Abstract
Objective
To determine the incidence and severity of symptoms related to the diagnosis of post-traumatic stress disorder (PTSD) in a cohort of general ICU patients.
Design
A prospective cohort study 3 months after general ICU discharge.
Setting
A general ICU in a teaching hospital in northern Scotland.
Patients and participants
Seventy-eight ICU survivors of general ICU.
Interventions
Patients were contacted 3 months after ICU discharge and asked to complete a telephone assessment of the Davidson Trauma Scale.
Measurements and results
The median score was 8, with 22% recording a score of at least 27 and 14% meeting the full diagnostic criteria for PTSD. The overall score was not correlated with sex, ICU length of stay, or APACHE II score but was inversely correlated with age and directly correlated with length of mechanical ventilation. The overall score was also related to the patient reporting having visited a GP or a mental health professional for psychological distress previous to ICU.
Conclusions
We found a high incidence of symptoms consistent with PTSD 3 months after ICU discharge in this general ICU cohort. This was associated with younger patients and those who visited their GP or a mental health professional complaining of psychological symptoms. Further research and a greater liaison between ICU staff and family practitioners and mental health practitioners is required to better identify individuals at risk and reduce psychological morbidity in this group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychological reactions to traumatic events (TE) are clinically important and common, with post-traumatic stress disorder (PTSD) having a lifetime prevalence in community samples of 1.3–12% [1, 2]. PTSD is a complex, chronic and severe disorder with high rates of psychiatric co-morbidity and substantial costs to the individual and to society both in terms of psychosocial well-being and financial consequences [2]. Research has shown that in addition to the potential for chronic distress there can be detrimental effects upon day-to-day functioning, education, employment and marriage [2]. Whilst no single type of trauma always causes psychological disturbance factors relating to the trauma, individual vulnerability and the perception of the traumatic event have been identified as important in producing the disorder [3]. Further, the complexity of the post-traumatic reactions is demonstrated by conflicting reports regarding the relationship of physical injury to psychopathology. Psychological sequelae have been shown in some studies to be high when individuals are physically injured whilst other groups have reported no relationship with the actual severity of the physical injury [4, 5, 6].
Few studies have examined the general psychological outcome or occurrence of PTSD after acute or critical medical events, and this morbidity may therefore go unrecognised [7]. Much of the current knowledge about the effects of critical illness is derived from the study of burns with a review describing varied incidences found for PTSD of between 8% and 45% [8]. Patients experiencing major burns have been found commonly to experience both early and late symptoms of stress, with early symptoms suggested to be related to the development of PTSD [9]. However, caution should be exercised when generalising from one group of survivors of critical illness to another [10].
Michaels and colleagues [11] report an incidence of PTSD of 42% in a clinical sample 6 months after major neurotrauma. However, the incidence of PTSD was low in severely injured accident victims who were physically and psychologically healthy before the traumatic event. The study of widely accepted predictive factors for PTSD relating to the traumatic event have produced variable results in studies of the critically ill or injured [12]. Whilst some studies have supported psychosocial variables and the presence of high scores for neuroticism and low scores for extraversion, others fail to demonstrate this and have found no relationship between the pre-morbid psychosocial state and post-traumatic psychopathology [13, 14, 15].
Little attention has been paid to the occurrence of PTSD and related disorders in general critically ill patients who have not been involved in accidents or assaults. The few studies which have been carried out report contradictory results. Features of potential interest to intensive care physicians such as severity of illness and the individual's perception of threat to life have been suggested by some researchers to be related to the severity and incidence of PTSD [16, 17]. Patients undergoing cardiac surgery followed by intensive care management were found to have an incidence of PTSD of 18% [18]. In addition, these patients complained of a lower quality of life than those without psychological symptoms [18]. Other studies have reported the incidence of PTSD in ICU patients to be between 27% and 41% depending on the sample characteristics [19, 20].
Psychological symptoms have been shown to occur commonly in various cohorts of critically ill patients [8, 9, 11, 21, 22]. Considerable effort is undertaken to reduce the high morbidity and mortality during and immediately after ICU care. However, much still needs to be learned regarding features such as the incidence of severe psychological problems, the return of quality of life and the effects of employment difficulties. These are thought to be important measures of outcome in the critically ill, and post-traumatic employment difficulties have been found to be related to high levels of psychopathology (both acutely and chronically) in other trauma populations [4, 21].
Early research in this area has been fraught with methodological problems including: the lack of validated measures, sampling problems such as small sample size and sampling bias, and the use of inappropriate measures such as the Hospital Anxiety and Depression Scale (HADS) [23]. The HADS is a well-validated 14-item questionnaire with anxiety and depression subscales. It avoids questions on somatic complaints that could introduce bias in physically injured individuals, but it does not ask about the core symptoms of PTSD. For example, Eddleston and colleagues [21] report that 9.8% of their patients required specialist mental health intervention for psychological problems within 3 months of discharge from ICU. The authors suggest that few patients would fulfil criteria for PTSD, yet they used the HADS rather than a validated measure for PTSD, and thus few specific post-traumatic symptoms would be identified. Many instruments have been developed to assess post-traumatic reactions, in particular PTSD. Self-report questionnaires such as the Impact of Event Scale-Revised version [24] and the Davidson Trauma Scale (DTS) [25] cover the core symptom clusters of PTSD, namely intrusive phenomena (e.g. nightmares and flashbacks), avoidance (e.g. of reminders of the event), and hyperarousal (e.g. insomnia and hypervigilance). The DTS has been used widely in the initial assessment of patients who have undergone a traumatic event that could be related to the development of PTSD. The DTS measures all 17 primary PTSD symptoms relating to the three main symptom areas with specific criteria for both frequency and intensity rated in relation to the past week. The maximum total score is 136.
The aim of our study was to quantify the incidence and risk factors for symptoms related to the diagnosis of PTSD using a measure validated in a variety of trauma populations in a general cohort of critically ill patients requiring ICU care 3 months after discharge.
Materials and methods
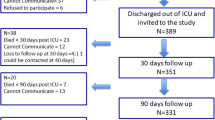
The requirement for informed consent was waived by the Institutional Review Board as the study was an observational audit of clinical practice. Were approached 111 consecutive general ICU survivors at the time of ICU discharge, and all agreed to participate in the study. There were no exclusion criteria. Three months after ICU discharge all patients were contacted by a research nurse by telephone and asked to complete a short structured interview and a telephone assessment of the DTS [25]. Of the 111 patients originally enrolled into the study 78 (70%) completed the protocol. Reasons for non-completion of the survey included withdrawal (n=9), death (n=8) and loss to follow-up (n=16). No significant difference was found between the responders and non-responders to the survey in terms of severity of illness (mean Acute Physiology and Chronic Health Evaluation II 18 vs. 18.5), age (median 58 vs. 61), sex (male 56% vs. 71%) or ICU length of stay (mean 5.6 vs. 5.1). Table 1 presents the baseline characteristics of the patients who completed the survey.
The DTS has been used widely in the initial assessment of patients who have undergone a range of physically or psychologically traumatic event that could be related to the development of PTSD. The DTS measures all 17 primary PTSD symptoms relating to the three main symptom areas (i.e. intrusion, avoidance and hyperarousal) with specific criteria for both frequency and intensity rated on a five-point scale (i.e. for frequency: 0, 'not at all'; 1, 'once only'; 2, '2 or 3 times'; 3, '4–6 times'; 4, 'every day'; and, for severity: 0, 'not at all distressing'; 1, 'minimally distressing'; 2, 'moderately distressing'; 3, 'markedly distressing'; 4, 'extremely distressing') in relation to the past week. The maximum total score is 136. For the purposes of this study we used two threshold scores to convert the continuous scores into dichotomous categories for the analyses of the data. A score of 40 or above (sensitivity 0.69; specificity 0.95; efficiency 0.83) was used to confirm with a high degree of specificity a diagnosis of PTSD according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) [26]. A score of 27 or above (sensitivity 0.81; specificity 0.82; efficiency 0.81) was used to identify those individuals with high levels of specific post-traumatic psychopathology who may or may not meet diagnostic criteria for PTSD as set out by the DSM-IV. The efficiency of the self-report measure corresponds to the percentage correctly classified as having PTSD or as not having PTSD. Patients were asked whether they about thoughts they might die of death and their interpretation of the seriousness of the injury. Patients were also asked to report whether they had visited their general practitioner (GP) or a mental health professional complaining of psychological symptoms before their critical illness but no more formal assessment of previous psychiatric history was made. All patients with significant post-traumatic psychopathology (as measured by the DTS) were offered follow-up by a psychiatrist with a special interest in post-trauma reactions.
Analyse-it software for Microsoft Excel was used to analyse the data. Non-parametric methods were needed owing to skewed distributions and heterogeneity of variance. The Mann-Whitney U test assisted between group comparisons. The relationship between variables was assessed by means of Spearman's rank correlation coefficient and the χ2 test for associations.
Results
There was no difference in DTS scores between admission diagnosis groups (Table 2). Eleven (14%) patients endorsed the statement that they had visited either a GP or a mental health professional for psychological distress prior to their critical illness, and this group had a higher DTS score than those without a previous history (p=0.005). Forty-two patients (54%) considered themselves to have been seriously injured at the time of their critical illness, but their DTS was not higher. Twenty seven patients (35%) had had thoughts of death before or after their critical illness, but their DTS was not higher than those without such thoughts. The median DTS score for the cohort was 8 (range 0–87) with 17 patients (22%) having a DTS score higher than 27 and 9 (12%) having a DTS score higher than 40 (Tables 2, 3). Further, 11 (14%) met the full DSM-IV diagnostic criteria for PTSD [26] according to their responses on the DTS [26]. Table 3 shows the distribution of patients on the DTS and whether they met DSM IV criteria for PTSD. A breakdown of symptoms in patients with DTS scores of 27 or higher is presented in Fig. 1. All of these patients were offered follow-up by a psychiatrist, and only one patient (5%) accepted referral. For a breakdown of symptoms in patients with DTS scores of 27 or higher (see Fig. 1).
Neither total DTS or its sub-scores were correlated with sex, ICU length of stay, or APACHE II score. The median age of patients with DTS scores lower than 27 was 61.5 years, that of patients with DTS scores of 27–39 46 years, and that of patients with scores of 39 or higher 51 years [p=0.04 for low (<27) vs. high DTS]. Patients with total DTS lower than 27 and those who met the full diagnostic criteria for PTSD according to DSM-IV were younger than patients whom did not have significant PTSD-related symptoms (p=0.04 and p=0.06, respectively). In the overall cohort of patients the DTS was inversely correlated with age (p=0.003; Fig. 2). There was a direct correlation between days of mechanical ventilation and total DTS score in the overall cohort (p=0.012) but the number of days of mechanical ventilation failed to reach statistical significance in those with DTS score of 27 or higher.
The correlation between age in years and total Davidson Trauma Score for a cohort of general ICU patients 3 months after ICU discharge. Filled dots Age of individuals who reported having visited their GP or a mental health professional for psychological distress prior to their ICU admission (significant difference at p=0.005). Correlations calculated using linear regression (r=0.11, p=0.003)
Discussion
From a cohort of general ICU patients, with variable severities of illness and ICU lengths of stay, we were able to identify a number of patients with high levels of specific post-traumatic psychopathology as measured by the DTS. No significant differences were found between patients with high or low scores on the DTS in terms of sex, severity of illness severity or admission diagnosis. Interestingly, total DTS score was correlated with time on mechanical ventilation but not ICU length of stay. These results may require re-testing in larger cohorts.
According to their response on the DTS, 11 (14%) of the patients in our study met DSM-IV criteria for the diagnosis of PTSD 3 months after discharge [26]. The total DTS score was at least 27 in 22% of patients, which represents a significant level of specific post-traumatic symptoms (even when PTSD criteria are not fulfilled), and 12% scored at least 40. These findings are comparable to the majority of previous results but higher than one series [18, 19, 20, 21]. Our results suggest that large numbers of patients suffer severe and debilitating psychological symptoms after critical illness. In routine clinical practice these patients may not be identified as suffering psychological problems and therefore not offered psychological help. It could be suggested that severity of symptoms 3 months after critical illness may improve with time. However, whilst no longitudinal studies have addressed the persistence of psychological symptoms related to PTSD after critical illness, community studies have demonstrated that PTSD symptoms at 3 months tend to persist chronically without treatment [12]. The average duration of an episode of PTSD is 7 years thus non-identification or non-treatment will lead to chronic suffering.
The most important potential limitation of this study is the use of the DTS by telephone rather than as a self-report measure. The DTS has been validated across a range of traumatic events, and the authors of the DTS have conducted one study in which it was used by telephone [27] and validated against the Mini International Neuropsychiatric Interview (MINI), an internationally validated structured interview for diagnosing all major psychiatric disorders. Telephone interviews to determine post-traumatic symptoms have also been used in epidemiological studies of PTSD by prominent epidemiologists such as Breslau et al. [28]. The authors recognise that in an ideal study a sample of the cohort would have been assessed on a standardised interview conducted face to face by a mental health professional. However, the DTS was chosen rather a structured interview such as the World Health Organization Composite International Diagnostic Interview because of the latter's length; it was considered important to limit the length of interview as the patients were interviewed soon after critical illness. The use of the DTS by telephone does represent a limitation upon the interpretation of our data.
Another limitations of this study is that it is a moderately sized sample. Also, acute PTSD resolving within 3 months would not have been identified as the assessment was undertaken 3 months after injury; and only retrospective data were available on pre-existing psychological distress that was reported to their GP or mental health professionals. This could lead to an underestimate of the incidence of psychological problems if symptoms went unreported or an overestimation of the incidence related to the reporting of minor psychological problems. With a lifetime prevalence in community samples of between 1.3% and 12%, any effect would be expected to be small although the presence of pre-existing PTSD could not be categorically excluded [1, 2]. However, in keeping with the correct use of the DTS all respondents were asked to detail their symptoms in relation solely to their experience in the ICU, once again reducing the likelihood of reporting of more chronic symptoms.
The limitations are compensated for by: (a) the prospective nature of the study, (b) the identification of individuals with prolonged distress, (c) the assessment of individuals with severe injuries or illness as they are often excluded from trauma studies, and (d) the use of a reliable and well validated self-report measure of post-traumatic psychopathology (although we used it via telephone rather through self-reporting, an incompletely validated method). With regard to the latter strength the DTS is a commonly used measure in post-trauma research; it measures post-traumatic symptoms matching DSM diagnostic criteria for PTSD and has been used in many trauma populations [25]. PTSD can be diagnosed 1 month after the traumatic event and after the symptoms have been present for 1 month. A proportion of patients would be expected to improve between 1 and 3 months after the traumatic event, and therefore we chose to measure symptoms at 3 months as this would signify persistent symptoms [28]. In addition, routine follow-up often takes place at 3 months as this has been found to be a useful time to determine symptoms relating to the critical illness after ICU admission [21, 29].
The response rate of 70% 3 months after hospital discharge is high for studies of trauma survivors. The importance of high response rates has been highlighted elsewhere by Weisaeth [30]. Weisaeth has noted that the true prevalence of post-traumatic reactions is underestimated if recruitment rates are low as a study examining features of the trauma may exclude some individuals with prominent avoidance of reminders of the trauma (a core symptom of PTSD). Thus it may be that our result is an underestimate of the problem.
There has been much debate regarding the causal role of factors such as previous mental health problems in PTSD; this is less clear in the area of critical illness than in other trauma populations. Klein et al. [31] have previously shown that endorsement of the statement "visited a GP for stress" prior to the accident is a more reliable predictor than asking about their pre-trauma psychiatric history. In keeping with these findings from studies of other trauma populations [31], our study confirms that subjects reporting having visited their GP or a mental health professional for psychological distress prior to their ICU admission have higher levels of post-traumatic symptoms. The failure to find this association in other studies of medical event trauma [13, 14, 15] may be related to the greater predictive power of this question. However, having a history of previous psychological distress did not predict the cause of admission to ICU. Epidemiological studies have found children and the elderly to be at greater risk of developing post-traumatic psychopathology after traumatic events [2, 32]. Our findings suggest that the experience of critical illness was more commonly associated with the development of specific post-traumatic psychopathology in adults under 50 years old. The reasons for this are unclear and further studies are needed.
Previous studies have reported that a clinical assessment of injury severity is not predictive of future PTSD [33], but that the patient's perception of the injury is significantly related to the development of PTSD [34, 35]. All patients who took part in this study were asked about their perception of their illness or injury and also about their perception of the threat to their life, which has also been shown to be predictive of future PTSD [36]. Neither factor was found to have a significant association with post-traumatic psychopathology. These findings may be due to either a type II error, or the very high rates of severe illness and threat to life. Further research is required before either of these factors can be identified as useful predictors to identify those at risk or requiring review in an ICU setting.
What can be done to identify these patients? The identification of pre-trauma stressors [15] and the assessment of the individuals' recovery environment (for example, pain or job loss) are important [12]. Patients with these identified predictive factors and possibly those with high DTS scores at time of hospital discharge should be followed-up [9, 29]. ICU follow-up clinics should add the assessment of post-traumatic psychopathology to their previously already identified aims which include: the provision of information about their ICU care and to follow-up medical issues related to their ICU admission [29]. This may assist the adjustment process after admission and may limit the development of PTSD [19, 20]. An integral part of the ICU follow-up clinic should be liaison with a mental health professional with an interest in post-traumatic reactions who can offer the accurate diagnosis, appropriate therapeutic options and follow-up for these patients.
In conclusion, a significant number of ICU patients returning to the community develop severe psychological symptoms relating to their hospital stay. We need to identify these patients and offer appropriate treatment by developing good quality ICU follow-up services with strong links with family practice and mental health services. Further research is needed to identify risk factors for the development of PTSD in the critically ill to aid the identification of at-risk patients before hospital discharge, with longitudinal studies required to study the time course and natural history of symptoms relating to PTSD in this cohort.
References
Davidson JRT, Hughes D, Blazer DG, George LK (1991) Post-traumatic stress disorder in the community: an epidemiological study. Psychol Med 21:713–721
Kessler RC (2000) Post-traumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry 61:4–12
Alexander DA (1997) Psychological Aspects of Trauma. In: Greaves I, Porter K, Burke D (eds) Key topics in trauma. Bios, Oxford, pp 249–257
Hull AM, Alexander DA, Klein S (2002) A long-term follow-up study of the survivors of the Piper Alpha oil platform disaster. Br J Psychiatry 181:435–440
Helzer JE, Robins LN, McEvoy L (1987) Post-traumatic stress disorder in the general population. Findings of the epidemiological catchment area survey. N Engl J Med 17:1630–1634
Epstein RS (1993) Avoidant symptoms cloaking the diagnosis of PTSD in patients with severe accidental injury. J Trauma Stress 6:139–145
Shalev AY, Schreiber S, Galai T, Melmed RN (1993) Post-traumatic stress disorder following medical events. Br J Clin Psychol 32:247–253
Yu BH, Dimsdale JE (1999) Posttraumatic stress disorder in patients with burn injuries. J Burn Care Rehabil 20:426–433
Ehde DM, Patterson DR, Wiechman SA, Wilson LG (2000) Post-traumatic stress symptoms and distress 1\year after burn injury. J Burn Care Rehabil 21:105–111
McFarlane AC (2000) Ethnocultural issues. In: Nutt D, Davidson JRT, Zohar J (eds) Post-traumatic stress disorder. Diagnosis, management and treatment. Dunitz, London, pp187–198
Michaels AJ, Michaels CE, Zimmerman MA, Smith JS, Moon CH, Peterson C (1999) Posttraumatic stress disorder in injured adults: etiology by path analysis. J Trauma Injury Infect Crit Care 47:867–873
Ballenger JC, Davidson JRT, Lecrubier Y, Nutt DJ, Foa EB, Kessler RC, McFarlane AC, Shalev AY (2000) Consensus statement on post-traumatic stress disorder from the international consensus group on depression and anxiety. J Clin Psychiatry 61S: 60–66
Fauerbach JA, Lawrence JW, Munster AM, Palombo DA, Richter D (1999) Prolonged adjustment difficulties among those with acute posttrauma distress following burn injury. J Behav Med 22:359–378
Fauerbach JA, Lawrence JW, Schmidt CW, Munster AM, Costa PT (2000) Personality predictors of injury-related posttraumatic stress disorder. J Nerv Ment Dis 188:510–517
Schnyder U, Moergeli H, Klaghofer R, Buddeberg C (2001) Incidence and prediction of posttraumatic stress disorder symptoms in severely injured accident victims. Am J Psychiatry 158:594–599
Shalev AY, Peri T, Canetti L, Schreiber S (1996) Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 153:219–225
Holbrook TL, Hoyt DB, Stein MB, Sieber WJ (2001) Perceived threat to life predicts posttraumatic stress disorder after major trauma: risk factors and functional outcome. J Trauma Injury Infect Crit Care 51:287–292
Stoll C, Schelling G, Goetz AE, Kilger E, Bayer A, Kapfhammer HP, Rothenhausler HB, Kreuzer E, Reichart B, Peter K (2000) Health-related quality of life and post-traumatic stress disorder in patients after cardiac surgery and intensive care treatment. J Thorac Cardiovasc Surg 120:505–512
Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Meier M, Preuss U, Bullinger M, Schuffel W, Peter K (1998) Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 26:651–659
Scragg P, Jones A, Fauvel N (2001) Psychological problems following ICU treatment. Anaesthesia 56:9–14
Eddleston JM, White P, Guthrie E (2000) Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med 28:2293–2299
Ehde DM, Patterson DR, Wiechman SA, Wilson LG (1999) Post-traumatic stress symptoms and distress following acute burn injury. Burns 25:587–592
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67:361–370
Marmer CR, Weiss DS (1997) The impact of event scale–revised. In: Wilson JP, Keane TM (eds) Assessing psychological trauma and PTSD. Guilford, New York, pp 399–411
Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, Hertzberg M, Mellman T, Beckham JC, Smith RD, Davison RM, Katz R, Feldman ME (1997) Assessment of a new self-report scale for PTSD. Psychol Med 27:153–160
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington
Davidson JRT, Tharwani HM, Connor KM (2002) Davidson Trauma Scale (DTS): normative scores in the general population and effect sizes in placebo-controlled SSRI trials. Depress Anxiety 15:75–78
Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P (1998) Trauma and posttraumatic stress disorder in the community. The Detroit Area Survey of Trauma. Arch Gen Psychiatry 55:626–632
Griffiths RD, Jones C (2002) Intensive care aftercare. Butterworth-Heineman, Oxford
Weisaeth L (1989) Importance of high response rates in traumatic stress research. Acta Psychiatr Scand 80:131–137
Klein S, Alexander DA, Hutchinson JD, Simpson JA, Simpson JM, Bell JS (2002) The Aberdeen Trauma Screening Index: an instrument to predict post-accident psychopathology. Psychol Med 32:863–871
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (1995) Post-traumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry 52:1048–1060
Green BL (1994) Psychosocial research in traumatic stress. J Trauma Stress 7:341–362
Jeavons S (2000) Predicting who suffers psychological trauma in the first year after a road accident. Behav Res Ther 38:499–508
Schnyder U, Morgeli H, Nigg C, Klaghofer R, Renner N, Trentz O, Buddenberg C (2000) Early psychological reactions to life-threatening injuries. Crit Care Med 28:86–92
Alexander DA (1999) Human reactions to trauma: their features and management. In: Greaves I, Porter K (eds) Pre-hospital medicine: the principles and practice of immediate care, Arnold, London
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuthbertson, B.H., Hull, A., Strachan, M. et al. Post-traumatic stress disorder after critical illness requiring general intensive care. Intensive Care Med 30, 450–455 (2004). https://doi.org/10.1007/s00134-003-2004-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2004-8