and GFR, the between-group errors were 33% and 43% comparing infusion clearance with urinary clearance and 65% and 67% comparing thermodilution with urinary clearance.
Conclusions
The infusion clearance method had the highest reproducibility and the highest agreement with the urinary clearance reference method. The renal vein thermodilution technique is less reliable in the ICU setting due to poor repeatability and poor agreement with the reference method.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perioperative repeated episodes of renal hypoperfusion might play a central role in the pathophysiology of acute renal failure (ARF) [1]. The renal medullary concentrating mechanism, requiring large amounts of oxygen, renders the renal medulla hypoxic already under normal conditions [2]. The renal medulla, particularly the outer portion, is therefore particularly sensitive to acute renal ischaemia. A logical approach in the management of clinical ischaemic ARF would therefore be to improve the renal oxygen supply/demand relationship by augmenting renal blood flow and/or to reduce renal oxygen consumption. In order to evaluate various interventions to treat ischaemic ARF in the critically ill patient, there is a need for reliable bedside measurements of renal blood flow (RBF), glomerular filtration rate (GFR) and oxygen consumption.
The use of the standard method for estimating renal blood flow, urinary clearance of paraaminohippurate (PAH), has several limitations in patients with ischaemic ARF. First, it assumes an almost complete extraction (>90%) of PAH from the renal circulation with subsequent delivery to the urine [3]; renal extraction of PAH might be considerably lower in ischaemic ARF [4, 5, 6]. Second, errors may be introduced by inaccurate collection of urine and by dead space of the urine collection system [7, 8]. When urine flow is rapidly increased or decreased, the renal clearance of PAH will be unduly high or low, respectively, as a consequence of the dead space error [7, 8].
To circumvent the problems with the standard urinary clearance technique, it has been suggested that RBF can be estimated in humans by the local thermodilution technique, using an indwelling renal vein catheter without the need for urine collections [4, 9, 10, 11]. Thermodilution estimation of RBF was shown to correlate to standard urinary PAH-clearance determined RBF [4, 9, 10, 11]. However, in none of these studies were the agreement between the two methods tested as suggested by Bland and Altman [12].
Another approach for the estimation of RBF without urine collection is to use the so-called constant-infusion technique, in which renal clearance is calculated from the arterial serum level of PAH and the infusion rate of PAH [7, 13, 14, 15, 16]. Requirements for this method are that the test substance (e.g. PAH) is rapidly equilibrated after the start of infusion, not metabolised and only excreted by the kidney. Furthermore, there should be equilibrium between the rate of excretion and rate of infusion of the test substance and its volume of distribution should be constant during the infusion period, as indicated by stable serum concentrations of the test substance. To our knowledge, the validity of the constant-infusion technique has not been assessed in the intensive care setting.
The aim of the present study was to test the validity of these two independent methods for bedside estimation of RBF, GFR and renal filtration fraction without urine collection in postoperative, sedated and mechanically ventilated cardiac surgical patients. The agreement between these two methods and the gold standard technique, the urinary clearance and renal extraction of PAH and chromium ethylenediaminetetraacetic acid (51Cr-EDTA), respectively, were assessed.
Methods
The Human Ethics Committee of the University of Göteborg approved the study protocol. Twenty patients with a preoperative serum creatinine of 150 µmol/l or less, undergoing elective cardiac surgery with cardiopulmonary bypass, were recruited after informed written consent. The patients were excluded from the study if they required inotropic support with or without intra-aortic balloon pump early after surgery. In the intensive care unit (ICU) the patients were sedated with propofol and mechanically ventilated. A pulmonary artery thermodilution catheter (Baxter Healthcare, Irvine, CA.) was inserted through a subclavian vein.
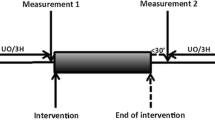
Measurements of renal blood flow by continuous retrograde thermodilution
A ball-ended 8 Fr two-thermistor retrograde venous thermodilution catheter (Webster Laboratories, Baldwin Park, CA,), originally designed for coronary sinus studies [17], was introduced into the left renal vein via the right jugular vein, under fluoroscopic guidance. The catheter was placed in the central portion of the renal vein and its position was verified by venography [18]. For measurement of RBF, isotonic saline (indicator), maintained at room temperature, was infused for 15–30 s at a constant rate of 48 ml/min. A two-channel Wheatstone bridge was used to measure changes in resistance due to temperature variations of the indicator (internal thermistor) and renal vein blood (external thermistor). The external thermistor was located on the external surface of the catheter, 2.5 cm proximal to the catheter tip. The analogue signals from the Wheatstone bridge, as well as arterial and venous pressures, were stored on a computer by using data acquisition software (AcqKnowledge Biopac, CA,). A proper position of the catheter was defined as one that yielded a variation of renal vein blood flow of no more than 10% in at least two consecutive measurements. Total RBF was assumed to be twice the blood flow to the left kidney. This technique for measurement of RBF has previously been described in detail [11, 19].
Administration and measurements of paraaminohippurate and chromium ethylenediaminetetraacetic
After blood and urine blanks were taken, an intravenous priming dose of PAH (8 mg/kg body weight) and 51Cr-EDTA (0.6 MegaBq/m2 body surface area) were given followed by an infusion at a constant rate individualised to body weight and serum creatinine. Serum concentrations of PAH and serum 51Cr-EDTA activity from arterial and renal vein blood samples as well as urinary samples were measured in duplicate by a spectrophotometer (Beckman DU 530, Life Science UV/Vis, Fullerton, CA) and a well counter (Wizard 3″, 1480, Perkin Elmer Turkuu, Finland), respectively.
Experimental procedure
Measurements started when the patients had a stable body temperature higher than 36.5°C, approximately 4–6 h after the end of cardiopulmonary bypass. The patients were mechanically ventilated and sedated with propofol (80±38 µg/kg per min) during the experimental procedure. After an equilibration period of at least 60 min, two 30-min urine collection periods (periods A and B) were begun. PAH and 51Cr-EDTA levels were obtained from arterial and renal vein blood samples at the end of each collection period. Thermodilution (TD) renal blood flow (RBFTD) was measured in duplicate at 10 and 20 min of each collection period. Systemic haemodynamics were obtained midway through each collection period. An indwelling Foley catheter carefully drained bladders. To improve retrieval of urine, a solution of sterile water (100 ml) was used for irrigation of the bladder together with gentle supra-pubic compression.
Calculated renal variables
Renal extractions of PAH (PAHEX) and 51Cr-EDTA (51Cr-EDTAEX) were derived according to the formula: (arterial concentration − renal vein concentration)/arterial concentration). Standard urinary clearance (UC) for PAH was corrected for by PAHEX to obtain renal plasma flow (RPFUC) and renal blood flow (RBFUC=RPFUC/1-hematocrit). Standard urinary clearance for 51Cr-EDTA was obtained as a measure of glomerular filtration rate (GFRUC). Renal filtration fraction derived from urinary clearances was defined as FFUC = GFRUC/RPFUC.
Renal extraction of 51Cr-EDTAEX is a direct measurement of renal filtration fraction (FFTD). Thermodilution glomerular filtration rate (GFRTD) can therefore be calculated as: RBFTD × (1-hematocrit) × 51Cr-EDTAEX.
Infusion clearance (IC) for PAH (PAH infusion rate/arterial PAH concentration) was corrected for by PAHEX to obtain renal plasma flow (RPFIC) and renal blood flow (RBFIC = RPFIC/1-hematocrit) without urine collection. Infusion clearance for 51Cr-EDTA (51Cr-EDTA infusion rate/arterial 51Cr-EDTA) was obtained as a measure of glomerular filtration rate (GFRIC) without urine collection. Filtration fraction obtained by infusion clearance was defined as GFRIC/RPFIC. All renal data were normalised to a body surface area of 1.73 m2.
Statistical analysis
Descriptive data analysis on RBF, GFR and FF from periods A and B was performed according to Bland and Altman [12]. The reproducibility of each of the three methods was assessed by the error (double standard deviation of the absolute differences divided by the mean of the repeated measurements), the repeatability coefficient (the double standard deviation of the absolute differences) and the mean coefficient of variation (standard deviation of the mean divided by the mean of repeated measurements).
The mean of the repeated measurements (periods A and B) of each variable for each method on each patient was calculated. The agreements between the “gold standard” urinary clearance method for estimation of RBF, GFR and FF and the two test methods, infusion clearance and renal vein thermodilution were assessed according to Bland and Altman [13]. The mean difference between two methods (bias) and the standard deviation of the differences were calculated as well as the error (double standard deviation divided by the mean of the measurements from the two methods) and the limits of agreement (mean difference ± two standard deviations). A priori we defined an acceptable within-method error to be 20% or less and an acceptable between-method error to be 30% or less, according to Critchley and Critchley [20]. The results are presented as means ± SD.
Results
Twenty patients were enrolled in this study. One patient was excluded because of development of heart failure requiring inotropic support during the experimental procedure. Another two patients were excluded because of urine sampling errors. The demographic data of the patients are presented in Table 1. Data on haemodynamics, mean serum PAH concentration (mg/100 ml), 51Cr-EDTA serum counts, PAHEX and 51Cr-EDTAEX are shown in Table 2. The mean coefficient of variation for serum PAH and 51Cr-EDTA serum counts were 5.0±3.5 and 3.3±2.4, respectively. The mean coefficient of variation for PAHEX and 51Cr-EDTAEX were 2.6±2.6 and 12.8±7.8, respectively.
Reproducibility within methods
The mean values of RBF for the three methods are seen in Fig. 1. RBFIC was higher (20%) and RBFTD was lower (−15%) than RBFUC. The error was highest for the thermodilution techniques and lowest for the infusion clearance technique. The coefficients of variation and the repeatability coefficients for RBFUC and RBFTD were of similar magnitudes, being higher than the corresponding values for RBFIC. The mean coefficient of variation for a duplicate measurement of RBFTD was 6.2±6.0. The importance of the catheter position for the achievement of renal vein blood flow is shown in Fig. 2.
The mean values of GFR for the urinary clearance, infusion clearance and the thermodilution techniques were 80.6±22.4, 89.5±24.7 and 71.3±23.1, respectively. The within-group errors for GFRUC, GFRIC and GFRTD were 32.5%, 10.8% and 63.6%, respectively. The repeatability coefficients for GFRUC, GFRIC and GFRTD were 26.2, 9.64 and 45.3 ml/min, respectively. The coefficients of variation for GFRUC, GFRIC and GFRTD were 10.2±10.4%, 3.3±2.4% and 14.8±13.1%, respectively.
The mean values of FF for the urinary clearance, infusion clearance and the thermodilution techniques were 0.17±0.04, 0.16±0.03 and 0.18±0.04, respectively. The within-group errors for FFUC, FFIC and FFTD were 30.5%, 17.5% and 42.1%, respectively. The repeatability coefficients for FFUC, FFIC and FFTD were 0.053, 0.028 and 0.075, respectively. The coefficients of variation for FFUC, FFIC and FFTD were 8.9±6.7, 5.1±3.6 and 13.2±7.7, respectively.
Agreement between methods
The agreements between RBFUC and RBFIC and between RBFUC and RBFTD are described in Fig. 3. The between-methods bias was −179 ml/min comparing RBFUC with RBFIC, while it was 123 ml/min comparing RBFUC with RBFTD. The error and the limits of agreement were higher comparing RBFUC with RBFTD than when comparing RBFUC with RBFIC.
Shows a continuous renal vein retrograde thermodilution recording from one patient. During the recording, the renal vein catheter was withdrawn approximately one centimetre (arrow), guided by fluoroscopy, which caused a change in the renal vein temperature corresponding to an increase in renal vein blood flow by approximately 30%. T ind indicator temperature, T blood renal vein blood temperature, RBF renal blood flow
The between-method bias was −11 ml/min comparing GFRUC with GFRIC, while it was 9 ml/min comparing GFRUC with GFRTD. The error was 42.5% and the limits of agreement were −48.0 to 25.4 ml/min comparing GFRIC with GFRUC. The corresponding values were 67.0% and −42.3 to 61.2 comparing GFRTD with GFRUC.
The between-method bias was 0.016 comparing FFUC with FFIC while it was −0.009 comparing FFUC with FFTD. The error was 50.7% and the limits of agreement were −0.67 to 0.099 comparing FFIC with FFUC. The corresponding values were 47.0% and −0.092 to 0.075 comparing FFTD with FFUC.
Discussion
The renal vein continuous thermodilution technique and the infusion clearance technique, for bedside estimation of absolute RBF, GFR and FF were validated in post-cardiac surgical patients. In a study of method comparison, assessment of within-method repeatability is important, because the repeatability of each of two methods limits the amount of agreement, which is possible [12, 21]. The repeatability was highest for the infusion clearance technique and lowest for the thermodilution technique with regard to RBF, GFR and FF. The gold standard method, the urinary clearance technique corrected for by PAHEX, had an unacceptably low repeatability, i.e. an error of 30–33%. It is therefore not surprising that the agreement between the infusion clearance and urinary clearance methods was relatively low, as, in the present study, the old gold standard method (urinary clearance) was more variable than the infusion clearance method. For the same reasons, the problem is even worse when comparing the thermodilution technique with the urinary clearance technique.
Since the original publication by Bland and Altman [12], clearly defined criteria as to whether one method could replace an older and more established one are lacking. In an attempt to clarify the criteria for accepting a newer technique, Critchley and Critchley suggested that acceptance of a new technique should rely on a between-methods error of up to 30% [20]. They could also demonstrate that the limits of within-group error of both the test and the reference method should be 20% or less to achieve a between-group error of 30% or less. In the present study, only the infusion clearance method fulfilled these criteria, with a within-method error less than 15% and a between-method error of 33% compared to the reference method.
The renal vein thermodilution technique has previously been described and validated using either a bolus [4, 9, 10] or a continuous infusion technique [11]. The renal vein thermodilution technique was found to correlate closely to the urinary clearance technique with a coefficient of correlation ranging from 0.77–0.89 with both the bolus and continuous infusion techniques [4, 9, 10, 11]. However, the agreement between the thermodilution and the urinary clearance techniques, according to Bland and Altman [12], has not been previously tested with regard to bias and within-, as well as, between-group errors. The relatively large bias and between-group error comparing the thermodilution technique with the reference method, as shown in the present study, might have several explanations. Thermodilution-derived absolute values of RBF assume that a single vein is present on the side of measurement, that equal blood flow is occurring to both kidneys, that there is minimal admixture of non-renal blood flow (spermatic, adrenal and ovarian) into the left renal vein and that there is complete mixing of the injectant with the blood. In our experience, a correct and stable position of the renal vein catheter thermistor in relation to the renal vein inflow of non-renal blood flows is the most critical factor for the estimation of total RBF. Small adjustments of the thermistor position may cause large variations in the renal venous flow measured, as illustrated in Fig. 2.
Plasma concentrations of PAH were stable during the experimental procedure, indicating that the rate of PAH infusion was equal to the rate of excretion. However, RBF values obtained by the infusion clearance method averaged 20% above the urinary clearance technique, indicating an extra-renal elimination of PAH. A similar magnitude of extra-renal elimination at steady state was demonstrated by Cole et al. both in patients with normal renal function and in patients with renal disease [15]. They attributed the observed differences between the urinary clearance and the infusion clearance for PAH to extra-renal conjugation of PAH.
It has repeatedly been shown that renal PAHEX approximates 0.9 in subjects with healthy kidneys [22, 23]. In the present study on post-cardiac surgical patients with preoperative normal renal function, mean PAHEX was 0.85 with a range from 0.72 to 0.99. Thus, if renal PAHEX were not measured in the present study, a potential error of 10–25% in estimated RBF would have been introduced at the most extreme deviations of PAHEX from 0.9. Brenner et al. showed, in septic and critically ill patients, that mean PAHEX was 56% with a range from 28–90% [4]. Furthermore, Myers et al. [5] demonstrated that mean PAHEX was only 43% in patients with early renal dysfunction after total renal ischaemia due to supra-renal clamping of the aorta. In other words, in post-cardiac surgical patients, and particularly in critically ill patients with acute renal dysfunction, the urinary clearance of PAH without correction for renal PAHEX would give invalid measurements of renal plasma flow. Another advantage with the use of a renal vein catheter is avoidance of the problem of obtaining perfectly constant arterial plasma concentrations of PAH after a pharmacological intervention with the aim to increase RBF [24]. Withdrawing arterial and renal venous blood simultaneously would allow repeated measurements of RBF at short intervals [24]. However, this needs to be tested in the intensive care setting.
Filtration fraction (FF) is defined as the relationship between GFR and RPF. Estimation of FF provides important information on the effects of various vasoactive agents on pre-glomerular (afferent) and post-glomerular (efferent) resistance vessels [25, 26, 27, 28]. Although the two independent methods for estimation of FF had approximately the same between-methods error when compared to the urinary clearance method, the within-group error was lowest for the infusion clearance technique. However, the estimation of FF by the infusion clearance method requires equilibrium between rate of excretion and infusion of 51Cr-EDTA and PAH [15, 16, 17], while repeated estimations of FF at short intervals are possible by measuring renal 51Cr-EDTAEX. However, one limitation with substances with low renal extraction, e.g. filtration markers, is that they may underestimate renal extraction in conditions with low renal plasma flow and high diuresis, i.e., when the arteriovenous flow difference might not be negligible [29].
In conclusion we have validated two independent methods for estimation of total RBF and GFR against the urinary clearance technique in the ICU setting. Although the renal vein thermodilution technique can be performed rapidly and repeatedly, this technique had the lowest reproducibility and a lower agreement with the reference method, when compared to the infusion clearance method. The infusion clearance method had the highest reproducibility when compared to both the urinary clearance and the renal vein thermodilution techniques and should therefore be considered as the reference method in future studies on renal haemodynamics and function in the ICU setting.
References
Block CA, Manning HL (2002) Prevention of acute renal failure in the critically ill. Am J Respir Crit Care Med 165:320–324
Brezis M, Rosen S (1995) Hypoxia of the renal medulla—its implications for disease. N Engl J Med 332:647–655
Smith HW, Finkelstein N, Aliminosa L, Crawford B (1945) The renal clearance of substituted hippuric acid derivates and other aromatic acids in dog and man. J Clin Invest 24:338–324
Brenner M, Schaer GL, Mallory DL, Suffredini AF, Parrillo JE (1990) Detection of renal blood flow abnormalities in septic and critically ill patients using a newly designer indwelling thermodilution renal vein catheter. Chest 98:170–179
Myers BD, Miller DC, Mehigan JT, Olcott CO 4th, Golbetz H, Robertson CR, Derby G, Spencer R, Friedman S (1984) Nature of the renal injury following total renal ischemia in man. J Clin Invest 73:329–341
Corrigan G, Ramaswamy D, Kwon O, Sommer FG, Alfrey EJ, Dafoe DC, Olshen RA, Scandling JD, Myers BD (1999) PAH extraction and estimation of plasma flow in human postischemic acute renal failure. Am J Physiol 277:F312–318
Levinsky NG, Levy M (1973) Clearance techniques. In: Orloff J, Berliner RW (eds) Handbook of Physiology, section 8, Renal Physiology, part 4. Waverly Press, Baltimore, pp 103–117
Caron N, Kramp R (1999) Measurement of changes in glomerular filtration rate induced by atrial natriuretic peptide in the rat kidney. Exp Physiol 84:689–696
Hornych A, Brod J, Slechta V (1971) The measurement of the renal venous outflow in man: the local thermodilution method. Nephron 8:17–32
Leivestad T, Brodwall EK, Simonsen S (1978) Determination of renal blood flow by thermodilution method. Scand J Clin Lab Invest 38:495–499
Haywood GA, Stewart JT, Counihan PJ, Sneddon JF, Tighe D, Bennet ED, McKenna WJ (1992) Validation of bedside measurements of absolute human renal blood flow by a continuous thermodilution technique. Crit Care Med 20:659–664
Bland JM, Altman DG (1986). Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8746):307–310
Earle DP, Berliner RW (1946) A simplified clinical procedure for measurement of glomerular filtration rate and renal plasma flow. Proc Soc Exp Biol Med 62:262–264
Rose GA (1969) Measurement of glomerular filtration rate by insulin clearance without urine collection. BMJ 2:91–93
Cole BR, Giangiacomo J, Ingelfinger JR, Robson AM (1972) Measurement of renal function without urine collection. A critical evaluation of the constant-infusion technic for determination on inulin and para-aminohippurate. N Engl J Med 287:1109–1114
Schnurr E, Lahme W, Kuppers H (1980) Measurement of renal clearance of inulin and PAH in the steady state without urine collection. Clin Nephrol 13:26–29
Ganz W, Tamura K, Marcus HS, Donoso R, Yoshida S, Swan HJ (1971) Measurement of coronary sinus blood flow by continuous thermodilution in man. Circulation 44:181–195
Tidgren B, Brodin U (1988) Plasma renin activity and oxygen content along the renal vein in hypertensive patients. Clin Physiol 8:407–416
Tidgren B, Hjemdahl P (1988) Reflex activation of renal nerves in humans: differential effect on noradrenaline, dopamine and renin overflow to renal vein plasma. Acta Physiol Scand 134:23–34
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15:85–91
Mantha S, Roizen MF, Fleisher LA, Thisted R, Foss J (2000) Comparing methods of clinical measurement: reporting standards for Bland and Altman analysis. Anesth Analg 90:593–602
Aurell M (1969) Renal response in man to plasma volume expansion and angiotensin. Scand J Clin Lab Invest 112 (Suppl):1–59
Battilana C, Zhang HP, Olshen RA, Wexler L, Myers BD (1991) PAH extraction and estimation of plasma flow in diseased human kidneys. Am J Physiol 261:F726–733
Aurell M, Fritjofsson A, Grimby G (1966) Renal extraction of para-aminohippurate during variations in renal blood flow and tubular load in man. Clin Sci 31:461–471
Valsson F, Ricksten SE, Hedner T, Zall S, William-Olsson EB, Lundin S (1994) Effects of atrial natriuretic peptide on renal function after cardiac surgery and in cyclosporine-treated heart transplant recipients. J Cardiothorac Vasc Anesth 8:425–430
Valsson F, Ricksten SE, Hedner T, Lundin S (1996) Effects of atrial natriuretic peptide on acute renal impairment patients with heart failure after cardiac surgery. Intensive Care Med 22:230–236
Sward K, Valson F, Ricksten SE (2001) Long-term infusion of atrial natriuretic peptide (ANP) improves renal blood flow and glomerular filtration rate in clinical acute renal failure. Acta Anaesthesiol Scand 45:536–542
Mathur VS, Swan SK, Lambrecht LJ, Anjum S, Fellman J, McGuire D, Epstein M, Luther RR (1999) The effects of fenoldopam, a selective dopamine receptor agonist, on systemic and renal hemodynamics in normotensive subjects. Crit Care Med 27:1832–1837
Andersson LG, Bratteby LE, Ekroth R, Wesslen O, Hallhagen S (1994) Calculation of renal extraction during high diuresis and low renal plasma flow conditions. Clin Physiol 14:79–85
National Kidney Foundation. K/DOQI (2002) Clinical practice guidelines for chronic kidney disease; evaluation, classification and stratification. Am J Kidney Dis 39 (Suppl):S76–S92
Acknowledgements
Grants from the Swedish Medical Research Council (no. 13156), Medical Faculty of Göteborg (LUA), and Göteborg Medical Society supported this study. The technical assistance of Mrs Marita Ahlqvist is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Swärd, K., Valsson, F., Sellgren, J. et al. Bedside estimation of absolute renal blood flow and glomerular filtration rate in the intensive care unit. Intensive Care Med 30, 1776–1782 (2004). https://doi.org/10.1007/s00134-004-2380-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2380-8