Abstract
Objective
Prevention of secondary insults, such as hyperthermia, is a major goal after traumatic brain injury. The aim of our study was to identify risk factors for early hyperthermia in severe head-injured patients.
Design
Retrospective cohort study.
Setting
A 17-bed multidisciplinary ICU of a 700-bed teaching hospital.
Patients
A total of 101 adult patients admitted from January 1999 to December 2001 requiring continuous monitoring of intracranial pressure according to international guidelines.
Measurement and results
Forty-four patients experienced early hyperthermia (at least one episode of body temperature >38.5°C within the first 2 days). On univariate analysis five variables were associated with early hyperthermia: sex; body temperature; white blood cell count on admission; prophylactic use of acetaminophen; and diabetes insipidus within 2 days. On multivariate analysis, white blood cell count >14.5×109/l on admission (odds ratio, 7.1; 95% confidence interval, 2.4–20.5; p=0.001) and a body temperature on admission >36°C (odds ratio, 6.7; 95% confidence interval, 2.3-20.1) were strong risk factors of early hyperthermia. Prophylactic use of acetaminophen was negatively associated with early hyperthermia (odds ratio, 0.1; 95% confidence interval, 0.02–0.4). Patients who experienced early hyperthermia were less prone to have good recovery (GOS=5; p=0.03). More patients with severe or moderate disability (GOS=3 or 4) experienced early hyperthermia (p=0.01).
Conclusion
We identified a subgroup of patients at high risk of early hyperthermia, which is common in severe head-injured patients. These results could have clinical implications for prevention of hyperthermia after traumatic brain injury in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperthermia is a common issue in neurological intensive care unit (ICU) and is associated with a poor neurological outcome in stroke and spontaneous subarachnoid hemorrhage [1, 2, 3, 4, 5]. In a study including 390 stroke patients, Reith et al. found that for each 1°C increase in body temperature on admission, the relative risk of poor outcome rose by 2.2 [3]. Although less studied, hyperthermia following traumatic brain injury (TBI) is also known to increase morbidity and mortality [6, 7].
Pathophysiological links between hyperthermia and outcome following brain injuries are not clear. Experimental studies have shown that brain injury is worsened when hyperthermia (even 1 or 2°C) is superimposed to an ischemic (focal or global) lesion [8, 9, 10, 11], which is common after severe TBI [12]. Both human and animal studies have shown that the extent of cerebral damage is related to the timing of hyperthermia onset with a poorer outcome when hyperthermia occurs soon after injury [13, 14, 15].
Pathogenesis of hyperthermia in head trauma patients is related to several causes and mechanisms including: (a) inflammatory cascade due to tissue attrition; (b) catecholergic stimulation; (c) direct damage to cerebral centers of thermoregulation; or (d) infection.
The aim of our study was to identify risk factors of early hyperthermia (within two days) and related consequences of this event on outcome in a population of severe adult TBI patients.
Materials and methods
Study population and design
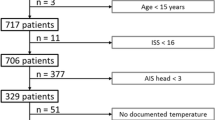
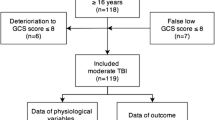
According to French legislation, no informed consent is needed to use data for an epidemiological study. We performed a retrospective observational cohort study on prospectively collected data in consecutive severe head trauma patients admitted to a 17-bed surgical ICU of a French teaching hospital (Hôpital Beaujon, Clichy, France). The inclusion criteria were an age higher than 18 years and a head trauma requiring an intracranial pressure (ICP) monitoring. The study period began in January 1999 and ended in December 2001. Indication for ICP monitoring was in agreement with international guidelines for head trauma: (a) Glasgow coma scale score (GCS) <8 after cardiopulmonary resuscitation with an abnormal admission cranial computed tomography (CT) scan; (b) GCS <8 with a normal CT scan with two or more of the following features noted on admission: age over 40 years, unilateral or bilateral motor deficit, systolic blood pressure (SBP) <90 mmHg; and (c) moderate head injury in case of traumatic mass lesions with a decreasing level of consciousness [16]. Exclusion criterion was death within the first 2 days.
Patient management
The initial management of these patients was performed on the scene of the accident by a medical team. This prehospital management included GCS determination and sedation, intubation, and ventilation when needed. Patient care (including the prehospital period) was delivered according to recommendations of the French society of anesthesiology and critical care on initial management of the severely head-injured patients [17]. A metallic survival blanket was used for all patients during transport to hospital. After determination of GCS score as well as intentional sedation with fentanyl and midazolam was used for all patients. Cerebral perfusion pressure (CPP) was maintained above 70 mm Hg with vasopressor (norepinephrine), if necessary. Refractory intracranial hypertension was treated by barbiturate (Thiopental). No intentional hypothermia was used. Management of hyperthermia, antibiotherapy, and prophylactic use of acetaminophen were left to discretion of physician in charge of the patient. The ICP was measured with an intraparenchymal probe (Codman, Johnson and Johnson Company, Raynham, Mass.). Blood and urine cultures were performed systematically when the body temperature was higher than 38.5°C. Ventilator-associated pneumonia was suspected when several criteria were associated with hyperthermia: new and/or progressive pulmonary infiltrate on chest X-ray and one of the following criteria: leukocytosis (≥12,000/mm3) or leukopenia (≤4000/mm3) and purulent tracheobronchial secretions. Ventilator-associated pneumonia was then confirmed with an invasive method using a fiberoptic bronchoscope by protected specimen brush growing ≥103 colony forming unit (CFU)/ml [18]. The final decision concerning presence or absence of infection was made by the physician in charge of the patient. When possible, nutritional support was performed by enteral nutrition started within the first 48 h via orogastric tube by a mixture containing glucose 50%, lipid 35%, and protein 15% (Sondalis, Nestle). No patient received intravenous glucose infusion within the first 48 h.
Data collection
The following data were gathered:
-
1.
Gender, GCS score on scene, cause of injury, findings on initial cranial CT scan, associated injuries, Simplified Acute Physiology Score (SAPS) II, Injury Severity Score (ISS)
-
2.
Body temperature, white blood cell count (WBC), and glycemia on admission
-
3.
Highest and mean temperature, highest and mean ICP, lower and mean CPP, early arterial hypotension, occurrence of diabetes insipidus, seizures, and neurosurgery within the first 2 days.
-
4.
Use of barbiturates, myorelaxant agent, vasoconstrictor, acetaminophen, and total dose of acetaminophen within the first 2 days.
-
5.
Length of ventilation, length of ICU stay, and the five-point Glasgow Outcome Scale (GOS) 6 months after injury [19].
Definitions
Early hyperthermia was defined by at least one measurement of body temperature higher than 38.5°C within the first 2 days. Body temperature was measured using an infrared tympanic thermometer (Genius 3000A, Sherwood Medical, St. Louis, Mo.) every 3 h. Initial GCS was reported by attending physicians on arrival on scene after cardiopulmonary resuscitation. Early arterial hypotension was defined as any episode of systolic blood pressure below 90 mmHg during the first 24 h of care. Early diabetes insipidus episode was defined by the association of polyuria with urinary gravity <1.005, absence of glycosuria, and natremia >145 mmol/l (normal value between 135 and 145 mmol/l) within the first 2 days. Associated traumatic lesions were diagnosed on body CT scan performed in all patients on arrival.
Use of acetaminophen was considered as prophylactic if infused before body temperature has reached 38.5°C. Acetaminophen was administered intravenously (Pro-Dafalgan, Laboratoires UPSA, Rueil-Malmaison,France) in a 30-min period diluted with 100 ml of saline serum with a maximum dose of 4 g a day. Each infused vial contained 2 g of propacetamol (yielding 1 g of acetaminophen).
Evaluation of the five-point GOS was performed by a neurosurgeon blinded to occurrence of early hyperthermia.
Statistical analyses
All results are expressed as mean±standard deviation or as a ratio of total patients. Qualitative variables were compared using chi-square test or Fisher’s exact test (two sided) when needed. Continuous variables were compared using Student’s t test. A multivariate analysis was performed to determine risk factors of early hyperthermia using a logistic regression taking variables with a p≤0.05 into account after univariate analysis. Threshold values were specified before statistical study. Data are presented in Table 1 including coefficient of the explanatory variable and the associated standard error, odds ratio, 95% confidence interval of the odds ratio, and p value (quoted with the Wald χ2 test). Explanatory variables were assessed for colinearity and tested for interaction.
Statistical analysis was performed using Statview 5.0 Software (SAS institute, Cary, N.C.) and JMP 3.0 Software (SAS institute, Cary, N.C.).
Results
One hundred seven head trauma patients fulfilling the inclusion criteria were admitted during the 2-year study period. Six patients died in the first 2 days. The remaining 101 patients had a mean age of 33±15 years, were mainly male, and 74 were multiple trauma patients. Cause of injury was: motor vehicle crash (n=21); motorcycle accident (n=27); fall (n=16); pedestrian accident (n=33); and assault (n=4). They had a mean SAPS 2 score of 38±11, an ISS score of 35±9, a mean GCS on admission of 7±2, and 25 patients underwent urgent neurosurgery. Mean body temperature on admission was 36.4±1.3°C. Sixty patients had a WBC >14.5×109/l on admission. Length of stay was 23±14 days and 22 patients died in ICU. Cranial CT scan findings were: diffuse edema (n=57); petechial lesions (n=19); intracerebral hematoma (n=69); and subarachnoid hemorrhage (n=41). Clinical events in the first 2 days and outcome are listed in Table 2.
Forty-four patients experienced early hyperthermia. Mean temperature within the first 2 days was 36.8±1.0°C. Forty-nine patients received acetaminophen: 21 for prevention of hyperthermia and 29 for treatment of hyperthermia. Mean dose of acetaminophen used in prevention was 3.5±1.5 g within first 2 days.
On univariate analysis, three variables were positively associated with the occurrence of early hyperthermia: sex; WBC on admission; and admission body temperature >36°C. Conversely, prophylactic use of acetaminophen and early occurrence of central diabetes insipidus were negatively associated with occurrence of early hyperthermia (see Table 1 for details).
On multivariate analysis three independent variables remained associated with the occurrence of early hyperthermia. WBC >14.5×109/l on admission and temperature >36°C on admission were positively associated with early hyperthermia. Prophylactic use of acetaminophen was negatively associated with early hyperthermia (see Table 3 for details). We found no colinearity as well as no interaction between independent variables.
Long-term outcome showed that patients who experienced early hyperthermia were less prone to have good recovery (GOS=5; p=0.03). More patients with severe or moderate disability (GOS=3 or 4) experienced early hyperthermia (p=0.01). Number of patients dead or vegetative were not different between patients with or without occurrence of early hyperthermia. These results are listed in Table 2. No episode of early hyperthermia was related to infection.
Discussion
In this study, several risk factors of early hyperthermia following TBI were identified. A WBC>14.5×109/l and a body temperature >36°C on admission were strongly associated with the occurrence of at least one episode of hyperthermia within 2 days. Conversely, prophylactic use of acetaminophen was negatively associated with occurrence of early hyperthermia.
An association between post-traumatic leukocytosis and early hyperthermia after TBI has been previously reported by Natale et al. in a pediatric population [20]. Post-traumatic leukocytosis seems to correlate with cerebral damage and outcome after TBI [21]. Hyperthermia and leukocytosis are linked by common explanatory mechanisms including catecholaminergic discharge and inflammatory response. Brain trauma is associated with a dramatic adrenergic discharge inducing several biological and clinical specific consequences such as hypokaliemia, leukocytosis, or hemodynamic response. This sympathetic response is closely related to the severity of initial brain injury [22]; hence, releasing of neutrophils store by catecholamine could account for a major part in post-traumatic leukocytosis [21]. Brain trauma induces an acute local and systemic inflammatory cascade through the activation of immune cells with release of pyrogenic cytokines such as IL-1, IL-6, or TNF [23, 24, 25] following by a compensatory anti-inflammatory response [26]; however, overactivity of sympathetic tone may interact with the inflammatory response following cerebral lesions by enhancing production of anti-inflammatory cytokines such as IL-10 [27]. We may infer that links between early high WBC and hyperthermia are part of a complex mechanism of adrenergic and inflammatory response in which hyperthermia and leukocytosis are only prominent and visible signs.
In our study, normal temperature on arrival in ICU was associated with early hyperthermia. Several studies have shown that hypothermia is associated with poor outcome in multiple trauma patients [28, 29]; however, this concerns deep hypothermia (<33°C). The natural evolution of temperature in a trauma patient is to decrease in a cold environment [30]. Prehospital care tends to attenuate body heat loss by exposing the trauma patient to a warm environment. The relationship found between temperature on admission and early hyperthermia in our study could be due to the fact that major determinant of early hyperthermia (i.e., inflammatory cascade and catecholergic response) could occur very early in the course of post-trauma period.
At the time of the study there were no guidelines for prevention or treatment of hyperthermia after TBI. The rationale for the use of antipyretic agents in severe head trauma is to limit neurological consequences of hyperthermia. Hyperthermia worsens ischemic lesions, enhances brain swelling by increasing vascular permeability [31], and increases CO2 production with rise of intracranial pressure. Acetaminophen was the drug used in our ICU to treat and/or prevent hyperthermia. Acetaminophen is widely used in ICU for pain relief or fever treatment and is considered safe providing that the daily dose does not exceed 4 g. We found that acetaminophen infused before patients reach a temperature >38.5°C was a negative independent risk factor of early hyperthermia. Since there was no protocol for its use, no definitive conclusion can be drawn from our results.
On univariate analysis, occurrence of central diabetes insipidus was negatively associated with early hyperthermia. Two assumptions can be formulated to explain this association: firstly, patients with diabetes insipidus receive more fluid to compensate water loss, which can decrease body temperature. Secondly, central diabetes insipidus is due to either intracranial hypertension or direct post-pituitary injury. Thermoregulator centers are located close to this region and their function could be impaired in patients with occurrence of diabetes insipidus; however, when thermoregulator centers are impaired, it is usually hyperthermia which occurs [32]. In our study, initial cranial CT scan did not reveal any direct hypothalamic injury knowing that magnetic resonance imaging is a better tool to detect such lesions.
The incidence of early hyperthermia was higher in patients with intermediate outcome (GOS 3 or 4) than those who had a good recovery (GOS 5). Interpretation of these results are difficult because severity of lesion and hyperthermia can be considered as either causes or consequences because (a) severe cerebral lesion may be the cause of early hyperthermia, or (b) hyperthermia may aggravate cerebral lesion and then be associated with a worse outcome. Occurrence of early hyperthermia was not associated with a worse early outcome and long-term bad outcome (persistent vegetative state and dead). These results may also suggest that less severe lesions are prone to worsen with hyperthermia and more severe lesions are insensitive to the aggravation consequences of hyperthermia due to the fact that primary injury account for a major part of prognosis; however, our study was not designed to answer the question of the impact of early hyperthermia on neurological recovery, and therefore, drawing conclusions based on our results should be done cautiously.
In our study we did not find any association between the type of cerebral lesions found on initial CT scan and early hyperthermia. A recent study on risk factors of hyperthermia in a neurological intensive care has found a strong association between spontaneous subarachnoid hemorrhage and fever during ICU hospitalization [33]. This discrepancy can be explained in two ways: 1. Despite common characteristics, such as time course of vasospasm, traumatic and spontaneous (aneurysmal) subarachnoid hemorrhage have different pathophysiological mechanisms and clinical course [34, 35]. 2. We only studied hyperthermia occurring within 2 days after trauma. Concerning the other initial cerebral lesions, Natale et al. showed an association between two types of lesion (i.e., cerebral edema axonal and diffuse axonal injury) and early hyperthermia [20]. In this study, no logistic regression analysis was performed to confirm the above associations found in univariate analysis. Moreover, we studied adult patients, whereas Natale et al. [20] studied pediatric patients. Consequences of intracerebral lesions might be different depending on age. In a recent study by Thompson et al., two other types of cerebral lesions (i.e., diffuse axonal injury and frontal injury of any type) were associated with neurogenic fever, a possible sequela after severe head injury [36]. In this study, early hyperthermia was not predictive of neurogenic fever confirming that these two entities were distinct with probably different pathophysiological mechanisms.
Hyperthermia is a challenging (and costly) condition in intensive care and is often considered as a surrogate marker of infection; however, a recent study showed that at least half of fever episodes in ICU course’s patient were not due to septic conditions [37]. In our study no episode of early hyperthermia was related to bacteriological infection. As a consequence, maintaining normothermia with phamacological or physical interventions should not expose to misdiagnosis of infection in the first 2 days following head trauma.
Our findings may have implications for clinical practice. Until now, studies on intentional mild hypothermia have failed to show an improvement of outcome in traumatic brain injured patients [38]; however, hyperthermia is commonly considered and treated as a secondary major insult in this population. We suggest that head trauma adult patient presenting a body temperature >36°C and/or a WBC>14.5×109/l on admission should undergo careful management of temperature. Prophylactic treatment using acetaminophen could be of interest in these patients knowing that this treatment will not affect root causes of hyperthermia.
References
Azzimondi G, Bassein L, Nonino F, Fiorani L, Vignatelli L, Re G, D’Alessandro R (1995) Fever in acute stroke worsens prognosis. A prospective study. Stroke 26:2040–2043
Jorgensen HS, Reith J, Nakayama H, Kammersgaard LP, Raaschou HO, Olsen TS (1999) What determines good recovery in patients with the most severe strokes? The Copenhagen Stroke Study. Stroke 30:2008–2012
Reith J, Jorgensen HS, Pedersen PM, Nakayama H, Raaschou HO, Jeppesen LL, Olsen TS (1996) Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome. Lancet 347:422–425
Oliveira-Filho J, Ezzeddine MA, Segal AZ, Buonanno FS, Chang Y, Ogilvy CS, Rordorf G, Schwamm LH, Koroshetz WJ, McDonald CT (2001) Fever in subarachnoid hemorrhage: relationship to vasospasm and outcome. Neurology 56:1299–1304
Kilpatrick MM, Lowry DW, Firlik AD, Yonas H, Marion DW (2000) Hyperthermia in the neurosurgical intensive care unit. Neurosurgery 47:850–856
Jones PA, Andrews PJ, Midgley S, Anderson SI, Piper IR, Tocher JL, Housley AM, Corrie JA, Slattery J, Dearden NM et al. (1994) Measuring the burden of secondary insults in head-injured patients during intensive care. J Neurosurg Anesthesiol 6:4–14
Jiang JY, Gao GY, Li WP, Yu MK, Zhu C (2002) Early indicators of prognosis in 846 cases of severe traumatic brain injury. J Neurotrauma 19:869–874
Baena RC, Busto R, Dietrich WD, Globus MY, Ginsberg MD (1997) Hyperthermia delayed by 24 hours aggravates neuronal damage in rat hippocampus following global ischemia. Neurology 48:768–773
Kim Y, Busto R, Dietrich WD, Kraydieh S, Ginsberg MD (1996) Delayed postischemic hyperthermia in awake rats worsens the histopathological outcome of transient focal cerebral ischemia. Stroke 27:2274–2281
Dietrich WD, Alonso O, Halley M, Busto R (1996) Delayed posttraumatic brain hyperthermia worsens outcome after fluid percussion brain injury: a light and electron microscopic study in rats. Neurosurgery 38:533–541
Dietrich WD, Busto R, Valdes I, Loor Y (1990) Effects of normothermic versus mild hyperthermic forebrain ischemia in rats. Stroke 21:1318–1325
Graham DI, Ford I, Adams JH, Doyle D, Teasdale GM, Lawrence AE, McLellan DR (1989) Ischaemic brain damage is still common in fatal non-missile head injury. J Neurol Neurosurg Psychiatry 52:346–350
Busto R, Dietrich WD, Globus MY, Valdes I, Scheinberg P, Ginsberg MD (1987) Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 7:729–738
Ginsberg MD, Sternau LL, Globus MY, Dietrich WD, Busto R (1992) Therapeutic modulation of brain temperature: relevance to ischemic brain injury. Cerebrovasc Brain Metab Rev 4:189–225
Castillo J, Davalos A, Marrugat J, Noya M (1998) Timing for fever-related brain damage in acute ischemic stroke. Stroke 29:2455–2460
Brain Trauma Foundation (1996) Guidelines for the management of severe head injury. American Association of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care. J Neurotrauma 13:641–734
Recommandations pour la pratique clinique (1999) Prise en charge des traumatisés craniens graves à la phase précoce. Ann Fr Anesth Reanim 18:5–159
Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165:867–903
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1:480–484
Natale JE, Joseph JG, Helfaer MA, Shaffner DH (2000) Early hyperthermia after traumatic brain injury in children: risk factors, influence on length of stay, and effect on short-term neurologic status. Crit Care Med 28:2608–2615
Rovlias A, Kotsou S (2001) The blood leukocyte count and its prognostic significance in severe head injury. Surg Neurol 55:190–196
Clifton GL, Ziegler MG, Grossman RG (1981) Circulating catecholamines and sympathetic activity after head injury. Neurosurgery 8:10–14
Shohami E, Novikov M, Bass R, Yamin A, Gallily R (1994) Closed head injury triggers early production of TNF alpha and IL-6 by brain tissue. J Cereb Blood Flow Metab 14:615–619
Fan L, Young PR, Barone FC, Feuerstein GZ, Smith DH, McIntosh TK (1995) Experimental brain injury induces expression of interleukin-1 beta mRNA in the rat brain. Brain Res Mol Brain Res 30:125–130
Young AB, Ott LG, Beard D, Dempsey RJ, Tibbs PA, McClain CJ (1988) The acute-phase response of the brain-injured patient. J Neurosurg 69:375–380
Morganti-Kossmann MC, Rancan M, Stahel PF, Kossmann T (2002) Inflammatory response in acute traumatic brain injury: a double-edged sword. Curr Opin Crit Care 8:101–105
Woiciechowsky C, Asadullah K, Nestler D, Eberhardt B, Platzer C, Schoning B, Glockner F, Lanksch WR, Volk HD, Docke WD (1998) Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nat Med 4:808–813
Jurkovich GJ, Greiser WB, Luterman A, Curreri PW (1987) Hypothermia in trauma victims: an ominous predictor of survival. J Trauma 27:1019–1024
Danzl DF, Pozos RS, Auerbach PS, Glazer S, Goetz W, Johnson E, Jui J, Lilja P, Marx JA, Miller J et al. (1987) Multicenter hypothermia survey. Ann Emerg Med 16:1042–1055
Peng RY, Bongard FS (1999) Hypothermia in trauma patients. J Am Coll Surg 188:685–696
Dietrich WD, Halley M, Valdes I, Busto R (1991) Interrelationships between increased vascular permeability and acute neuronal damage following temperature-controlled brain ischemia in rats. Acta Neuropathol (Berl) 81:615–625
Carpenter MB, Sutin J (1983) Hypothalamus. In: Carpenter MB, Sutin J (eds) Human anatomy. Williams and Wilkins, Baltimore, pp 552–578
Commichau C, Scarmeas N, Mayer SA (2003) Risk factors for fever in the neurologic intensive care unit. Neurology 60:837–841
Harders A, Kakarieka A, Braakman R (1996) Traumatic subarachnoid hemorrhage and its treatment with nimodipine. German tSAH Study Group. J Neurosurg 85:82–89
Martin NA, Doberstein C, Zane C, Caron MJ, Thomas K, Becker DP (1992) Posttraumatic cerebral arterial spasm: transcranial Doppler ultrasound, cerebral blood flow, and angiographic findings. J Neurosurg 77:575–583
Thompson HJ, Pinto-Martin J, Bullock MR (2003) Neurogenic fever after traumatic brain injury: an epidemiological study. J Neurol Neurosurg Psychiatry 74:614–619
Circiumaru B, Baldock G, Cohen J (1999) A prospective study of fever in the intensive care unit. Intensive Care Med 25:668–673
Clifton GL, Miller ER, Choi SC, Levin HS, McCauley S, Smith KR Jr, Muizelaar JP, Wagner FC Jr, Marion DW, Luerssen TG, Chesnut RM, Schwartz M (2001) Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med 344:556–563
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Geffroy, A., Bronchard, R., Merckx, P. et al. Severe traumatic head injury in adults: Which patients are at risk of early hyperthermia?. Intensive Care Med 30, 785–790 (2004). https://doi.org/10.1007/s00134-004-2280-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2280-y