Abstract
Objective
To evaluate the risk factors for the development of acute renal failure (ARF) in severe rhabdomyolysis.
Design
Observational historical cohort study.
Setting
General intensive care unit of a university hospital.
Patients
Twenty-six patients with severe rhabdomyolysis, who were admitted between July 1996 and July 2001.
Measurements and results
Clinical and laboratory data were reviewed and groups were stratified according to presence or absence of acute renal failure. The underlying cause of rhabdomyolysis was ischemia by vascular obstruction (50%), crush injury by trauma (23%), sepsis (11.5%), heatstroke/hyperthermia (11.5%) and hyponatremia in a single patient. Mean creatine kinase (CK) level was 38,351±35,354 U/l on admission and rose further in all patients (mean: 59,747±67,514 U/l). Renal failure developed in 17 patients (65%). Serum CK levels correlated with onset of ARF, as these patients had significantly higher admission and peak serum CK concentrations. Patients with ARF had a higher mortality (59% vs 22%).
Conclusion
In our cohort of patients with severe rhabdomyolysis the level of serum CK predicted the development of ARF. Although our results suggest that series of CK determination might be beneficial for the evaluation of the effect of therapy, the value of CK determination as a prognostic tool is limited, given the wide range of CK levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rhabdomyolysis is a clinical and laboratory syndrome defined by injury to the sarcolemma of skeletal muscle, which results in leakage of its content into the plasma and urine. Rhabdomyolysis is most commonly caused by direct physical trauma to skeletal muscle as a result of crush injury, extreme exercise, or epileptic seizures. Muscular ischemia is associated with rhabdomyolysis, most likely due to reperfusion injury after restoration of adequate blood flow. Other causes include hereditary disorders such as carnitine palmitoyltransferase II deficiency, malignant hyperthermia and inflammatory disorders such as dermatomyositis and polymyositis. Lastly, fulminant rhabdomyolysis has been associated with the use of HMG-CoA reductase inhibitors, and the use of toxic substances (ethanol, cocaine and amphetamine) [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. In the intensive care unit rhabdomyolysis is most commonly caused by extensive muscular trauma after crush injuries or vascular obstruction [11, 12]. Serum creatine kinase (CK) is one of the most sensitive indicators of muscle damage and is invariably elevated in rhabdomyolysis [2]. Typically, there is an increased myoglobin concentration in urine and serum [13].
Acute renal failure (ARF) is the most important complication of rhabdomyolysis. The incidence of ARF in patients with rhabdomyolysis ranges from 10% to 30%, depending on the series cited [11]. The onset of ARF in rhabdomyolysis is associated with profound changes of electrolyte balance with hyperkalemia, hyperphosphatemia, hypocalcemia, and metabolic acidosis. The precise mechanisms of ARF in rhabdomyolysis are unclear, but most studies point to tubule obstruction by precipitation of myoglobin, tubular necrosis, and the role of lipid peroxidation, and finally renal vasoconstriction due to hypovolemia and the use of vasoactive medication [1, 11, 12, 14, 15, 16, 17]. The major goal in treatment of rhabdomyolysis is the prevention of ARF. The cornerstone of the prevention of ARF development is aggressive and early volume replacement. Likewise, alkalinization of urine by bicarbonate therapy in order to facilitate myoglobin excretion is of value in the prevention of ARF [12, 17, 18, 19, 20, 21]. Once present, ARF constitutes a major contributing factor to morbidity and mortality in patients with rhabdomyolysis [14, 22]. Identification of patients at high risk of developing ARF is thus a highly desirable goal. It is unclear which factors predispose the patient with rhabdomyolysis to ARF. Some studies have focused on myoglobinuria but failed to establish it as a risk factor for development of ARF [13, 23, 24]. We therefore set out to identify the laboratory and clinical parameters that would predict the onset of ARF in patients with acute, severe rhabdomyolysis.
Patients and methods
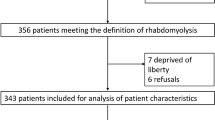
We identified cases of severe rhabdomyolysis by review of laboratory records of patients aged 18 years or older who were admitted between July 1996 and July 2001 to the intensive care unit of the University Medical Centre, Nijmegen. Severe rhabdomyolysis was defined primarily on the basis of elevated serum CK levels of greater than 10,000 U/l at some time during hospitalization in the intensive care unit. The CK limit of 10,000 U/l is 50-times higher than the normal upper limit in adults for our laboratory (200 U/l). Serum CK levels, as well as other biochemical parameters, were measured with standard clinical chemical assays with the aid of a Hitachi 747 Analyzer (Roche Diagnostics, Almere, The Netherlands). As we sought cases of severe rhabdomyolysis, we excluded 41 patients with elevated CK levels due to myocardial infarction (27 patients) and cardiac surgery (ten patients). Patients with a cerebral vascular accident were also excluded, as damage to cerebral tissue could give rise to plasma CK isoenzyme levels. However, in the 5-year period there were no patients with a cerebral vascular accident admitted to the ICU with CK levels >10,000 U/l. Likewise, patients with end-stage renal disease who were dependent on renal replacement therapy before being admitted to the ICU were also excluded from the analysis (four patients). The etiology of rhabdomyolysis was determined by chart review. The clinical factors that were investigated were development of renal failure and duration to recovery. Acute physiology and chronic health evaluation (Apache) II scores were recorded upon the patients' admission. The following laboratory parameters were included in the analysis: admission and peak serum concentrations of CK, creatinine, phosphorus and potassium together with the lowest ionized calcium concentration, and pH value. ARF was defined as a decline in renal function to such an extent as to warrant hemodialysis or any other form of renal replacement therapy. Groups were stratified according to presence or absence of ARF.
Statistical tests
Mean values with standard deviations are presented throughout. We used Student's t-test to compare group means. Where indicated, in cases of skewed datasets the non-parametric Mann–Whitney U test was used for intergroup comparisons. Descriptive data were compared by Chi-square testing. P values less than 0.05 were considered to be statistically significant.
Results
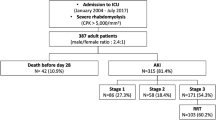
Between July 1996 and July 2001 approximately 7,500 patients were admitted to the ICU. Serum CK concentrations (>10,000 U/l) were detected in only 71 patients. In total, 30 patients met the entrance criteria for severe rhabdomyolysis. Four patients were excluded because charts were not available. Mean age of the patients in our group was 53 years (±21 years), and 21 patients (80%) were male. The median stay on the intensive care unit was 8 days (range 2–48 days). The underlying cause of rhabdomyolysis was ischemia by vascular obstruction (13 patients, 50%), and trauma (six patients, 23%), followed by sepsis, heatstroke/hypothermia in three patients each (11.5%), and lastly, hyponatremia in a single patient. The mean APACHE II score in the population that was studied was 20 (SD ±8). All but one patient received mechanical ventilation and 18 patients (69%) were in need of vasopressor support. Twelve patients (46%) died after an average stay of 5 days (SD ±3 days) on the intensive care unit. The fluid balance in the first 48 h of admission in our cohort was strongly positive (8,172 ml, SD ±3,895 ml). CK concentrations peaked within 24 h in the majority (54%) of patients. By definition, CK levels were highly elevated on the patients' admission, (38,351 U/l, SD ±35,354U/l; median, 26,000 U/l; range, 1,034–152,700 U/l), and rose further (maximum 59,747 U/l, SD ±67,514 U/l; median, 37,815 U/l; range, 11,400–152,700 U/l). Serum or urine myoglobin concentration was tested only once at admission in 5/26 patients. This parameter has hitherto no value in the analysis. Urine pH was tested in 12 patients (46%) and only two patients had proper alkalinized urine.
Acute renal failure
Renal failure developed in 17 patients (65%), invariably during the first 48 h after their admission. Table 1 depicts the clinical and laboratory variables, with renal failure as divergent factor. There was no difference with respect to cause of rhabdomyolysis between the two groups. The mortality, however, in patients with rhabdomyolysis and ARF was nearly three times that of patients without ARF, although this did not reach statistical significance. Interestingly, patients with ARF could not be discerned from those without ARF on the basis of admission creatinine levels. Serum CK concentrations, however, correlated with ARF, as these patients had both significantly higher admission (P<0.05; Fig. 1) and peak (P<0.05; Fig. 2) serum CK concentrations. Kinetic analysis showed that CK values declined faster in patients without renal failure (Fig. 3). There was no correlation between serum creatinine and CK concentrations, either on admission or on the day of peak CK.
Kinetic analysis of CK levels in patients with (closed squares) and without (open squares) renal failure. Note that values in patients without renal failure are lower and that there is a trend toward earlier decline of CK values. Symbols represent mean values; vertical lines indicate standard error of means
Discussion
The present study analyzed a cohort with clinically important rhabdomyolysis, using data that were collected in a 5-year-span at a general intensive care unit of a university hospital. Rhabdomyolysis is a serious condition that is associated with a high mortality rate. Indeed, in our study population the mean APACHE II score was 20±8 points, predicting a mortality rate of 38±22%, which accords with the true mortality of 46%. As is evident from our study, patients with rhabdomyolysis are at risk of ARF, and 17 patients (65%) developed ARF in the first 48 h after admission. In patients who developed ARF, the APACHE II scores were significantly higher than in those who did not have renal failure, and this corresponded with the three-times higher mortality rate. Our study identified CK levels as an important risk factor for the development of ARF. Patients with ARF had both higher admission and peak CK concentrations. Our data might suggest that CK could be used to predict ARF in patients with rhabdomyolysis. Application of CK as a clinical tool, however, is hampered by the wide range of individual serum CK concentrations. We failed to detect a relationship between etiology, age, gender, duration of stay at the ICU, or medical history, with the development of ARF. This suggests that ARF per se, irrespective of cause of rhabdomyolysis, is an important factor in the determination of the prognosis of patients. Although we noted that CK levels declined slower in renal-failure patients, we would like to inject a note of caution, as there are missing data from various time points, which limits the number of patients that we could compare and precludes interpretable statistical analysis. It is of interest to note that despite temporary renal replacement therapy, there was no evidence of chronic renal failure at follow-up in the surviving patients.
Rhabdomyolysis in our study was primarily due to vascular disorders (vascular thrombosis or embolus) or due to ischemia–reperfusion injury after traumatic crush injury. This concurs with one study [25] but contrasts with another published report [2]. Here, alcohol abuse, muscle compression, and seizures, were among the three most common causes of rhabdomyolysis, as well as differences in case-mix. Most likely the low cut-off level of CK serum concentrations (4,500 U/l) in the last study accounts for these differences. We used 10,000 U/l as a cut-off level and were able to diagnose rhabdomyolysis in only 30/71 of admitted patients, which emphasizes the importance of clinical assessment. Measurement of plasma or urine myoglobin (reflecting the degree of muscle injury) can be used as a confirmatory test. However, it has not gained wide popularity in clinical practice as it requires laborious and costly tests, the interpretation of results is hampered by unpredictable renal and hepatic elimination of plasma myoglobin, and correlation with the degree of myoglobinemia is poor [1, 9, 13, 23].
The pathophysiological mechanisms of ARF in rhabdomyolysis are diverse and are, in most instances, multifactorial. Hypotension and shock impair glomerular filtration due to reactive renal vasoconstriction, which results in decreased renal perfusion. As a result, oxygen delivery is reduced and renal tubular cell dysfunction impends. Hypovolemia is initiated by capillary leak syndrome and movement of intravascular plasma into damaged muscle [1, 12, 16, 18, 21, 25]. Volume expansion was initiated in all patients with or without use of vasoactive medication. There was no significant difference in fluid balance between the two groups. Likewise, renal tubular obstruction by casts with resulting oliguria is an important reason for ARF [13, 21, 26]. Myoglobin exerts a direct toxic effect by free-radical production and lipid peroxidation, but clinical therapies are not yet available [1, 12, 15]. As cast formation occurs in an acid environment, alkalization of urine by infusion of bicarbonate is the cornerstone of treatment. In clinical practice this axiom is often disregarded, as we observed optimal urine pH in only two patients. This is most probably due to insufficient bicarbonate dosages being used.
Therapy of severe rhabdomyolysis is aimed to prevent both additional muscle injury and ARF. The primary objective in prevention of muscle injury is prompt restoration of blood flow to the ischemic extremity. Fasciotomy was performed in eight patients, followed by amputation in four patients. The main goal to prevent ARF is large volume resuscitation with crystalloids to generate a urine flow of approximately 200 ml/h. Mannitol as osmotic treatment can be useful in the prevention of ARF [1, 17]. In our study, mannitol was infused in six patients but there was no benefit in terms of survival or development of ARF.
In conclusion, we show that in rhabdomyolysis CK values are associated with ARF, as patients with ARF had (1) higher CK values at admission, (2) higher peak CK levels, and (3) slower decline of serum CK levels. The value of CK measurement as a prognostic tool is, nevertheless, limited, given the wide inter-individual range of CK levels.
References
Slater MS, Mullins RJ (1998) Rhabdomyolysis and myoglobinuric renal failure in trauma and surgical patients: a review. J Am Coll Surg 186:693–716
Gabow PA, Kaehny WD, Kelleher SP (1982) The spectrum of rhabdomyolysis. Medicine 61:141–152
Vanholder R, Sever MS, Erek E, Lameire N (2000) Rhabdomyolysis. J Am Nephrol 11:1553–1561
Vanholder R, Sever MS, Erek E, Lameire N (2000) Acute renal failure related to the crush syndrome: towards an era of seismo-nephrology? Nephrol Dial Transplant 15:1517–1521
Bollaert PE, Frisoni A (1999) Epidemiology, mechanisms and clinical features of rhabdomyolysis. Minerva Anestesiol 65:245–249
Visweswaran P, Guntupalli J (1999) Rhabdomyolysis. Crit Care Clin 15:415–428
Betrosian A, Thireos E, Kofinas G, Balla M, Papanikolaou M, Georgiadis G (1999) Bacterial sepsis-induced rhabdomyolysis. Intensive Care Med 25:469–474
Koppel C (1989) Clinical features, pathogenesis and management of drug-induced rhabdomyolysis. Med Toxicol Adverse Drug Experience 4:108–126
Knochel JP (1993) Mechanisms of rhabdomyolysis. Curr Opin Rheumatol 5:725–731
Defraigne JO, Pincemail J (1998) Local and systemic consequences of severe ischemia and reperfusion of the skeletal muscle. Physiopathology and prevention. Acta Chir Belg 4:176–186
Hojs R, Ekart R, Sinkovic A, Hojs-Fabjan T (1999) Rhabdomyolysis and acute renal failure in intensive care unit. Ren Fail 21:675–684
Holt SG, Moore KP (2001) Pathogenesis and treatment of renal dysfunction in rhabdomyolysis. Intensive Care Med 27:803–811
David WS (2000) Myoglobinuria. Neurol Clin 18:215–243
Abassi ZA, Hoffman A, Better OS (1998) Acute renal failure complicating muscle crush injury. Semin Nephrol 18:558–565
Guglielminotti J, Guidet B (1999) Acute renal failure in rhabdomyolysis. Minerva Anestesiol 65:250–255
Nimmo GR, Lambie AT, Cumming AD (1989) Rhabdomyolysis and acute renal failure. Intensive Care Med 15:486–487
Nespoli A, Corso V, Matterel D, Valerio M, Nespoli L (1999) The management of shock and local injury in traumatic rhabdomyolysis. Minerva Anestesiol 65:256–262
Shimazu T, Yoshioka T, Nakata Y, Ishikawa K, Mizishima Y, Morimoto F, Kishi M, Takaoka M, Tanaka H, Iwai A, Hiraide A (1997) Fluid resuscitation and systemic complications in crush syndrome: 14 Hanshin-Awaji earthquake patients. J Trauma 42:641–646
Better OS, Stein JH (1990). Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. N Engl J Med 322:825–829
Schenk MR, Beck DH, Nolte M, Kox WJ (2001) Continuous veno-venous hemofiltration for the immediate management of massive rhabdomyolysis after fulminant malignant hyperthermia in a bodybuilder. Anesthesiology 94:1139–1141
Vivino G, Antonelli M, Moro ML, Cottini F, Conti G, Bufi M, Cannata F, Gasparetto A (1998) Risk factors for acute renal failure in trauma patients. Intensive Care Med 24:808–814
Poels PJE, Gabreels FJM (1993) Rhabdomyolysis: a review of the literature. Clin Neurol Neurosurg 95:175–192
Beetham R (2000) Biochemical investigation of suspected rhabdomyolysis. Ann Clin Biochem 37:581–587
Lofberg M, Tahtela R, Harkonen M, Somer H (1995) Myosin heavy chain fragments and cardiac troponins in the serum in rhabdomyolysis. Diagnostic specificity of new biochemical markers. Arch Neurol 52:1210–1214
Ward MM (1988) Factors predictive of acute renal failure in rhabdomyolysis. Arch Intern Med 148:1553–1557
Splendiani G, Mazzarella V, Cipriani S, Pollicita S, Rodio F, Casciani CU (2001) Dialytic treatment of rhabdomyolysis-induced acute renal failure: our experience. Ren Fail 23:183–191
Author information
Authors and Affiliations
Corresponding author
Additional information
J.P.H. Drenth is an investigator of the Royal Netherlands Academy of Arts and Sciences
Rights and permissions
About this article
Cite this article
de Meijer, A.R., Fikkers, B.G., de Keijzer, M.H. et al. Serum creatine kinase as predictor of clinical course in rhabdomyolysis: a 5-year intensive care survey. Intensive Care Med 29, 1121–1125 (2003). https://doi.org/10.1007/s00134-003-1800-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1800-5