Abstract
Objective
To determine the correlation of blood concentration of lactate and severity of injury and survival in severely injured patients.
Design and setting
A prospective study of severely injured patients admitted directly from an emergency surgical unit to a surgical intensive care unit with an Injury Severity Score (ISS) of 16 points or more. The study was conducted over 30 months.
Patients
98 severely injured subjects aged between 16 and 82 years with ISS range from 16 to 75 points, overall 25.5% mortality.
Interventions
Blood lactate concentrations were measured once on admission, twice daily during the first 2 days and once daily during the next 3 days. ISS, Revised Trauma Score, Shock Index, and Trauma and Injury Severity Score were calculated for each subject.
Measurements and results
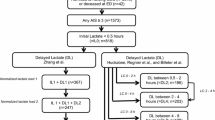
Of 98 severely injured patients 91 had elevated blood lactate concentration (over 2.0 mmol/l). Regression analyses demonstrated that injury severity, as measured by ISS, can be predicted from lactate concentration on admission, while survival, either actual or predicted by Trauma and Injury Severity Score higher than 0.5, can be predicted from lactate concentration after 12 h. We also found that patients with Shock Index higher than 0.9 had significantly higher lactate levels during the first 36 h than those with values less than 0.9.
Conclusions
This study confirmed the relationship between blood lactate levels and injury severity as well as the prognostic value of blood lactate level for survival of severely injured patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mortality in traumatized patients depends to the greatest extent on the mechanism and severity of injury [1]. Hypovolemic shock, the main cause of tissue hypoxia [2], is the predominant characteristic in the majority of severely injured patients who show reduced perfusion and arterial oxygen supply [3]. Maldistribution of perfusion and inadequate tissue oxygenation in the state of compensated shock may lead to multiple organ failure. Monitoring arterial blood lactate concentrations is a method for assessing the degree of tissue hypoxia, especially in injured patients. Inadequate tissue oxygenation is associated with enhanced production of lactate and the resulting increase in blood lactate concentrations [4, 5].
The main advantages of monitoring blood lactate concentrations as an indicator of metabolic derangements include sensitive, accurate information about tissue perfusion and oxygen debt, simple performance and rapid availability of results [6]. Normal arterial blood lactate concentrations range from 0.8 to 2.0 mmol/l [7]. Blood lactate concentrations determined in injured patients on admission to hospital may be an objective indicator of the patient's pre-hospital conditions, and serve as an independent predictor of injury severity, morbidity and mortality [8]. Of course, trauma does not necessarily induce circulatory failure. Since blood pressure may remain normal even in the state of compensated shock associated with inadequate tissue perfusion, the occurrence of circulatory failure is frequently impossible to predict [9]. Blood lactate concentrations return to normal more slowly than blood pressure and heart rate.
The severity of injury can be assessed clinically or using a variety of scores and scales, based either on anatomical criteria or physiological parameters, or a combination of the two. The Abbreviated Injury Scale [9] with its extension, the Injury Severity Score (ISS) [11], is one of the most widely used scoring systems based on the assessment of anatomical injury. The Revised Trauma Score (RTS) measures physiological changes caused by injury and represents a simple triage (T-RTS) and prognostic system [12]. The Trauma and Injury Severity Score (TRISS) combines ISS, prognostic RTS, age of the patient, and mechanism of injury (penetrating or blunt injury) [13]. The Shock Index (SI), i.e., the ratio of heart rate to systolic blood pressure, is not a classical scoring system; it is employed for circulatory function assessment and for triage of injured patients [14]. Elevated SI value indicates acute deterioration in left ventricular mechanical performance, due mostly to changes in the size of the left ventricular stroke work. An SI value of 0.9 or higher can identify most critically ill patients with deterioration in the left ventricular function who have stable vital signs [15].
The purpose of this study was to investigate the relationship between blood lactate levels, injury severity, and probability of survival.
Patients and methods
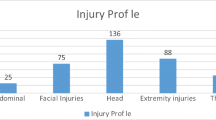
The study was conducted in the Surgical Intensive Care Unit (SICU) of the Department of Anesthesiology and Surgical Intensive Care, Division of Surgery, University Medical Center Ljubljana. We prospectively studied 98 severely injured adults with an ISS of 16 points or higher (75 men, 23 women). All patients enrolled in the study were admitted to the SICU directly from the Surgical Emergency Unit (SEU). The majority of patients were injured in road accidents (75%). Head trauma was present in 75%, and 15 patients in our series died due to severe head injury. Emergency surgery was required in 59 patients (60.2%); in the SEU 57 patients (58.2%) received transfusion of whole blood and/or packed red cells. There were 73 survivors and 25 nonsurvivors. Descriptive statistics are presented in Table 1. Patients who died during first 12 h after the admission to the SICU were excluded from the study. The guidelines of the Declarations of Helsinki (1964) and Tokyo (1975) were strictly adhered to throughout the study. Informed consent was not necessary since determination of blood lactate is a standard procedure. The study was approved by the Medical Ethics Committee of the Ministry of Health of the Republic of Slovenia.
The assessment of injury severity was based on anatomical injury determined by the Abbreviated Injury Scale 90 and ISS, and on the patient's physiological status determined by the T-RTS and prognostic RTS calculations. The values obtained were used for calculating the probability of survival using the TRISS method. The presence of shock on admission to the hospital was determined on the basis of clinical picture in the injured patient (hypotension, systolic blood pressure less the 90 mmHg; tachycardia, pulse frequency higher then 100 beats/min, peripheral vasoconstriction, and altered mental status [16, 17]). SI was calculated for all patients from the first measured RR values and pulse frequency on admission.
The first arterial blood sample for lactate measurements was collected on the patient's admission to the hospital. Blood lactate concentrations were monitored every 12 h within the first 48 h after admission and once daily during the next 3 days. A 2-ml sample was collected in a vacuum tube containing the prescribed amount of sodium fluoride and potassium oxalate. The specimens were analyzed in the Emergency Laboratory of the University Medical Center Ljubljana. Serum lactate concentration was determined using the Kodak analyzer (Vitros 950, Rochester, N.Y., USA). Specimens were centrifuged within 15 min after collection. Vitros LAC slide, a dry, multilayered analytical element coated on a polyester support was used to measure lactate concentrations [18]. A drop of sample was deposited on the slide and the intensity of the dye complex was measured by colorimetric method at 540 ηm wavelength. The results were expressed in mmol/l. Normal values are up to 2.0 mmol/l.
Data were analyzed using SPSS for Windows 10.1 and LogXact-4 statistical software packages. Descriptive statistics were calculated for all investigated parameters. Linear regression was used to predict ISS (log10 transformed) from T-RTS and blood lactate concentration on admission (log10 transformed). Binary logistic regression was used to predict actual survival of patients and survival according to the TRISS higher than 0.5 criterion from blood lactate concentration after 12 h and RTS score. Exact logistic regression was used to assess the relationship between quantity of blood received during treatment in the SICU and survival. Differences in selected numerical parameters between survivors and nonsurvivors, as well as between the two groups based on the SI=0.9 cutoff value, were tested using the exact version of the Mann-Whitney nonparametric test. Fisher's exact test was applied for comparing the percentage of patients showing clinical signs of shock between the two SI groups. p values less than 0.05 were considered statistically significant.
Results
The T-RTS score based on physiological status on admission ranged from 3 to 12 points. In 77 patients (78.6%) the T-RTS was less than 12 points. Patients with a T-RTS of 12 had a significantly lower ISS (25.4±6.5, p<0.01) than those with a T-RTS of 11 or less (33.0±11.3). A clinical picture of shock was present in 46 subjects (46.9%). Twenty-eight of them demonstrated overt signs of protracted shock (profound hypotension, tachycardia, pale and cool skin, confusion). Subsequent measurements revealed that lactate concentration measured in the first blood sample collected on admission was not invariably the highest concentration of lactate determined in individual patients. In some cases peak values were noted at 12 or even 24 h after admission. Blood lactate levels higher than 2.0 mmol/l were recorded in 91 patients (92.8%). Seven patients had normal lactate concentrations throughout the study. All of them were normotensive. Changes in blood lactate concentration within the first 48 h after admission for survivors and nonsurvivors are presented in Fig. 1.
Linear regression analysis confirmed the relationship of blood lactate concentration to injury severity. The model with log10 transformed ISS as dependent variable and T-RTS and log10 transformed blood lactate concentration on admission as independent variables fitted the data well (model p<0.001, adjusted R 2=0.184, all regression diagnostics acceptable). Both predictors proved statistically significant (p=0.041 and p=0.001 for log10 lactate concentration on admission and T-RTS, respectively), whereby their effect was in the opposite direction (standardized regression coefficients: 0.198 for log10 lactate concentration on admission, −0.337 for T-RTS).
When modeling either actual survival of patients or survival according to the TRISS greater than 0.5 criterion, blood lactate concentration on admission did not prove to be a statistically significant predictor. However, lactate concentration after 12 h did provide prognostic information in addition to the RTS score in the logistic regression models predicting survival and TRISS greater than 0.5. Both models fitted the data very well (likelihood-ratio test p<0.001, Hosmer-Lemeshow test p>0.40, Nagelkerke pseudo R 2 >0.40 for both models). These are summarized in Table 2.
There were statistically significant differences between survivors and nonsurvivors concerning ISS, T-RTS, RTS, TRISS, and Glasgow Coma Scale. In the 57 patients treated by transfusion of whole blood or packed red cells the amount of blood transfused was correlated significantly with lactate concentration on admission (r=0.61; p<0.001). Also, a marginally significant association was established between quantity of blood received during treatment in the SEU and survival, whereby the value zero was assigned to patients not receiving transfusion (exact p=0.06).
Regarding the SI elevated lactate levels were found in 58 of the total of 61 patients (95.1%) with SI 0.9 or higher and in 32 of the 37 (86.5%) with SI lower than 0.9. A statistically significant difference was found between the groups regarding the number of patients showing clinical signs of shock (all the 46 patients in the state of shock had SI ≥ 0.9, p<0.001). Blood lactate concentrations in the samples collected within the first 36 h after admission and ISS also differed significantly between the two SI groups.
Discussion
Despite the numerous studies on lactate measurements in critically ill patients there were, a relatively small number of studies investigated the relationship between blood lactate concentration and injury severity [8, 19, 20, 21, 22]. According to some authors, trauma is the disease of younger population groups. Injuries are most frequently sustained in traffic accidents (76%) [23]. As a rule the injured are young and healthy individuals who have no coexisting diseases or severe chronic disorders that would contribute to increased mortality [24]. The age of patients in our study was similar to that mentioned above: 61 patients were aged under 40 years. Unlike other studies, particularly those carried out in the United States [19, 22, 24, 25, 26, 27] mostly reporting on patients with penetrating injuries, the majority of patients in our study had blunt trauma that occurred in road accidents or due to fall from height. Penetrating injuries accounted for only 6% of injuries in our series. Similar data were reported by Frutiger et al. [1] and Manikis et al. [21].
Mortality in our series did not differ notably from that documented in the above studies [1, 21]. Furthermore, Roumen et al. [20] and Manikis et al. [21] found similar ISS values in survivors and nonsurvivors as in our series. Survivors and nonsurvivors also differed significantly in their physiological status assessed by the T-RTS. Although all patients in our series faced severe trauma, as determined on the basis of anatomical criteria (ISS>16), only 77 had a T-RTS of 11 or less, i.e., a score representing severe injury. Gilpin and Nelson [28] explained this difference in their study by the rapid transport of patients from the site of accident to hospital. In our case the two groups differed most notably in their ISS values.
While lactate levels in the group of survivors showed a progressive decline, in nonsurvivors they remained almost unchanged from the 12th h after the first sampling on. A similar change in lactate concentrations was reported by Abramson et al. [18], who noted a transient increase in lactate levels in blood samples collected 8 h after admission to the SICU. Significantly higher lactate levels in nonsurvivors than survivors have been reported in several other studies [20, 21]. Milzman et al. [8] found a clear correlation between increased lactate concentrations, increased ISS, and higher mortality rates. In our study linear regression analysis of blood lactate concentration on admission and injury severity showed that the higher lactate concentrations and lower T-RTS scores on admission are associated with higher ISS values. According to these results, blood lactate concentration on admission is important for prediction of injury severity. A quick analysis of blood lactate specimen combined with T-RTS on admission in the hospital allows a rapid assessment of injury severity without calculating a temporary ISS.
Elevated lactate concentrations are associated with higher mortality, irrespective of the presence of lactic acidosis [29]. The association of elevated lactate levels with higher mortality was also reported by Weil et al. [30, 31]. In our series blood lactate concentration on admission did not demonstrate significant association with patient's actual or predicted survival. However, use of lactate concentration after 12 h instead of lactate on admission in the same statistical model showed that lactate could be a statistically significant predictor. The higher the lactate concentration after 12 h, the lower the probability of survival, actual as well as predicted by the TRISS, controlling for RTS score.
In contrast to anatomical indices that remain unchanged after trauma, physiological status is continually changing [32], partly because of deterioration in the patient's condition and partly due to the effect of therapy. Blood lactate concentrations in those with SI of 0.9 or higher differed significantly from those with SI lower than 0.9 within the first 36 h after admission (i.e., in the first four samples). As soon as lactate levels began to normalize, the difference between the groups was no longer statistically significant. This finding may be due to the effects of therapy but may also be explained by a notably reduced number of patients in the nonsurvivor group 48 h after admission.
Conclusion
Blood lactate levels in severely injured patients are significantly higher among nonsurvivors than among survivors. There is a clear association between lactate concentrations on admission and ISS. According to our findings, the presence of higher values of blood lactate concentrations on admission combined with T-RTS predicts the severity of injury, hence allowing rapid orientation without calculating temporary ISS. Also, blood lactate concentration after 12 h is a good predictor of patient's actual survival and survival according to TRISS greater than 0.5. Patients with a SI value higher than the borderline have higher lactate levels than those with a SI value below the threshold.
References
Frutiger A, Ray C, Bilat C, Rosso R, Furrer R, Cantieni R, Rüedi T, Leutenegger A (1991) Five years' follow-up of severely injured ICU patients. J Trauma 31:1216–1226
Baker J (1999) Blood lactate levels. Curr Opin Crit Care 5:234–239
Kruse JA, Carlson RW (1987) Lactate metabolism. Crit Care Clin 5:725–746
Regel G, Grotz M, Weltner T, Sturm JA, Tscherne H (1996) Pattern of organ failure following severe trauma. World J Surg 20:422–429
Moomey CB, Melton SM, Croce MA, Fabian TC, Proctor KG (1999) Prognostic value of blood lactate, base deficit, and oxygen-derived variables in an LD50 model of penetrating trauma. Crit Care Med 27:154–161
Vitek V, Cowley RA (1991) Blood lactate in the prognosis of various forms of shock. Ann Surg 173:308–313
Bakker J (1996) Monitoring of blood lactate levels. Int J Intensive Care 3:29–39
Milzman D, Boulanger B, Wiles C, Hinson D (1992) Admission lactate predicts injury severity and outcome in trauma patients (abstract). Crit Care Med 21:S94
Sauaia A, Moore FA, Moore EE, Haenel JB, Read RA, Lezotte DC (1994) Early predictors of post injury multiple organ failure. Arch Surg 129:39–45
Association for the Advancement of Automotive Medicine (1990) The Abbreviated Injury Scale. USA
Baker SP, O'Neill B, Haddon W, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Champion HR, Sacco WJ, Copes WS, Gan DS, Gennarelli TA, Flanagan ME (1989) A revision of the Trauma Score. J Trauma 29:623–629
Boyd CR, Tolson MA, Copes WS (1987) Evaluation trauma care: the TRISS method. J Trauma 27:370–378
Rady MY (1992) The role of central venous oximetry, lactic acid concentration and shock index in the evaluation of clinical shock: a review. Resuscitation 24:55–60
Rady MY, Smithline HA, Blake H, Nowak R, Rivers E (1994) A comparison of the shock index and conventional vital signs to identify acute, critical illness in the emergency department. Ann Emerg Med 24:685–690
Committee on Trauma (1993) Advanced trauma life support course for physicians. American College of Surgeons, Chicago, pp 75–94
Martin LC (1997) Primary Triage of the Trauma Patient. In: Kitby RR, Taylor RW, Civetta JM (ed) Handbook of critical care, 2nd edn. Lipincott-Raven, Philadelphia, pp 367–375
Vitros Test Methodologies (1996) Chapter: Lactate. Johnson & Johnson Clinical Diagnostics, Rochester
Abramson D, Scales T, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J (1993) Lactate clearance and survival following injury. J Trauma 35:584–589
Roumen RMH, Redl H, Schlag G, Sandtner W, Koller W, Goris JA (1993) Scoring systems and blood lactate concentrations in relation to the development of adult respiratory distress syndrome and multiple organ failure in severely traumatized patients. J Trauma 35:349–355
Manikis P, Jankowski S, Zhang H, Kahn R, Vincent JL (1995) Correlation of serial blood lactate levels to organ failure and mortality after trauma. Am J Emerg Med 13:619–622
Kremžar B, Špec-Marn A, Kompan L, Cerovic O (1997) Normal values of SvO2 as therapeutic goal in patients with multiples injuries. Intensive Care Med 23:65–70
Sluis CK van der, Klasen HJ, Eisma WH, ten Duis HJ (1996) Major trauma in young and old: What is the difference? J Trauma 40:78–82
Sacco WJ, Copes WS, Bain LW, MacKenzie EJ, Frey CF, Hoyt DB, Weigelt JA, Champion HR (1993) Effect of preinjury illness on trauma patient survival outcome. J Trauma 35:538–543
Peng R, Chang C, Gilmore D, Bongard F (1998) Epidemiology of immediate and early trauma death at an urban level I trauma center. Am Surg 64:950–954
Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD (1980) Epidemiology of trauma deaths. Am J Surg 140:144–150
Cummings P (1990) Cause of death in an emergency department. Am J Emerg Med 8:379–384
Gilpin DA, Nelson PG (1991) Revised trauma score: a triage tool in the accident and emergency department. Injury 22:35–37
Luft D, Deichsel G, Schmülling RM, Stein W, Eggstein M (1983) Definition of clinically relevant lactic acidosis in patients with internal diseases. Am J Clin Pathol 80:484–489
Broder G, Weil MH (1964) Excess lactate: an index of reversibility of shock in human patients. Science 143:1457–1459
Weil MH, Afifi AA (1970) Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation 41:989–1001
Oppenheim WL (1980) Early biochemical changes and severity of injury on man. J Trauma 20:135–140
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cerović, O., Golubović, V., Špec-Marn, A. et al. Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med 29, 1300–1305 (2003). https://doi.org/10.1007/s00134-003-1753-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1753-8