Abstract
Objective
To investigate age-related differences in morphine requirements and metabolism in full-term neonates.
Design and setting
Randomized double-blind study in the pediatric surgical intensive care unit.
Patients
Sixty-eight neonates (52 aged under 7 days, 16 aged 7 day or older) following major surgery.
Interventions
After surgery patients were randomly assigned to continuous morphine (10 µg/kg per hour) or intermittent morphine (30 µg/kg per 3 hours). Additional morphine was administered on guidance of pain scores.
Measurements and results
Pain was measured by the Comfort behavioral scale and visual analogue scale. Morphine and morphine-6-glucuronide (M6G) plasma concentrations were determined before and 0, 6, 12, and 24 h after surgery. The younger neonates differed significantly from the older neonates in morphine requirement (median 10 vs. 10.8 µg/kg per hour), morphine plasma concentration [23.0 vs. 15.3 ng/ml), and M6G/morphine ratio (0.6 vs. 1.5). Pain scores did not differ between age groups or morphine treatment groups. Neonates who were mechanically ventilated longer than 24 h had significantly higher morphine plasma concentrations than the spontaneously breathing neonates 12 and 24 h after surgery (29.1 vs. 13.1 ng/ml and 26.9 vs. 12.0 ng/ml, respectively). Morphine plasma concentrations were not correlated with analgesia or respiratory depression. Five neonates (intermittent morphine) showed respiratory insufficiency; however, the difference between the groups was not significant.
Conclusions
Neonates aged 7 days or younger require significantly less morphine postoperatively than older neonates. The two morphine regimens (continuous, intermittent) were equally effective and safe. Mechanical ventilation decreases morphine metabolism and clearance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although health care professionals are becoming increasingly alert to pain management in neonates and infants [1, 2, 3, 4, 5, 6], adequate treatment of continuing pain is not guaranteed. We still do not know the morphine doses that provide sufficient analgesia after major surgery in newborn infants. Physiological alterations starting from birth, with improving hepatic and renal clearing capacity and changing volume of distribution, are likely to influence the efficacy and safety of morphine in the vulnerable neonate [7, 8, 9, 10, 11].
Previously we investigated in infants of different ages (0–3 years) the effects of two morphine administration regimens (continuous versus intermittent intravenously) on hormonal and metabolic stress responses and morphine requirement after major noncardiac surgery [12, 13]. We concluded that age was the most important variable because significant differences were found between neonates and older infants. Within the age groups differences between the two methods of morphine administration were found only in the older age groups.
In the present study we investigated the effect of developmental maturation on morphine metabolism in full-term neonates after thoracic or abdominal surgery. We distinguished between neonates aged 7 days or younger and those aged over 7 days, because hepatic and renal physiology change markedly during the first week after birth. The analysis included (a) age-related aspects, i.e., analgesia, morphine requirement, morphine and morphine-6-glucuronide (M6G) concentrations; and (b) effects of other clinical factors, i.e., apnea, mechanical ventilation, intermittent vs. continuous morphine.
Materials and methods
This study enrolled 68 neonates aged 0–4 weeks (gestational age 35–42 weeks; body weight 1500 g or more) admitted to the surgical intensive care unit following thoracic or abdominal surgery. Neonates with neurological, renal, or hepatic dysfunction, or with opioid therapy less than 6 h prior to surgery were excluded. The study protocol was approved by the Medical Ethics Committee of the Erasmus Medical Center, Rotterdam. Patients were enrolled only after informed consent had been obtained from the parents.
To analyze the effects of age we distinguished between neonates aged 7 days or younger (n=52) and those aged over 7 days (n=16). Table 1 gives their clinical and surgical characteristics. The two age groups showed no significant differences apart from age-related differences in weight, heart rate (HR), mean arterial blood pressure (MAP), and plasma concentrations of creatinine and bilirubin (Table 1).
Anesthetic management was completely standardized. Anesthesia was induced intravenously with 3–5 mg/kg thiopentone or by inhalation with halothane in oxygen. Fentanyl at 5 µg/kg was given before orotracheal intubation, which was facilitated with 0.5–1 mg/kg atracurium or 2 mg/kg suxamethonium. Ventilation was controlled and anesthesia was maintained with isoflurane 0.5 minimum alveolar concentration in 60% nitrous oxide in oxygen or air in oxygen. Perioperative fluids were standardized to maintain a glucose infusion rate between 4 and 6 mg/kg per minute; body temperature was kept within normal ranges. A peripheral artery was cannulated, and the measured MAP and HR data served as preoperative baseline values. Patients received a second dose of 5 µg/kg fentanyl before surgical incision. Additional doses of fentanyl 2 µg/kg were administered when HR and/or MAP was 15% above baseline value. At the end of surgery the neuromuscular block was antagonized, and the tracheal tube was removed. Mechanical ventilation was continued in patients who required ventilatory support.
The anesthetist then computed the Surgical Stress Score (SSS) to classify the degree of surgical stress [14]. This measure takes into account seven items: amount of blood loss, site of surgery, amount of superficial trauma, extent of visceral trauma, duration of surgery, associated stress factors (hypothermia, localized or generalized infection and prematurity), and cardiac surgery. The total scores in this study (excluding cardiac surgery and prematurity <35 weeks) ranged from 3 to 24. All neonates received a dose of morphine hydrochloride 100 µg/kg at the end of surgery and were randomly allocated to equivalent intravenous doses of continuous morphine infusions (CM, 10 µg/kg per hour) or intermittent morphine boluses (IM, 30 µg/kg per 3 hours). Pain was assessed by trained nurses before surgery and every 3 h for 24 h after surgery using the validated behavioral Comfort scale (CS; total scores range from 6 to 30) and visual analogue scale (VAS; ranging from 0 to10). Recently the behavioral part of the CS (referred to below as behavioral CS) has been confirmed as a reliable and valid instrument to assess postoperative pain in neonates and infants aged 0–3 years [15, 16]. The behavioral CS includes six behavioral items: alertness, calmness, respiratory response for ventilated or crying for nonventilated children, physical movement, muscle tone, and facial tension. VAS scores were assigned after every 2-min observation period in which the behavioral CS was scored. VAS scores of 4 or higher are taken to reflect moderate to severe pain. Every time the nurse scored a VAS of 4 or higher, the child was given an additional 5 µg/kg dose of morphine, repeated every 10 min when required.
Respiratory insufficiency was defined by the presence of apnea or arterial PaCO2 values of 7.3 kPa or higher in spontaneously breathing neonates [17]. Arterial blood samples were taken after induction of anesthesia (baseline), directly after surgery, and 6, 12, and 24 h postoperatively to determine blood gas values and plasma concentrations of morphine and M6G. Blood was sampled before an intermittent bolus was given; thus plasma concentrations in the IM group were measured at time points corresponding with trough plasma morphine concentrations. Standardized automated laboratory analyzers measured plasma total bilirubin and creatinine concentrations. Plasma levels of morphine and M6G were measured by high-performance liquid chromatography [18]. In serum all calibration graphs were linear: for morphine the concentrations ranged from 5 to 90 ng/ml and for M6G from 5 to 100 ng/ml. On average the quantitation limit was 5 ng/ml for morphine and M6G. However, in individual samples, the chromatogram allowed for a lower threshold. In this concentration range the intra- and interday coefficients of variation were less than 10% for all compounds and the accuracy was about 5%, indicating a high degree of precision.
Differences between younger (≤7 days) and older (>7 days) neonates in the need for additional morphine (yes/no) and various factors in the univariate analysis were analyzed by Fisher's exact test. Multivariate analysis was performed using logistic regression. Correlation coefficients are Spearman's ρ. Other tests used are given in the text. The level of p=0.05 (two-tailed) was considered the limit of significance. There were 37 mechanically ventilated and 15 nonventilated neonates during the first 24 h after surgery. The other neonates were ventilated for longer than 24 h. A post hoc power calculation shows that with these numbers differences in mean concentrations as small as approx. 0.8 SD can be detected (α=0.05, β=0.20), which difference generally is considered to be relatively small.
Results
Morphine
Six patients were excluded from morphine analysis, five because of detectable plasma morphine levels at baseline and one because of loss of the arterial line at the end of surgery. The five patients with detectable morphine concentrations at time 0 had received morphine more than 6 h before surgery. All these patients were on mechanical ventilation (congenital diaphragmatic hernia, n=4; meconium peritonitis, n=1); four of them were 7 days of age or younger (three CM, one IM), and one was 28 days of age (CM). The factors postnatal age, gestational age, sex, body weight, plasma concentration of creatinine and total bilirubin, preoperative and postoperative mechanical ventilation, SSS, and morphine treatment (CM or IM), were investigated for their relationship with the need for additional morphine (yes or no) during the first 24 h after surgery. Multivariate logistic analysis showed the only significant predictors of the need for additional morphine to be age (13/47 younger, 27%, vs. 10/15 older, 66%; p=0.006)] and preoperative mechanical ventilation (1/13 ventilated, 7%, vs. 22/48 nonventilated, 46%; p=0.014). Postoperative mechanical ventilation did not significantly influence the need for additional morphine. Table 2 presents the morphine requirement for each age group. Morphine requirement (related to body weight), was significantly lower in the younger neonates on CM (p<0.001, Mann-Whitney U test).
Morphine plasma concentrations
Table 3 presents the plasma concentrations of morphine and M6G and the M6G/morphine ratio in the both age and both treatment groups at the different time points. Median plasma concentrations of morphine 24 h after surgery were significantly higher in younger than older neonates in the CM group (p=0.027). Morphine plasma concentrations varied widely and were not indicative for additional morphine need in the postoperative period following these measured values. Figure 1 shows the plasma concentrations according to age (≤ 7 days and >7 days) and treatment (CM and IM) 6 and 12 h after surgery. Neonates who were mechanically ventilated longer than 24 h postoperatively (n=37) had significantly higher morphine plasma concentrations than nonventilated patients (n=15) 12 and 24 h after surgery (29.1 vs. 13.1 ng/ml and 26.9 vs. 12.0 ng/ml, respectively; both p<0.001). This difference in morphine plasma levels was not related to age or treatment regimen. Morphine requirements did not significantly differ between ventilated and nonventilated neonates.
Morphine plasma concentrations 6 h (left) and 12 h (right) after surgery, according to age (≤ 7 days or >7 days of age) and treatment group (continuous morphine, CM, or intermittent morphine, IM). Circles Plasma levels of patients who did not need additional morphine during next period (left 6–12 h, right 12–24 h); triangles plasma levels of patients who did need additional morphine during next period
Morphine-6-glucuronide plasma concentrations
M6G was detectable in the plasma of all neonates from 6 h after surgery. M6G plasma concentrations did not differ significantly between younger and older neonates. The median M6G/morphine ratio was significantly lower in younger neonates 6, 12, and 24 h after surgery (all p<0.04; Table 3). Although the plasma concentrations of M6G did not differ significantly between ventilated and nonventilated neonates, the M6G/morphine ratio was significantly lower in postoperatively mechanically ventilated neonates 12 and 24 h postoperatively (0.7 vs. 1.6 and 0.7 vs. 1.4, respectively; both p<0.02). The M6G/morphine ratios in neonates ventilated less than 24 h (n=10) lay between those of the ventilated and nonventilated neonates.
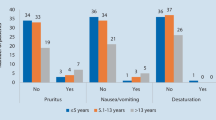
Physiological and behavioral responses
Table 4 presents the mean values of HR, MAP, and pain scores for the first 24 h postoperatively. Hemodynamic data could not be analyzed in 3 of the 68 neonates due to loss of the arterial line during the study. In multiple regression analysis mean HR varied positively with age and body weight (both p<0.05). MAP was related only to age and was significantly lower in younger neonates, even after adjusting for baseline values (p<0.001). Mean Comfort and VAS scores were correlated significantly with each other (r=0.7, p<0.001). Pain scores did not significantly differ between the two age cohorts or between the two treatment groups. Frequencies of VAS scores of 4 or higher (indicating pain) ranged from 0 to 3 and were not related to age, plasma concentrations of morphine or M6G, specific diagnosis, or type of surgery performed.
Respiratory depression
The number of spontaneously breathing neonates increased from 15 at 6 h (9 aged ≤ 7 days, 6 aged >7 days) to 22 at 24 h postoperatively (14 aged ≤ 7 days, 8 aged >7 days). Only one of them (duodenal atresia) showed increased PaCO2 levels of 8.9, associated with high morphine (trough) concentrations of 55 ng/ml 6 h after surgery. Four others (morphine trough plasma levels varying from 8 to 23.9 ng/ml) required intubation and mechanical ventilation: failed extubation after repair of esophageal atresia (n=2), apnea after repair of extrophy of the bladder (n=1) and jejunal atresia (n=1). All of these five neonates were on IM and in the younger group; none of them had received additional morphine in the postoperative period. Remarkably, two other of younger neonates on IM with morphine trough plasma levels of 29 and 59 ng/ml, respectively, at 6 h postoperatively did not manifest either hypercarbia or hypoventilation.
Other adverse effects
Hypotension related to the administration of morphine was not observed. Urinary retention could not be monitored because most of the neonates had a urinary catheter. As all had undergone major abdominal or thoracic surgery, it could not be established whether either surgery or morphine therapy had altered gut motility.
Discussion
This randomized, controlled trial evaluated the effects of age on morphine metabolism in full-term newborns. After surgery neonates aged 7 days or younger required fewer additional morphine doses, maintained higher plasma morphine levels, and converted less morphine to M6G (lower M6G/morphine ratios) than older neonates. The higher morphine plasma concentrations may in part result from a smaller volume of distribution at this age. While a meta-analysis showed that the morphine volume of distribution is not dependent on age [19], other studies have found the volume of distribution tended to be somewhat smaller in neonates aged 7 days or younger than in older infants, but this difference was not statistically significant [7, 10]. A morphine loading dose of 50 µg/kg probably suffices for neonates aged 7 days or younger, whereas 100 µg/kg is generally necessary in older infants.
A meta-analysis has calculated an initial morphine infusion of 7 µg/kg/h to be sufficient for postoperative pain treatment in full-term neonates [19]. An adjustment was suggested with regard to cardiac and noncardiac surgery (5 and 10–15 µg/kg per hour, respectively) [20]. In our study only 27% of the younger neonates required additional morphine compared with 66% of the older ones, suggesting that postoperative pain in some of the younger neonates could have been adequately treated with less morphine than the minimal dose used. Because all nurses were trained and qualified in using the Comfort Scale and were unaware of the later subanalysis between the young and older neonates, biased in their decisions for additional morphine can be excluded.
Findings from our study suggest that concentrations between 15 and 20 ng/ml are effective in postoperative neonates up to 4 weeks of age [21]. However, as documented earlier, morphine plasma concentrations ranged widely, and no significant correlation was found between plasma levels and the need for additional morphine during the following hours.
In a study comparing the effects of IM vs. CM in nonventilated infants (including 14 neonates under 1 month of age) 7% of the infusion group had respiratory problems even when adjusted to a target morphine plasma concentration of 20 ng/ml [21]. Although in the present study median morphine plasma concentrations were higher in neonates aged 7 days or less, none of the spontaneously breathing neonates in the CM group had respiratory problems. Five neonates, all on IM, showed respiratory depression. In only one of them this could be attributed to the morphine therapy because periods of apnea started 30 min after a morphine bolus dose. In the others the respiratory problems largely resulted from surgical complications. This suggests that morphine plasma concentrations alone are not necessarily indicative of ventilatory depression.
In the present study, mechanical ventilation was associated with higher plasma morphine levels, similar plasma M6G levels, and lower M6G/morphine ratios. In five neonates, who were on ventilation preoperatively and had been without morphine therapy longer than 6 h, morphine was still detectable at the time of surgery. Data on the clinical consequences of mechanical ventilation on portal hemodynamics and renal function are conflicting [22, 23]. However, although morphine metabolism is more dependent on the glucuronidation capability, a slower morphine metabolism and a longer elimination time may be the result of a decreased hepatic and renal perfusion due to positive end-expiratory pressure. Decreased M6G production combined with reduced renal clearance can explain the similar M6G plasma concentrations and higher morphine in mechanically ventilated neonates. Bearing in mind the individual variability in morphine clearance, at this young age a 6-h period is apparently too short to effectively clear plasma of morphine [10], especially under conditions of mechanical ventilation. This phenomenon can also explain why neonates who had been mechanically ventilated before surgery needed less morphine after surgery.
Postoperative ventilation did not influence the need for additional morphine. However, in spite of the nonsignificant differences in morphine requirements between postoperatively ventilated and nonventilated neonates the mechanically ventilated neonates proved to have higher plasma concentrations of morphine.
Although we realize that the included patients were heterogeneous in their kind of surgery and complications, this is the normal population in our pediatric surgical intensive care unit. All patients were scheduled for major surgery, and no significant differences were found in their SSS. Actually, we think that the inclusion of this heterogeneous population contributes to the power of this study. Excluding the patients who were on mechanical ventilation would have resulted in loss of important information.
The clinical effect of morphine also relies on the formation of its active metabolite M6G. Morphine is largely metabolized by the age-dependent isoform uridine 5′-diphosphate glucuronosyl transferase (UGT)-2B7 to M6G and M3G [24]. In this study the M6G/morphine ratio was significantly lower in the younger neonates, probably as a result of the low UGT activity at this age.
Remarkably, the hemodynamic variables (HR and MAP) showed no significant correlation with pain scores. This questions the reliability of HR and MAP as parameters for pain measurement in this age group [25].
Conclusions
The findings from the present study suggest that in neonates aged over 7 days a morphine dose of 10 µg/kg per hour is sufficient for postoperative analgesia after noncardiac major surgery. Hepatic and renal disturbances, however, may require dose adjustment. For neonates aged 7 days or younger an initial morphine infusion of 5–10 µg/kg per hour is recommended, after a loading dose of 50 µg/kg. Further research into morphine requirements in this age group is needed. Morphine plasma concentrations varied widely. We found no consistency between morphine plasma levels and analgesia or between plasma levels and respiratory depression. Although in the present study the CM and IM groups showed no significant differences in safety, the IM regimen did not provide any advantage. Morphine given as a continuous infusion is more feasible and might be regarded as safer in neonates. Further findings from this study suggest that neonates on mechanical ventilation have a slower morphine metabolism than spontaneously breathing neonates. Behavioral observation can be used as indication for tapering off the morphine infusion, thus preventing overdosing with its associated risks.
References
Choonara I (1999) Why do babies cry. BMJ 319:1381
Lima de J, Lloyd-Thomas AR, Howars RF, Sumner E, Quinn TM (1996) Infant and neonatal pain anaesthetists' perceptions and prescribing patterns. BMJ 313:787
Anand KJS (2001) Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med 155:173–180
Anand KJS, Sippell WG, Aynsley-Green A (1987) Randomized trial of fentanyl anesthesia in preterm babies undergoing surgery: effects on the stress response. Lancet I:243–248
Fitzgerald M, Millard C, McIntosh N (1989) Cutaneous hypersensitivity following peripheral tissue damage in newborn infants and its reversal with topical anesthesia. Pain 39:31–36
Anand KJS, Scalzo FM (2000) Can adverse neonatal experiences alter brain development and subsequent behavior? Biol Neonate 77:69–82
Lynn AM, Slattery JT (1987) Morphine pharmacokinetics in early infancy. Anesthesiology 66:136–139
Choonara IA, McKay P, Hain R, Rane A (1989) Morphine metabolism in children. Br J Clin Pharmacol 28:599–604
McRorie TI, Lynn AM, Nespeca MK, Opheim KE, Slattery JT (1992) The maturation of morphine clearance and metabolism. Am J Dis Child 146:972–976
Pokela ML, Olkkola KT, Seppälä T, Koivisto M (1993) Age-related morphine kinetics in infants. Dev Pharmacol Ther 20:26–34
Faura CC, Collins SL, Moore RA, McQuay HJ (1998) Systematic review of factors affecting the ratios of morphine and its major metabolites. Pain 74:43–53
Bouwmeester NJ, Anand KJS, Dijk van M, Hop WCJ, Boomsma F, Tibboel D (2001) Hormonal and metabolic stress responses after major surgery in children aged 0–3 years: a double-blind, randomized trial comparing the effects of continuous versus intermittent morphine. Br J Anaesth 87:390–399
Bouwmeester NJ, van den Anker JN, Hop WCJ, Anand KJS, Tibboel D (2003) Age- and therapy-related effects on morphine requirements and plasma concentrations of morphine and its metabolites in postoperative infants. Br J Anaesth 90:642–652
Anand KJS, Aynsley-Green A (1988) Measuring the severity of surgical stress in newborn infants. J Pediatr Surg 23:297–305
Ambuel B, HamLett KW, Marx CM, Blumer JL (1992) Assessing distress in paediatric intensive care environments: the Comfort scale. J Pediatr Psychol 17:95–109
Dijk van M, Boer de JB, Koot HM, Tibboel D, Passchier J, Duivenvoorden HJ (2000) The reliability and validity of the COMFORT scale as a postoperative pain instrument in 0–3 year-old infants. Pain 84:367–377
Lynn AM, Nespeca MK, Opheim KE, Slattery JT (1993) Respiratory effects of intravenous morphine infusions in neonates, infants, and children after cardiac surgery. Anesth Analg 77:695–701
Verwey-van Wissen CP, Koopman-Kimenai PM, Vree TB (1991) Direct determination of codeine, norcodeine, morphine and normorphine with their corresponding O-glucuronide conjugates by high-performance liquid chromatography with electrochemical detection. J Chromatogr 570:309–320
Kart T, Christrup LL, Rasmussen M (1997) Recommended use of morphine in neonates, infants and children based on a literature review. II. Clinical use. Pediatr Anaesth 7:93–101
Lynn AM, Nespeca MK, Bratton SL, Strauss SG, Shen DD (1998) Clearance of morphine in postoperative infants during intravenous infusions: the influence of age and surgery. Anesth Analg 86:958–963
Lynn AM, Nespeca MK, Bratton SL, Shen DD (2000) Intravenous morphine in postoperative infants: intermittent dosing versus targeted continuous infusions. Pain 88:89–95
Richard C, Berdeaux A, Delion F, Riou B, Rimailho A, Giudicelli JF, Auzepy P (1986) Effect of mechanical ventilation on hepatic drug pharmacokinetics. Chest 90:837–841
Mutlu GM, Mutlu EA, Factor P (2001) GI Complications in patients receiving mechanical ventilation. Chest 119:1222–1241
Coffman B, Rios GR, King CD, Tephly TR (1997) Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab Dispos 25:1–4
Dijk M van, Boer de JB, Koot HM, Duivenvoorden HJ, Passchier J, Bouwmeester N, Tibboel D (2001) The association between physiological and behavioral pain measures in 0- to 3-year old infants after major surgery. J Pain Symptom Manage 22:600–609
Acknowledgements
The laboratory assistance of Dr. P.M. Koopman-Kiemenai, Department of Clinical Pharmacy, University Hospital Nijmegen, is gratefully acknowledged. We also thank the pharmacists, the anesthetists, surgeons, anesthetic nurses, intensivists, and pediatric ICU nurses of the Sophia Children's Hospital for their co-operation, Mrs. L. Visser-Isles and Mr. K. Hagoort (Erasmus Medical Center, Rotterdam) for the editing, and, finally, the parents and their children, who allowed this study to take place.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was supported by The Netherlands Research Council (NWO, The Hague) and the Sophia Foundation for Medical Research.
Rights and permissions
About this article
Cite this article
Bouwmeester, N.J., Hop, W.C.J., van Dijk, M. et al. Postoperative pain in the neonate: age-related differences in morphine requirements and metabolism. Intensive Care Med 29, 2009–2015 (2003). https://doi.org/10.1007/s00134-003-1899-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1899-4