Abstract
Objective
Brain-damaged patients may develop hyponatremia and natriuresis. Clinical evidence of digoxin antibody effect on natriuresis we found in an 11-year-old boy who developed excessive natriuresis and hyponatremia after brain tumor excision. To better understand the mechanisms involved in these clinical disturbances we used an experimental model of rats subjected to intracerebroventricular (ICV) hemorrhage. The participation of serum ouabainlike activity, possibly a natriuretic compound, and the effects of a specific blocker, digoxin antibody, were studied.
Methods
The experimental study was performed in four groups of ICV infused Wistar rats: venous autologous blood infused, blood preceded by digoxin antibody, CSF-like solution, and a control group with no cannulation and no infusions. The following parameters were analyzed before and after ICV infusions: weight, urinary volume, and natriuresis. Ouabainlike activity was measured by proportional serum inhibitory activity on normal rat renal medullary Na-K-ATPase activity.
Results
ICV blood but not CSF-like infusion increased urinary volume, natriuresis, and serum ouabainlike activity without weight gain. Natriuresis was positively correlated with serum ouabain activity in ICV blood and blood plus antibody rats. Digoxin antibody restored urinary volume, natriuresis, and ouabainlike activity.
Conclusions
These data provide evidence of ouabainlike activity involvement in natriuresis and urinary volume changes that occur in cerebral hemorrhage. A possible therapeutic action of digoxin antibody is proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The central nervous system is involved in salt regulation by neurohumoral mechanisms, and therefore cerebral diseases can cause sodium disorders. It is estimated that approx. 30% of patients with cerebral injury, especially subarachnoid hemorrhage, admitted to intensive care units develop hyponatremia by distinct pathophysiological mechanisms [1, 2]. The syndrome of inappropriate antidiuretic hormone secretion is one of these mechanisms. In this situation fluid retention and extracellular volume expansion [3] occur. Water restriction is the therapeutic approach for this syndrome [4]. The cerebral salt wasting (CSW) syndrome characterized by hyponatremia and excessive natriuresis, with an unknown underlying mechanism, was described as early as the 1950s by Peters et al. [5] and by Cort [6]. Overproduction of atrial [7] or brain [8] natriuretic peptides and depressed mineralocorticoid activity [9] have also been postulated as involved mechanisms. The usual therapeutic approach for hyponatremia with natriuresis in humans consists of intravenous sodium replacement, which depending on the infusion rate can be harmful because of the pontine myelinosis risk [10].
Another natriuretic substance, probably originating in the central nervous system, was initially described as the result of intravascular volume expansion. This acts as an Na-K-ATPase inhibitor [11, 12] and may participate in CSW. In human cerebral damage and in intracerebroventricular (ICV) manipulations in animal models an overproduction of this natriuretic substance by local stimulation can occur, as demonstrated in the following observations. Wijdicks et al. [13] showed that an endogenous ouabainlike compound (OLC) was increased in the plasma of 18 out of 25 patients with subarachnoid hemorrhage in whom hyponatremia with excessive natriuresis was present. Nelson et al. [14] observed that subarachnoid hemorrhage in monkeys caused hyponatremia and natriuresis with normal antidiuretic hormone concentration and proposed a cerebral natriuretic factor as the mediator. Huang et al. [15] reported the role of an OLC as the mediator of excessive natriuresis after ICV administration of hypertonic saline. Furthermore, Yamada et al. [16] blocked these effects employing ICV digoxin antibody in rats. Data from our previous studies show high OLC in salt-sensitive hypertensive humans [17].
Based on the fact that an endogenous natriuretic substance with inhibitory activity on Na-K-ATPase, and therefore with ouabain activity, can be overproduced after brain injury, the possibility of blocking this substance with digoxin antibody was hypothesized. A clinical case addressing this hypothesis is described. An 11-year-old white boy who developed hyponatremia with natriuresis after brain surgery is reported, and the effect of polyclonal digoxin antibody (Digibind), originally synthesized for human use in digitalis intoxication treatment [18], was evaluated.
The patient was admitted to the hospital with 10 days' history of headache, weight loss, and drowsiness. Computed tomography disclosed a large tumor in the left anterior encephalic area expanded to hypothalamus. At admission his body weight was 31.5 kg, blood pressure 126/76 mmHg, and heart rate 94 bpm. Laboratory tests showed hematocrit 40%, white blood cells 13,000/mm3, creatinine 0.5 mg/dl, serum Na 139 mEq/l, K 4 mEq/l, and glucose 123 mg/dl. On the first postoperative day of tumor excision, hyponatremia developed. At this moment water restriction was introduced; however, there was no clinical improvement. An intravenous and nasoenteric sodium replacement was started and maintained for 28 days. Phenytoin at 100 mg twice daily was given during the entire period of hospitalization. Decreasing doses of dexametasone (days 1–21) was given. On the 22nd day a 6-day fludrocortisone trial (0.2 mg/day) was started, but natriuresis did not improve. Informed consent was obtained from patient's family and the Scientific and Ethics Committee of Albert Einstein Hospital, in accordance with the ethical standards of the 1964 Declaration of Helsinki, to allow intravenous infusion of digoxin antibody (8 mg in 200 ml saline/30 min according to the manufacturer's instructions). As Fig. 1A shows, this led to a decrease in serum sodium and an increase in sodium replacement. Administration of digoxin antibody (28th day) corrected hyponatremia and decreased sodium replacement. Figure 1B shows increased urinary volume and volume infusion (both corrected with digoxin antibody) and normal blood pressure. Figure 1C shows the digoxin antibody acute effect, reducing natriuresis during a 144 h observation period. Plasma renin activity, aldosterone, cortisol, and antidiuretic hormone levels were normal. Plasma digoxin on days 26 and 28 were, respectively, 0.30 and 0.34 ng/ml (RIA-Abbot). High urine osmolality and density were observed.
Digoxin antibody (DA) effect in the patient. A Serum sodium (filled circles) and sodium replacement (open circles). B Urinary volume (open circles), volume infusion (filled circles), and mean blood pressure (filled squares). C DA acute effect on urinary sodium excretion: before (filled squares) and after (open squares). FLU Fludrocortisone. A, B star p<0.05 vs. −3 and 36. C star p<0.05 vs. after. Each point represents 3 days in A and B (mean ±SEM)
After the results obtained in this patient an experimental study was undertaken to determine whether OLC is involved in natriuretic changes in awake animals subjected to ICV hemorrhage and also to evaluate the effect of ICV infusion of digoxin antibody as a preventive procedure for these changes.
Methods
Animals
Male Wistar rats weighing 250–350 g were studied. Blood urea nitrogen (<50 mg/dl, normal value) was measured to estimate renal function. Ad libitum diet containing 0.6 Na g% and tap water was given. The experimental protocol was approved by the animal studies ethics committee of Sao Paulo University Medical School, in accordance with the "Principles of laboratory animal care," (NIH publication no. 86-23, revised in 1985) [19].
Surgical implant of the cannula
A skin incision under anesthesia with thiopental sodium (50 mg/kg intraperitoneally) was performed and a 1-mm hole was drilled through the right parietal bone 0.8 mm posterior and 1.5 mm lateral to bregma suture. A stainless steel cannula was introduced stereotaxically down to 1 mm above the right lateral ventricle and fixed with cement to the skull. Brain histology was performed to confirm the site of ICV infusion.
Animal groups and ICV Infusions
The following groups of animals were studied:
-
Group 1: ICV infused with autologous venous blood previously collected from the animal tail through an infusion pump at 50 µl/12 min (n=6)
-
Group 2: ICV infused with Fab fragments of digoxin antibody (Digibind, 10 mg/ml) just before blood infusion at 10 µl/2.4 min (n=6)
-
Group 3: ICV infused with cerebrospinal fluid (CSF)-like solution containing: 140 mEq/l Na+, 3 mEq/l K+, 1.3 mEq/l Ca2+, 1 mEq/l Mg2+, 25 mEq/l HCO3, and 60 mg/dl glucose, at 50 µl/12 min (n=6)
-
Group 4: controls anesthetized and sham-operated on the same day of cannula introduction and ICV infusions (n=5).
Laboratory measurements
One week after cannula implantation the animals were placed in metabolic cages with an adaptation period of 3 days and subsequently maintained for 11 days. ICV infusions were performed on the 4th day under anesthesia (thiopental sodium 50 mg/kg intraperitoneally) through a needle 1.5 mm longer than the cannula to allow entry in the right lateral ventricle. Collections performed on the day after infusions (5th day) were discarded due to anesthesia influence. Daily chow and water ingestion, body weight, and urinary volume were measured. Urinary sodium concentration was measured with a flame photometer (CELM FC-280, Brazil), and urinary sodium excretion was determined by calculating sodium content in 1-day urine volume. On the last day blood samples were collected by cardiac puncture under anesthesia in order to measure the effects on Na-K-ATPase activity in renal outer medulla homogenate of normal rats. The [32P]ATP hydrolysis method was used to determine enzyme activity [20].
Na-K-ATPase assay
Normal rats under anesthesia were nephrectomized. Kidneys were sliced longitudinally, and the outer medulla was separated and homogenized for Na-K-ATPase assay. Four solutions were prepared to avoid influence of any other enzyme activity: (a) 20 mM KCl, (b) 20 mM KCl plus 100 µl ouabain (0.018 g/ml; Sigma), (c) no KCl plus 100 µl ouabain, and (d) 20 mM KCl plus 100 µl filtered animal serum. The experimental procedure was performed as follows: 400 µl of each solution was added to 100 µl outer medulla homogenate (in duplicate) and to 100 µl homogenate solvent. All tubes were incubated at 37°C for 30 min. Subsequently 100 µl 30% trichloroacetic acid and 900 µl 10% activated charcoal were added to the tubes. All tubes were centrifuged at 10,000 rpm for 6 min. At the end 500 µl of the supernatant was added to 5 ml aquasol in counting vials, and the radioactivity was determined in liquid scintillation analyzer (Packard Tri-Carb, 1600 TR, USA) [21].
Serum inhibitory activity on normal rat renal Na-K-ATPase activity
To estimate the effects of animal serum on Na-K-ATPase activity we compared maximal enzymatic activity (solution A) with the difference between solutions D and C. Inhibition or stimulation of the enzyme was calculated.
Statistical analysis
Animal data were analyzed by paired t test. Analysis of variance was used to compare independent groups. Correlations were measured by Spearman's test. Human case report data were analyzed longitudinally by analysis of variance. The level of p<0.05 was assumed to reject the null hypothesis and declare results statistically significant. Results are expressed as mean ±SEM.
Results
Body weight
Body weight was measured for 11 days before and after ICV infusions. Mean ±SEM of 4 days before (B) and 6 days after (A) infusions, and differences (Δ=A−B) were calculated:
-
Group 1, ICV blood: before 333±15, after 336±15, difference 2±3
-
Group 2, ICV blood plus antibody: before 335±6, after 337±11, difference 1±7
-
Group 3, CSF-like: before 317±10, after 323±10, difference 6±6
-
Group 4, control: before 300±15, after 320±17, difference=20±3
Only control rats presented increased body weight (before vs. after p<0.05) and the increase was higher than that in the other three groups (p<0.05).
Ingested sodium and water
Only control rats presented higher sodium ingestion, from 0.82±0.05 to 0.94±0.04 mEq Na/day (before vs. after, p<0.05). None of the groups presented water ingestion change.
Urinary sodium excretion (mEqNa/100 g body weight/day) and urinary volume (ml/100 g body weight/day)
Table 1 shows urinary volume and sodium excretion and the difference before and after ICV infusions. Only ICV blood rats increased diuresis and natriuresis (before vs. after, p<0.05), and the increase was higher than in blood plus antibody and control rats (p<0.05).
Serum inhibitory activity on Na-K-ATPase activity
The proportional inhibition (positive value) or stimulation (negative value) of rat serum on Na-K-ATPase activity of the outer medulla of normal rats is shown in Table 1. Serum of ICV blood animals showed an inhibition on Na-K-ATPase activity of +19±15%. Digoxin antibody reversed the inhibitory effect of serum on Na-K-ATPase activity in ICV plus antibody animals with a stimulation of −5±22%. Serum of CSF group animals showed a stimulation of Na-K-ATPase activity of −72±7%. Control animals showed a stimulatory activity of Na-K-ATPase activity of −19±3%. A significant difference between ICV blood and CSF-like rats was observed (p<0.05).
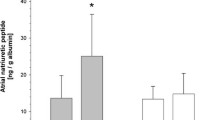
Correlation between maximal proportional increase in urinary sodium excretion and inhibitory activity of serum on Na-K-ATPase activity
Figure 2 shows a positive correlation between maximal proportional increase in urinary sodium excretion (Δmax% UNaV) and inhibitory activity of serum on Na-K-ATPase activity (IA %) in ICV blood and blood plus antibody groups, with r=0.60 and p<0.05. ICV blood rats showed higher maximal proportional increase in natriuresis, which was correlated with IA %. On the other hand, rats that received digoxin antibody presented lower maximal proportional increase in natriuresis and IA %.
Discussion
An endogenous natriuretic substance with inhibitory activity on Na-K-ATPase, an ouabain-like substance, could be overproduced after brain damage, inducing marked natriuresis. Therefore we hypothesized that blockade of this substance by digoxin antibody would have therapeutic effects on the natriuresis and diuresis by brain injury.
Results obtained in this study confirm this hypothesis. ICV blood rats showed high urinary volume, increased sodium excretion, and Na-K-ATPase inhibition. ICV digoxin antibody reversed these changes in ICV blood infused animals. The positive correlation between proportional increase in sodium excretion and NA-K-ATPase inhibition in ICV blood and ICV plus digoxin antibody rats corroborated these results.
Data in the literature show enhanced sodium excretion in animal models and in patients with subarachnoid hemorrhage [14, 22, 23]. Okuchi et al. [22] speculated that the natriuresis in human cerebral hemorrhage results from renal tubules Na-K-ATPase inhibition with a hypothalamic OLC rather than an atrial natriuretic factor, vasopressin, renin, or aldosterone action. Three alternative mechanisms may explain natriuresis after ICV hemorrhage. First, enhanced sodium ingestion may lead to increased sodium excretion. Brensilver et al. [24] reported a linear relationship between sodium ingestion and excretion. ICV blood rats presented an increased diuresis and natriuresis without a correspondent increase in sodium ingestion or body weight. Second, an elevation in blood pressure increased urinary volume and sodium excretion. Ulfendahl et al. [25] rejected this possibility because in their experiments animals presented increased natriuresis with high ICV sodium concentration and maintenance of blood pressure at 100 mmHg. Third, natriuresis could depend on the nature of ICV infused fluid. Our results demonstrate that blood but not CSF-like solution induces natriuresis through Na-K-ATPase activity inhibition.
As a final evidence, the patient observations of OLC effect on natriuresis and its prevention with digoxin antibody are reported. Water restriction on the first postoperative day was ineffective. Increased urinary volume, hyponatremia, and normal blood pressure suggested a volume depleting syndrome, such as the CSW. Aggressive replacement of sodium losses, the cornerstone for the treatment of CSW, was performed. However, this therapy may be harmful if prolonged. Fludrocortisone administration (days 21–28) did not improve the hyponatremia. Sakarcan and Bocchini [26] successfully treated a child with tuberculosis meningitis and hyponatremia by this regimen. Digoxin antibody, used for digitalis intoxication treatment, was tried based on its cross-reactivity with an endogenous hormone in a patient, not using digitalis, with two high serum digoxin measurements [17]. As a result of this new therapeutic approach urinary sodium excretion decreased, and sodium replacement reduced and serum sodium improved. To our knowledge, this was the first time that digoxin antibody was used for this purpose in human. The mechanism by which venous or ICV infusion of digoxin antibody reduced natriuresis is unknown. Renal or even hypothalamic (the blood-brain barrier could be ruptured) action on the endogenous ouabain by digoxin antibody may explain these beneficial effects.
Conclusions
We can summarize these findings as follows: (a) Animal studies demonstrated that ICV hemorrhage increases diuresis and natriuresis, which was prevented by digoxin antibody. (b) Patient data about hyponatremia treatment illustrate a possible participation of increased serum ouabain activity and its prevention with digoxin antibody, together with mineralocorticoid and sodium supplementation.
References
Harrigan MR (2001) Cerebral salt wasting syndrome. Crit Care Clin 17:125–138
Palmer BF (2000) Hyponatremia in a neurosurgical patient: syndrome of inappropriate antidiuretic hormone secretion versus cerebral salt wasting. Nephrol Dial Transplant 15:262–268
Schwartz WB, Bennett W, Curelop S, Bartter FC (1957) A syndrome of renal salt loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med 13:529–542
Miller M (2001) Syndromes of excess antidiuretic hormone release. Crit Care Clin 17:11–23
Peters JP, Welt LG, Sims EAH, Orloff J, Needham J (1950) Salt-wasting syndrome associated with cerebral disease. Trans Assoc Am Physicians 63:57–64
Cort JH (1954) Cerebral salt wasting. Lancet I:752–754
Narotam PK, Kemp M, Buck R, Gouws E, Dellen JR van, Bholla KD (1994) Hyponatremic natriuretic syndrome in tuberculous meningitis: the probable role of atrial natriuretic peptide. Neurosurgery 34:982–988
Berendes E, Walter M, Cullen P, Prien T, Van Aken H, Schulte M, van Wild K, Scherer R (1997) Secretion of brain natriuretic peptide in patients with aneurysmal subarachnoid haemorrhage. Lancet 349:245–249
Ichikawa SE, Saito T, Kaneko K, Okada K, Kuzuya T (1987) Hyponatremia responsive fludrocortisone acetate in elderly patients after head injury. Ann Intern Med 106:187–190
Soupart A, Decaux G (1996) Therapeutic recommendations for management of severe hyponatremia: current concepts on pathogenesis and prevention of neurologic complications. Clin Nephrol 46:149–169
Wardener HE De, Mills IH, Clapham WF, Hayter CJ (1961) Studies on the efferent mechanism of the sodium diuresis which follows the administration of intravenous saline in the dog. Clin Sci (Colch) 21:249–258
Gruber KA, Whitaker JM, Buckalew VM Jr (1980) Endogenous digitalis-like substance in plasma of volume-expanded dogs. Nature 287:743–745
Wijdicks EFM, Vermeulen M, van Brummelen P (1987) Digoxin-like immunoreactive substance in patients with aneurysmal subarachnoid hemorrhage. BMJ 294:729–732
Nelson PB, Seif S, GutaL J, Robinson AG (1984) Hyponatremia and natriuresis following subarachnoid hemorrhage in a monkey model. J Neurosurg 60:233–237
Huang BS, Leenen FHH (1992) Brain ouabain-like activity and the sympathoexitatory and pressor effects of central sodium in rats. Circ Res 71:1059–1066
Yamada K, Goto A, Nagoshi H, Hui C, Omata M (1994) Role of brain ouabain like compound in central nervous system-mediated natriuresis in rats. Hypertension 23:1027–1031
Dichtchekenian V, Gisiger S, Quental I, Santos SR, Marcondes M, Heimann JC (1992) Higher salt consumption, digoxin-like factor, and nifedipine response are associated with salt sensitivity in essential hypertension. Am J Hypertens 5:707–712
Boucher BA, Lalonde RL (1986) Digoxin-specific antibody fragments for the treatment of digoxin intoxication. Clin Pharm 5:826–827
Leader RW and Stark D (1987) The importance of animal in biomedical research. Perspect Biol Med 30:470–485
Araujo M, Helou CMB, Seguro AC (1998) Renal potassium handling in aging rats. Kidney Blood Press Res 21:425–431
Woolfson RG, Poston L, de Wardener HE (1994) Dioxin-like inhibitors of active sodium transport and blood pressure: the current status. Kidney Int 46:297–309
Okuchi K, Fujioka M, Fujikawa A, Nishimura A, Konobu T, Miyamoto S, Sakaki T (1996) Rapid natriuresis and preventive hypervolemia for symptomatic vasospasm after subarachnoid hemorrhage. Acta Neurochir (Wien) 138:951–957
Jandhyala BS, Ansari AF (1986) Elevation of sodium levels in the cerebral ventricles of anesthetized dogs triggers the release of an inhibitor of ouabain-sensitive sodium, potassium ATPase into the circulation. Clin Sci (Colch) 70:103–110
Brensilver JM, Daniels FH, Lefavour GS, Malseptic RM, Lorch J, Ponte ML, Cortell S (1985) Effect of variations in dietary sodium intake on sodium excretion in mature rats. Kidney Int 27:497–502
Ulfendahl HR, Ahlsson A, Hansell P, Höglund U, Jacobsson E, Lee SL, Sjöquist M, Isaksson B (1989) Studies on the mechanisms underlying CNS-induced natriuresis. Acta Physiol Scand 136:75–78
Sakarcan A, Bocchini J Jr (1998) The role of fludrocortisone in a child with cerebral salt wasting. Pediatr Nephrol 12:769–771
Acknowledgements
The authors thank Prof. César Timo Iaria, Dr. Antonio C. Seguro, Dr. Joel C. Heimann, and Dr. Luis Yu, Sao Paulo University, School of Medicine; the Hospital Israelita Albert Einstein that provided the Digibind and the physicians Hallim Feres Jr. and Vae Dichtchekenian; and the Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP), which sponsored this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menezes, J.C., Troster, E.J. & Dichtchekenian, V. Digoxin antibody decreases natriuresis and diuresis in cerebral hemorrhage. Intensive Care Med 29, 2291–2296 (2003). https://doi.org/10.1007/s00134-003-1955-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1955-0