Abstract
Objective
To compare the health-related quality of life (HR-QOL) in acute respiratory distress syndrome (ARDS) survivors with that in a matched control group of non-ARDS survivors.
Design and setting
Prospective, matched, parallel cohort study, comparing HR-QOL between intensive care unit (ICU) survivors with ARDS and a control group in a tertiary care hospital.
Patients
Between May 1997 and December 2000, all ARDS adult patients of an eight-bed medical/surgical unit of a tertiary care hospital were enrolled and a control group of non-ARDS survivors, matched for severity of disease and for previous health state, was selected. The study included 29 ARDS survivors who answered the EQ-5D questionnaire and had lung function evaluated.
Measurements and results
A follow-up appointment was performed 6 months after ICU discharge consisting of: (a) evaluation of HR-QOL using EQ-5D and (b) lung function tests and measure of diffusing capacity. Among ARDS survivors 41% had normal lung function and 59% mild to moderate lung function impairments. Nearly a one-third of ARDS survivors reported problems in one or more of the five dimensions of the EQ-5D, and 48% reported feeling worse at the interview than 6 month before ICU admission. No significant differences were found in HR-QOL between ARDS survivors and other ICU survivors with similar age and matched for previous health state and severity of disease.
Conclusions
This study suggests that impairments in HR-QOL among ARDS survivors may not be distinguishable from that among other ICU survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The acute respiratory distress syndrome (ARDS) is a rapidly progressive illness associated with high morbidity and mortality which requires aggressive therapy and advanced technological support. Recent reports suggest that the mortality rate has declined, but it still ranges between 34% and 60% [1, 2]. Consequently the main concerns relating to ARDS patients have been ways of improving survival. More recent outcome studies have documented residual pulmonary dysfunction after ARDS [3, 4, 5]. Health-related quality of life (HR-QOL) has also been studied, with most authors reporting lower HR-QOL in ARDS survivors than in the normal population [5, 6, 7, 8, 9]. Moreover, reductions in HR-QOL of ARDS survivors compared with critically ill controls have also been suggested by one study [10].
A number of factors make HR-QOL evaluation difficult: (a) those related to the HR-QOL evaluation in general, such as the timing of data collection, the choice of particular dimensions to be included, and the lack of consensus over the instruments to be used; (b) those related to HR-QOL specifically after ARDS, such as the lack of an appropriate comparison group, the lack of previous HR-QOL evaluation [10, 11], the extent to which ARDS sequelae influence HR-QOL. The cost-effectiveness of the treatment in ARDS patients has also been studied [11, 12].
The aim of this study was to compare HR-QOL in ARDS survivors with that in similar ICU survivors, using a control group without ARDS and matched by previous health state and severity of disease.
Patients and methods
The study addressed all adult patients (18 years old or more) admitted to an eight-bed medical/surgical ICU between May 1997 and December 2000 in whom ARDS was diagnosed according to the criteria of the American-European Consensus Conference on ARDS: acute onset: PaO2 of 200 mmHg or lower; bilateral infiltrates on frontal chest radiograph, Paw of 18 mmHg or lower, or no clinical evidence of left atrial hypertension [13]. Survivors with previous chronic lung disease (chronic bronchitis and emphysema) were excluded.
Background variables included patient's gender, age, main activity, smoking habits, and previous (i.e., premorbid) health status. Previous health status was evaluated according to three categories: healthy, chronic nondisabling diseases (i.e., able to keep work or normal daily activities) and chronic disabling diseases (i.e., unable to work or to undertake normal daily activities). One of the authors classified all patients according to one of these three categories. ICU variables included severity of disease at admission, length of stay and diagnosis. ARDS variables included primary or secondary pulmonary lesion, days of ventilation, lung injury score, maximum values of positive end-expiratory pressure (PEEP), and the number of days with a FIO2 greater than 60%.
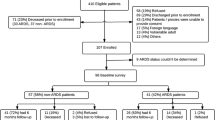
From a total of 1251 patients, 88 with the diagnosis of ARDS were enrolled in the study; 26 of these died in the ICU and another 7 in the ward (38% in-hospital mortality rate). Three patients died after hospital discharge but before the 6-month evaluation. Nine patients were excluded for previous chronic lung disease, and another 14 were lost to follow-up (i.e., nonrespondents; Table 1). A follow-up appointment was performed 6 months after ICU discharge consisting of an evaluation of HR-QOL using EQ-5D [14], lung function tests, and measure of diffusing capacity (DLCO). DLCO was measured by the single-breath carbon monoxide technique. SensorMedics Vmax22 was the pulmonary system used. Recommendations for standard technique (ATS update 1995) were followed. Six months after ICU discharge 29 patients completed EQ-5D questionnaire and had their lung function evaluated. The most frequent diagnoses were pneumonia (n=13), sepsis (n=7), aspiration (n=2), multiple trauma (n=2), and intoxication (n=2).
HR-QOL was measured using EQ-5D questionnaire. This is a generic measure instrument designed to measure health outcome, which was developed at a European level [14, 15]. The EuroQol Group originally developed the Portuguese version of the EQ-5D in 1998 (EuroQol Group Newsletter, January 2000). The EQ-5D comprises two parts: the EQ-5D self-classifier, a self-reported description of health problems according to a five dimensional classification i.e., mobility, self-care, usual activities, pain/discomfort and anxiety/depression (see Table 5 for description of the EQ-5D self-classifier); the EQ visual analogue scale (VAS), a self-rated health status of a form similar to a thermometer to record perceptions of participants own current overall health; the scale is graded from 0 (the worst imaginable health state) to 100 (the best imaginable state) [15] (EuroQol Group Newsletter, January 2000). In both the time frame is the current day. Because the ICU stay was only 6 months before the interview, the "perceived current health status" asked in the EQ-5D questionnaire was changed from "compared with my general level of health over the past 12 months my health state today is better/the same/worse" to "compared with my general level of health 12 months ago my health state today is better/the same/worse." An index (EQ Index), based on the five dimensions and the EQ VAS and ranging from 0 to 100 was also calculated and used to describe the overall QOL of these patients [16, 17].
All questionnaires were administered by one of the authors during a follow-up consultation 6 months after ICU discharge. A matched control group was created, with two controls for each survivor of ARDS, with the same previous health state and similar Acute Physiology and Chronic Health Evaluation (APACHE) II (±2 units), which were randomly selected among other ICU survivors without the diagnosis of ARDS. Scheduled surgery patients were excluded from controls, as there were no scheduled surgery patients among ARDS respondents.
Pearson's χ2 test was used for analysis of categorical data, and the Mann-Whitney test was used for continuous variables with asymmetrical distribution. Friedman's test for matched ordinal data was used to compare EQ-5D dimensions and the paired sample t test to compare EQ VAS and EQ Index dimensions between ARDS group and the two paired control groups. Statistical significance was set at p<0.05. The hospital's ethics committee approved the study.
Results
There were significant differences between survivors and nonsurvivors concerning background variables with the latter being significantly older than the former. Concerning ICU variables, we found significant differences in severity of disease, as those who died had more severe disease, as measured by APACHE II. We also found differences in ARDS variables, as the lung injury score was significantly higher in nonsurvivors. There were no significant differences between respondents and nonrespondents except in the time of ventilation and ICU length of stay (Table 1). Differences between respondents and nonrespondents in the control group were not explored as we have previously found that there were no differences in a group including all patients admitted in the ICU [18].
Of the 29 survivors 17 exhibited abnormalities in lung function (Table 2). Lung function impairments were mild to moderate, and many patients had impairments only in carbon monoxide diffusion. There were no significant differences between those survivors with normal lung function and those with residual pulmonary dysfunction, either in background variables, ICU variables, or ARDS variables. Patients with impairments in lung function were older, had a longer ventilation time, stayed longer in the ICU, and needed a FIO2 greater than 60% for more days than survivors with normal lung function (Table 3). However, as none of these differences were statistically significant, we decided to analyze together these patients regarding their HR-QOL.
There were no differences between ARDS survivors and the matched control group concerning background variables (gender, age, main activity, smoking habits, and previous health state). Concerning ICU variables we found a significantly longer ICU stay in ARDS survivors (Table 4).
No significant differences were found in HR-QOL when evaluated by EQ-5D between ARDS survivors and other ICU survivors (control group; Table 5). Concerning the five dimensions, and except for anxiety/depression, there was even a trend for ARDS survivors to report fewer problems than the control group, although not reaching statistical significance. ARDS survivors reporting no problems in all five dimensions of the EQ-5D ranged from 52% for anxiety/depression to 86% for mobility and self-care; However, no other trend was observed, as there were no differences either in EQ VAS or EQ Index between the two groups. Concerning perceived current health state, 48% on the ARDS group and 30% in the control group claimed to be worse than 12 months previously (Table 5).
Discussion
This study found ARDS mortality to be significantly associated with age, severity of disease, and severity of ARDS. These findings agree with those of previous studies in which age [2, 19, 20] and lung injury score [2] were associated with mortality. Mild to moderate impairments in lung function have been previously described [3, 5, 7, 9], and we found a similar (approx. 60%) proportion of ARDS survivors with these impairments. Moreover, although not statistically significant, it was apparent that patients with impairments in lung function were older, had a longer ventilation time, stayed in the ICU longer, and needed FIO2 greater than 60% for more days. These findings agree with those of McHugh et al. [3] who reported that improvement in lung function was related to a higher severity of lung injury and duration of ventilation. ARDS survivors also had a significantly longer median hospital stay, a finding similar to that of McHugh et al. [3], Davidson et al. [10] and more recently from Herridge et al. [5]. As in other reports [6, 7], we found a fair HR-QOL among ARDS survivors, although nearly one-third reported problems in at least one of the five dimensions of the EQ-5D.
To our knowledge, this is the first study using EQ-5D in a cohort of ARDS survivors. Together with SF-36, this instrument has been recently recommended as the best suited instrument to be used in critical care outcome studies [21]. The most striking finding in this study is that there were no differences in HR-QOL between ARDS survivors and a control group with similar age and matched for previous health state and severity of disease, which contrasts with a study from Davidson et al. [10]. However, some differences in the study design and methods may explain these conflicting results: our control group was matched for both severity of disease and previous health state, as these variables were found to be determinants of HR-QOL [18]. On the other hand, Davidson et al. [10] addressed a control group of critical patients matched for severity of disease and for diagnosis. Also, their study included only trauma and sepsis patients, patients with previous chronic lung disease were not excluded, and there is no information on their previous health status. Moreover, SF-36 was the generic questionnaire that was administered. More recently Herridge et al. [5] drew our attention to the fact that the long-term effect of ARDS may be related to age and preexisting pulmonary function and may thus be cohort specific, which may help to explain different results between different studies.
This study presents some limitations. Firstly, we acknowledge the relatively small number of ARDS survivors involved and the consequent reduction in statistical power that could have prevented us from finding significant differences. However, it should be underlined that the differences in HR-QOL found between ARDS survivors and their controls were not only very small but also had an unexpected direction as ARDS survivors reported less moderate to extreme problems in most EQ-5D dimensions. Secondly, ARDS nonrespondents showed significantly shorter ICU stay and fewer days of ventilation regarding ARDS respondents. Should these differences result in a selection bias, its direction would increase the relative proportions of severe ARDS patients included in our sample, which would probably result in a worse HR-QOL.
Several long-lasting effects of ICU stay have been described after ARDS, including posttraumatic stress disorder [6], cognitive sequelae [8], and the rehabilitation phase after a long, debilitating hospitalization [11]. Therefore one can expect reductions in HR-QOL in ARDS survivors, related either directly to residual pulmonary dysfunction or to prolonged ICU stays. This study suggests that these reductions may not be distinguishable from those in other critical patients with similar age and matched for severity of disease and previous health state.
Two main conclusions may be driven from this study. Firstly, HR-QOL of ARDS survivors may not differ from HR-QOL of other ICU survivors, which should encourage early and aggressive treatment of ARDS to improve survival. Secondly, as with other authors [5, 6, 7], we were able to identify some of the sequelae of these survivors, so ARDS survivors should be included in follow-up clinics to reduce the long-term effect of the sequelae and to help them recover to their previous level of HR-QOL more quickly and more efficiently.
References
Ware LB, Matthay M (2000) The acute respiratory distress syndrome. N Engl J Med 342:1334–1349
Rocco TR Jr, Reinert SE, Cioffi W, Harrington D, Buczko G, Simms HH (2001) A 9-year, single institution, retrospective review of death rate and prognostic factors in adult respiratory distress syndrome. Ann Surg 233:414–422
McHugh LG, Milberg JA, Whitcomb ME, Schoene RB, Maunder RJ, Hudson LD (1994) Recovery of function in survivors of the acute respiratory distress syndrome. Am J Respir Crit Care Med 150:90–94
Hert R, Albert RK (1994) Sequelae of the adult respiratory distress syndrome. Thorax 49:8–13
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky A (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Preub U, Bullinger M, Schuffel W, Peter K (1998) Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 26:651–659
Schelling G, Stoll C, Vogelmeier C, Hummel T, Behr J, Kapfhammer HP, Rothenhausler HB, Haller M, Durst K, Krauseneck T, Briegel J (2000) Pulmonary function and health-related quality of life in a sample of long-term survivors of the acute respiratory distress syndrome. Intensive Care Med 26:1304–1311
Hopkins RO, Weaver LK, Pope D, Orme JF Jr, Bigler ED, Larson-Lohr V (1999) Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. Am J Respir Crit Care Med 160:50–56
Cooper AB, Ferguson ND, Hanly PJ, Meade MO, Kachura JR, Granton JT, Slutsky AS, Stewart TE (1999) Long-term follow-up of survivors of acute lung injury: lack of effect of a ventilation strategy to prevent barotrauma. Crit Care Med 27:2616–2621
Davidson TA, Caldweel ES, Curtis JR, Hudson LD, Steinberg KP (1999) Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill patients. JAMA 281:354–360
Angus DC, Musthafa AA, Clermont G, Griffin MF, Linde-Zwirble WT, Dremsizov TT, Pinsky MR (2001) Quality-adjusted survival in the first year after the acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1389–1394
Hamel MB, Phillips RS, Davis RB, Teno J, Connors AF, Desbiens N, Lynn J, Dawson NV, Fulkerson W, Tsevat J (2000) Outcomes and cost-effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med 109:614–620
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R, The Consensus Committee (1994) Report of the American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. Intensive Care Med 20:225–232
EuroQol Group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Brooks R, with the EuroQol Group (1996) EuroQol: the current state of play. Health Policy 37:53–72
Kuilman M, Bleeker JK, Hartman JAM, Simoons ML (1999) Long-term survival after out-of-hospital cardiac arrest: an 8 year follow-up. Resuscitation 41:25–31
Dolan P (1997) Modeling valuations for EuroQol health states. Med Care 35:1095–1108
Granja C, Teixeira-Pinto A, Costa-Pereira A (2002) Quality of life after intensive care—evaluation with EQ-5D. Intensive Care Med 28:898–907
Ely EW, Wheeler AP, Thompson BT, Ancukiewicz M, Steinberg P, Bernard GR for the Acute Respiratory Distress Syndrome Network (2002) Recovery rate and prognosis in older persons who develop acute lung injury and the acute respiratory distress syndrome. Ann Intern Med 136:25–36
Suchyta MR, Clemmer TP, Elliot CG, Orme Jr JF, Morris AH, Jacobson J, Menlove R (1997) Increased mortality of older patients with acute respiratory distress syndrome. Chest 111:1334–1339
Angus D, Carlet J (2003) Surviving intensive care: a report from the 2002 Brussels Roundtable. Intensive Care Med 29:368–377
Acknowledgements
We thank Alexandra Vieira and Luís Filipe Azevedo for their invaluable help in data management and analysis, and Paula Simão and Paula Negrão for their assistance in lung function evaluation.
Author information
Authors and Affiliations
Corresponding author
Additional information
An editorial regarding this article can be found in the same issue (http://dx.doi.org/10.1007/s00134-003-1855-3)
Rights and permissions
About this article
Cite this article
Granja, C., Morujão, E. & Costa-Pereira, A. Quality of life in acute respiratory distress syndrome survivors may be no worst than in other ICU survivors. Intensive Care Med 29, 1744–1750 (2003). https://doi.org/10.1007/s00134-003-1808-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1808-x