Abstract
Objective
To study the prognostic impact of the appropriateness of initial antimicrobial therapy in patients suffering from ventilator-associated pneumonia (VAP).
Design and setting
Observational cohort from January 1994 to December 2001 in one intensive care unit (ICU) from an university-affiliated, urban teaching hospital.
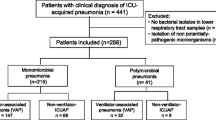
Patients
All 132 consecutive patients exhibiting bacteriologically documented VAP during ICU stay.
Measurements and results
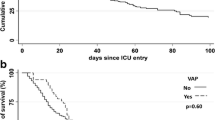
Initial antimicrobial treatment was deemed appropriate when the period from initial VAP diagnosis and subsequent administration of antibiotics was within 24 h and all causative pathogens were in vitro susceptible to at least one of the antibiotics of the regimen. Such a treatment was present in 106 episodes. Fifty-eight patients died. In bivariate analysis an appropriate initial antimicrobial therapy was associated with a significantly lower mortality rate (40% vs. 62%). In multivariate analysis the three independent factors present upon VAP onset and associated with death were pulmonary involvement of more than a single lobe on chest radiograph, platelet count less than 150,000/mm3, and Simplified Acute Physiology Score II higher than 37. Appropriate antimicrobial therapy was associated with a nonsignificant trend toward a lower mortality.
Conclusions
In our cohort the mortality rate was lower in patients suffering from VAP when the initial antimicrobial therapy was appropriate. However, such a factor did not appear as an independent prognostic factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ventilator-associated pneumonia (VAP) remains a frequent and severe infection in intensive care units (ICU). Although determination of mortality attributable to VAP is challenging, it remains apparent throughout the literature that certain factors are linked with poor prognosis [1, 2, 3, 4, 5, 6, 7]. There are factors associated with the patient, such as old age, underlying disease, immunosuppression, and nonsurgical cause of ICU admission; with the VAP itself, such as bacteremia, shock, prior antimicrobial therapy, associated organ failures, high Simplified Acute Physiology Score (SAPS) II, late-onset pneumonia, and high-risk pathogens; and with the medical management, such as the appropriateness and the delay in initiating antimicrobial therapy [4, 5, 6, 7]. However, despite numerous studies some controversies continue to exist about the genuine prognostic impact of the initial antimicrobial therapy [1].
The goal of our study was therefore to use multivariate analysis of prognostic factors reported in the literature and additional biological and radiographic findings to identify factors associated with prognosis of VAP encountered in our ICU and to determine the prognostic impact of our initial antibiotics choices.
Patients and methods
Between 1994 and 2001 all 132 consecutive patients exhibiting bacterologically documented VAP were included in an observational cohort study (95 men, 37 women; mean age 64.6±13.6 years). VAP was defined as new and/or progressive chest roentgenographic infiltrates occurring during or after a mechanical ventilation period of more than 48 h after ICU admission in conjunction with at least two of the following criteria: purulent respiratory secretions, temperature above 38.5°C or below 35°C, leukocyte count above 10,000/mm3 or below 1,500/mm3. Only patients exhibiting bacteriologically documented VAP were studied. Establishment of causal diagnosis required isolation of bacteria in significant quantity from a sample of lower respiratory tract secretions (endotracheal aspiration at least 106 cfu/ml, protected brush catheter at least 103 cfu/ml or bronchoalveolar lavage at least 104 cfu/ml) or isolation of a definitive pathogen from a blood or pleural fluid culture. In each episode all significant isolates and their antimicrobial susceptibility were identified by standard techniques.
On ICU admission we prospectively collected demographic characteristics, indication(s) of ICU admission, underlying clinical conditions, severity of illness, and vital sign abnormalities. The underlying diseases were classified with criteria proposed by McCabe and Jackson [8]. When VAP occurred, its time of onset from ICU admission, prior antimicrobial therapy within 1 month before VAP, chest radiographic involvement, presence of shock, SAPS II, usual biochemical, and hematological tests were recorded. Shock was defined by usual criteria [9]. Initial antimicrobial treatment was deemed appropriate when the period from the initial VAP diagnosis and the subsequent administration of antibiotics was 24 h or less, and when all causative pathogens were in vitro susceptible to at least one of the antibiotics of the regimen [5]. During the ICU stay complications were recorded. We distinguished those related to pneumonia, such as sepsis-related complications (i.e., acute respiratory distress syndrome or multiple-organ failure) or recurrences or relapses, and those not directly related to VAP such as ICU-related complications (i.e., gastrointestinal bleeding) or complications attributed to underlying medical conditions. Patient mortality was evaluated at ICU discharge.
Prognosis was analyzed retrospectively according to two groups: patients who died during their ICU stay (n=58) and those who survived (n=74). Categorical variables were compared using the χ2 test or Fisher's exact test when the χ2 test was not appropriate. Continuous variables were compared using Student's t test. Differences between groups were considered to be significant for variables yielding a p value of 0.05 or less. Some continuous variables were categorized into classes by selecting the best cutoffs (receiver operating characteristic analysis, maximization of the χ2). All variables attaining an α value of 0.05 were included in a multiple logistic regression analysis model with a stepwise selection of variables. All analyses were performed using the SAS Software version 8.2 (SAS Institute, Cary, N.C., USA).
Results
The main indications for ICU admission were acute respiratory failure (81%) and infectious diseases (42%); from their underlying condition death would have been expected in maximally 5 years in 82 of the patients. The mean SAPS II on ICU admission was 43.1±12.7. The median period between ICU admission and VAP onset was 13.2±10.4 days. During the 1 month prior to the occurrence of VAP 108 patients had received prior antibiotics. Upon VAP onset the mean SAPS II value was 37.9±10.9. Pulmonary involvement was in more than a single lobe in 58 patients. Fifteen patients exhibited shock. Mean PaO2/FIO2, creatinine, and platelet count values were 201±86 mmHg, 14.4±11.6 mg/l, and 235±119 103/mm3, respectively. Among the 162 causative pathogens identified, the principal ones were Streptococcus pneumoniae (n=8), Haemophilus influenzae (n=8), Staphylococcus aureus (n=30) with 11 methicillin-resistant strains, Enterobacteriaceae (n=32), Pseudomonas aeruginosa (n=57), Stenotrophomonas maltophilia (n=11), and Acinetobacter baumannii (n=9).
Initial antimicrobial therapy for VAP was instituted empirically in 126 patients and in the remaining six patients was based on the results of culture from lower respiratory tract secretions. Antibiotics empirically instituted are reported in Table 1. Initial empirical therapy was appropriate in 106 episodes (84%) and inappropriate in 20 episodes. Inappropriateness was due either to a too late initiation (n=11) or to a resistance of all causative pathogens to the antibiotic(s) (n=9). All treatments (n=6) based on results from culture of respiratory specimens were considered inappropriate. Despite in vitro susceptibility of causative pathogen(s), the delayed initiation explained the inappropriateness. In summary, initial antimicrobial therapy was considered inappropriate in 26 episodes.
When initial therapy was inappropriate, the occurrence of complications linked to underlying conditions was more frequent (13/26 vs. 20/106; p=0.001). However, the occurrence of sepsis-related complications (10/26 vs. 45/106) and ICU-related complications (10/26 vs. 36/106) was not correlated with the appropriateness of initial therapy. Significant factors associated with death in bivariate and multivariate analyses are reported in Table 2. None of variables collected on ICU admission or during ICU stay before VAP occurrence was significantly associated with prognosis. Among variables collected upon VAP onset three appeared as independent prognostic factor: chest radiographical involvement in more than 1 lobe, platelet count less than 150,000/mm3, and SAPS II higher than 37. Appropriate initial therapy appeared associated with a significant decreased mortality rate (42/106 vs. 16/26; p=0.04) in bivariate analysis. According to multivariate analysis, this factor was associated with a trend toward a lower mortality rate (adjusted odds ratio =0.6) but did not appear as an independent factor (p=0.35).
Discussion
In our cohort, although an appropriate initial antimicrobial treatment was associated with a significant lower mortality rate, it did not appear as an independent prognostic factor. The independent factors, all identified upon VAP onset, were chest radiographic involvement of more than a single 1 lobe, SAPS II higher than 37, and platelet count less than 150,000/mm3. The prognostic value of SAPS II determined upon VAP onset has been reported previously [10]. Froon et al. [10] showed that SAPS II upon ICU admission does not differ significantly between survivors and nonsurvivors at 10 days, whereas SAPS II determined at the onset of VAP was greater in survivors than non-survivors, though without reaching significance. Our results were quite similar since the mean SAPS II values upon ICU admission did not differ in survivors and non-survivors, but SAPS II upon onset of VAP was significantly greater in nonsurvivors than in survivors. The prognostic importance of chest radiographic involvement may seem more surprising. This parameter does not appear to have been considered of value throughout the literature. We have, however, previously reported the prognostic importance of initial lung involvement in severe community-acquired pneumonia [11]. It therefore seems logical to consider that radiographic findings may be of prognostic importance in patients developing VAP. Finally, the prognostic significance of platelet count does not seem to ever have been considered even though two recent studies have reported the overall prognostic importance in the ICU of thrombocytopenia defined as a platelet count less than 150,000/mm3. Vanderschueren et al. [12] found that the existence of thrombocytopenia at any given moment of the ICU stay was an independent prognostic factor. Likewise, Akca et al. [13] found that thrombocytopenia on day 14 of ICU stay was a factor of poor outcome. In our cohort VAP occurred in 13.2±10.4 days following ICU admission. The fact that a platelet count lower than 150,000/mm3 is of prognostic importance is thus in accordance with these studies.
The prognostic importance of appropriate initial antimicrobial therapy both in timing and efficacy on the causal micro-organism(s) has been underlined in many studies [4, 5, 6, 7]. In our study appropriate antimicrobial therapy was defined identically to Iregui et al. [5]. Although bivariate analysis yielded a significantly greater mortality with inappropriate than appropriate therapy (62% vs. 40%, p=0.4), we found no independent correlation between prognosis and appropriateness of initial antimicrobial therapy. These results may be explained by the small number of patients treated with an inappropriate initial antimicrobial therapy (20%). This incidence of inappropriate therapy is markedly lower than those reported in studies showing a prognostic importance of initial treatment. The reported incidence ranges from 75% to 31% [4, 5, 6, 7]. However, there may be other explanations since some authors report no negative effect on prognosis in the presence of high incidence of inappropriateness. Bercault and Boulain [14] did not observe a negative effect even with a 32% incidence of inappropriate therapy.
In summary, in our cohort the mortality rate was lower in patients suffering from VAP when the initial antimicrobial therapy was appropriate. However, such a factor did not appear as an independent prognostic factor.
References
Chastre J, Fagon JY. Ventilator-associated pneumonia (2002) Am J Respir Crit Care Med 165:867–903
Kollef MH, Silver P, Murphy DM, Trovillion E (1995) The effect of late-onset ventilator-associated pneumonia in determining patient mortality. Chest 108:1655–1662
Ibrahim EH, Tracy L, Hill C, Fraser VJ, Kollef MH (2001) The occurrence of ventilator-associated pneumonia in a community hospital: risk factors and clinical outcomes. Chest 120:555–561
Moine P, Timsit JF, de Lassence A, Troche G, Fosse JP, Alberti C, Cohen Y, The OUTCOMEREA study group (2002) Mortality associated with late-onset pneumonia in the intensive care unit: results of a multi-center cohort study. Intensive Care Med 28:154–163
Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH (2002) Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest 122:262–268
Kollef MH, Ward S (1998) The influence of mini-BAL cultures on patient outcomes: implications for the antibiotic management of ventilator-associated pneumonia. Chest 113:412–420
Luna CM, Vujacich P, Niederman MS, Vay C, Gherardi C, Matera J, Jolly EC (1997) Impact of BAL data on the therapy and outcome of ventilator-associated pneumonia. Chest 111:676–685
McCabe WR, Jackson CG (1962) Gram-negative bacteremia: etiology and ecology. Arch Intern Med 110:847–855
Bone RC, Fischer CJ, Clemmer TP, Slotman GJ, Metz CA, Balk RA (1989) The methylprednisolone severe sepsis study group. Sepsis syndrome: a valid clinical entity. Crit Care Med 17:389–393
Froon AHM, Bonten MJM, Gaillard CA, Greve JW, Dentener MA, de Leeuw PW, Drent M, Stobberingh EE, Buurman WA (1998) Prediction of clinical severity and outcome of ventilator-associated pneumonia. Am J Respir Crit Care Med 158:1026–1031
Leroy O, Devos P, Guery B, Georges H, Vandenbussche C, Coffinier C, Thevenin D, Beaucaire G (1999) Simplified prediction rule for prognosis of patients with severe community-acquired pneumonia in ICUs. Chest 116:157–165
Vanderschueren S, De Weerdt A, Malbrain M, Vankersschaever D, Frans E, Wilmer A, Bobbaers H (2000) Thrombocytopenia and prognosis in intensive care. Crit Care Med 28:1871–1876
Akca S, Haji-Michael P, de Mendonça A, Suter P, Levi M, Vincent JL (2002) Time course of platelet counts in critically ill patients. Crit Care Med 30:753–756
Bercault N, Boulain T (2001) Mortality rate attributable to ventilator-associated nosocomial pneumonia in an adult intensive care unit: a prospective case-control study. Crit Care Med 29:2303–2309
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leroy, O., Meybeck, A., d'Escrivan, T. et al. Impact of adequacy of initial antimicrobial therapy on the prognosis of patients with ventilator-associated pneumonia. Intensive Care Med 29, 2170–2173 (2003). https://doi.org/10.1007/s00134-003-1990-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1990-x