Abstract
Although fluoride induced inflammatory reactions have been shown in animals and in vitro humans, there are few studies about fluoride induced inflammatory reactions in human beings at clinical setting. We aimed to measure the plasma neopterin, a marker of activation of the monocyte/macrophage system, and high sensitivity C-reactive protein (hs-CRP) levels in patients with endemic fluorosis to investigate the possible role of inflammatory processes (monocyte/macrophage activity) in the underlying pathophysiology of fluoride toxicity at clinical level. Plasma neopterin and hs-CRP levels were determined in endemic fluorosis patients and control subjects. Plasma neopterin levels were significantly higher among patients with endemic fluorosis when compared with control group (2.40 ± 0.66 vs. 1.63 ± 0.27 ng/mL respectively; p < 0.001) and plasma hs-CRP levels were also significantly higher among patients with endemic fluorosis when compared with control group (2.41 ± 1.23 vs. 1.93 ± 0.64 mg/L respectively; p < 0.001). Plasma neopterin levels were positively correlated with urine fluoride levels (r = 0.67, p < 0.001) and serum hs-CRP levels were positively correlated with urine fluoride levels (r = 0.36, p < 0.001). We have found that plasma neopterin and hs-CRP levels are increased in patients with endemic fluorosis. We have concluded that inflammation play an important role in the pathophysiology of fluoride toxicity in patients with endemic fluorosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Fluoride is an important environmental pollutants and the main source of fluoride exposure for humans is drinking water. Excessive intake of fluoride leads to chronic fluorosis, dental fluorosis (mottled teeth) and skeletal fluorosis (Ozsvath 2009). Fluorosis is a worldwide health problem and is endemic in some areas where fluoride content is high in drinking water. In our city, Isparta which is located in southwest part of Turkey, fluoride content of natural drinking water is high. As a result, fluorosis is endemic in our city (Oruc 2008). The origin of fluoride was attributed to volcanic rocks in the Golcuk Lake area, located 6 km southwest of the Isparta city centre. Golcuk area consists of sedimentary and volcanic rocks those are tephriphonolite, pyroclastic series and trachyandesite together with trachyite. These volcanic rocks consist of fluoride bearing minerals. These minerals are pyroxene, hornblende, biotite, fluorapatite and glassy groundmass (Oruc 2008). According to Isparta Health Organization data, the mean fluoride level in drinking water was 2.74 ± 064 ppm in the endemic fluorosis region and 0.53 ± 0.06 ppm in the nonendemic region (Varol et al. 2010b).
It has been shown that fluoride induces inflammatory reactions in animals (Cenesiz et al. 2008; Ma et al. 2012; Susheela and Sharma 1981). Fluoride induced inflammatory reactions have also been shown in humans, in vitro (Gutowska et al. 2010, 2011; Salgado-Bustamante et al. 2010) and in vivo (Lund et al. 1999; Susheela and Jethanandani 1994). To the best of our knowledge there is only one study about plasma inflammatory factors in patients with endemic skeletal fluorosis (Susheela and Jethanandani 1994).
Neopterin, a pteridine derivative and a byproduct of the guanosine triphosphate-biopterin pathway, is produced by activated macrophages and is thought to represent an important marker of inflammation, immune activation and macrophage activity (Huber et al. 1984). As far as we know, there is no study about plasma neopterin levels in endemic fluorosis patients.
Accordingly, we aimed to measure the plasma neopterin and high sensitivity C-reactive protein (hs-CRP) levels, an acute phase reactant, at the same time in patients with endemic fluorosis to investigate the possible role of inflammatory processes (monocyte/macrophage activity) in the underlying pathophysiology of fluoride toxicity at clinical level.
Materials and Methods
Seventy-nine patients with endemic fluorosis (35 males/44 females; mean age 44.0 ± 11.9 years) and 55 age, sex and body mass index (BMI) matched healthy controls (23 males/32 females; mean age 47.2 ± 7.5 years) with normal fluoride intake were enrolled in this prospective study. The control subjects were selected from persons who have no dental fluorosis and whose urine fluoride levels are less than 1.5 mg/L. (normal < 1.5 mg/L).
Endemic fluorosis was diagnosed according to the clinical diagnosis criteria, as described by Wang et al. (1994): (1) living in the endemic fluorosis region since birth, (2) having mottled tooth enamel, indicating dental fluorosis, (3) consuming water with fluoride levels above 1.2 mg/L (normal 1 mg/L) and (4) a urine fluoride level greater than 1.5 mg/L. (normal < 1.5 mg/L).
Physical examination was performed in all patients and controls. The patients were also examined for having mottled tooth enamel which is one of the diagnostic criteria of endemic fluorosis. All patients met Wang’s criteria. Body weight and height were recorded and BMI was calculated for each patient as weight (kg)/height (m)2.
None of the patients or control subjects were taking any medications (such as statin) affecting neopterin levels at the time of blood sampling. Hypertension was considered to be present if the systolic blood pressure was >140 mmHg and/or diastolic blood pressure was >90 mmHg or if the individual was taking antihypertensive medications. Diabetes mellitus was defined as a fasting blood glucose level >126 mg/dL or current use of a diet or medication to lower blood glucose. Patients who smoke before study were accepted as smokers.
Patients with coronary artery disease, acute coronary syndromes, previous myocardial infarctions, left ventricular dysfunction, valvular heart disease, renal and hepatic failure, peripheral vascular disease, immunologic or inflammatory diseases, sepsis, active local or systemic infections, a history of recent infection (<3 months before the study), and a history of malignancy were excluded from the study. The study was approved by the institutional ethics committee, and informed consent was obtained from all patients.
Venous blood was collected from the antecubital vein with a 19-gauge needle without venous stasis. Sera of patients and controls were stored at −80 °C. Neopterin levels in serum were determined in a competitive inhibition enzyme-linked immunosorbent assay using a commercial kit (DRG Diagnostics, Marburg, Germany) according to the manufacturer’s instructions. Briefly, 25 μL of undiluted sera and standards were added to the appropriate wells of a 96-well microtiter plate followed by 100 μL enzyme conjugate. The plate was covered with black adhesive foil and incubated at room temperature for 2 h on rotary horizontal shaker (200 rpm). After incubation, the contents of all wells aspirated and the plate was washed three times with phosphate-buffered saline (pH: 7.2) and 200 μL of color substrate (tetramethyl benzidine) was added into the wells as a substrate. Plate was incubated at room temperature for 30 min on a rotary horizontal shaker. The reaction was stopped with 100 μL of 1 mol/L H2SO4. The optical density was read at 450 nm in a micro titer plate reader and calculated the results using the data reduction system. The minimum limit of detection of serum neopterin was 0.2 ng/mL.
hs-CRP was measured using chemiluminescent immunometric assay on IMMULITE 2000 Analyzer (DPC Cirrus Inc, Los Angeles, CA, USA). The analytical sensivity of hs-CRP was 0.1 mg/L.
Urine samples were analyzed for fluoride by using an ion specific electrode (Orion 9609BN ionplus Sure-Flow Fluoride). Serum glucose, creatinine and lipid levels were determined by standard methods.
Data were analyzed with the SPSS software version 10.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous variables from the study groups were reported as mean ± standard deviation, categorical variables as percentages. To compare continuous variables, the Student t test or Mann–Whitney U test were used where appropriate. Categorical variables were compared with the Chi-square test. The correlations between plasma neopterin and hs-CRP levels and urine fluoride levels were performed with Pearson correlation analysis. A p < 0.05 was considered statistically significant.
Results and Discussion
Clinical and laboratory characteristics of fluorosis patients and of the control group are shown in Table 1. Urine fluoride levels of fluorosis patients were significantly higher than control subjects as expected (1.9 ± 0.1 mg/L vs 0.4 ± 0.1 mg/L respectively; p < 0.001). There were no significant differences between fluorosis patients and the controls with respect to age, gender, BMI, systolic and diastolic blood pressure, presence of smoking and the mean serum levels of glucose, creatinine, total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-cholesterol) and high-density lipoprotein-cholesterol (HDL-cholesterol).
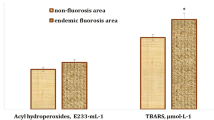
Plasma neopterin levels were significantly higher among patients with endemic fluorosis when compared with control group (2.40 ± 0.66 vs. 1.63 ± 0.27 ng/mL respectively; p < 0.001). Plasma hs-CRP levels were also significantly higher among patients with endemic fluorosis when compared with control group (2.41 ± 1.23 vs. 1.93 ± 0.64 mg/L respectively; p < 0.001). Plasma neopterin levels were positively correlated with urine fluoride levels (r = 0.67, p < 0.001) (Fig. 1) and plasma hs-CRP levels were positively correlated with urine fluoride levels (r = 0.36, p < 0.001) (Fig. 2).
In the present study, we investigated the plasma neopterin and hs-CRP levels in patients with endemic fluorosis. We have found that plasma neopterin and hs-CRP levels are significantly higher in patients with endemic fluorosis when compared with control group. Therefore, we have concluded that inflammation play an important role in pathophysiology of fluoride toxicity in patients with endemic fluorosis.
Recent studies have shown that fluoride accumulates not only in bones and teeth but, to a lesser extent, in soft tissues (Ozsvath 2009). Although various effects of chronic fluorosis on different organ systems have been examined, mechanism and pathophysiology of fluoride toxicity is not still clear.
Fluoride can interact with a wide range of cellular processes such as gene expression, cell cycle, proliferation and migration, respiration, metabolism, ion transport, secretion, endocytosis, apoptosis/necrosis, and oxidative stress, and that these mechanism are involved in a wide variety of signaling pathways (Barbier et al. 2010).
Fluoride exposure has been implicated in inflammation. Although fluoride induced inflammatory reactions have been shown in animals (Cenesiz et al. 2008; Ma et al. 2012; Susheela and Sharma 1981) and in vitro humans (Gutowska et al. 2010, 2011; Salgado-Bustamante et al. 2010), there are few studies about fluoride induced inflammatory reactions in human beings at clinical setting. Lund et al. (1999) have examined the whether experimental hydrogen fluoride exposure for 1 h induces an inflammatory response in the lower respiratory tract that is detectable in bronchoalveolar lavage fluid and they found a significant increase in the percentage of CD3 positive cells, myeloperoxidase and interleukin-6 levels in bronchoalveolar lavage fluid after hydrogen fluoride exposure. In another similar study Lund et al. (2002) have observed an increase in the number of neutrophils and total cells, increase in tumor necrosis factor-alpha, prostaglandin E(2), leukotriene B(4), and peptide leukotrienes in bronchoalveolar lavage after 1 h experimental hydrogen fluoride exposure. They presumed that exposure to hydrogen fluoride induced immediate inflammatory response in respiratory tract in healthy human volunteers. Schwarze et al. (2000) evaluated the inflammatory effect of fluoride exposure on human lung epithelial cells, and they found an increase in the activity of interleukin-8. Cenesiz et al. reported that fluoride toxicity caused increased inflammatory markers, C-reactive protein (CRP) and adenosine deaminase in rabbit sera. Susheela et al. (1981) reported that fibrinogen, an acute phase protein was raised in the sera of rabbits treated with sodium fluoride.
To the best of our knowledge there is only one study about serum inflammatory factors in patients with endemic skeletal fluorosis (Susheela and Jethanandani 1994). In this study, Susheela et al. studied the circulating levels of haptoglobin and CRP in patients with skeletal fluorosis and compared them with controls. They found a significant increase in the serum levels of haptoglobin and CRP as well as a raised erythrocyte sedimentation rate in patients with skeletal fluorosis when compared to controls. They suggested that subclinical inflammatory reaction is present in patients with skeletal fluorosis.
In our study, we have examined the hs-CRP that is more sensitive marker of inflammation as compared to CRP and we have found increased hs-CRP levels in patients with endemic fluorosis for the first time. Our results show that chronic low grade subclinical inflammation is present in endemic fluorosis patients. Our results confirm the previous studies.
Neopterin is produced by activated macrophages and is thought to represent an important marker of inflammation, immune activation and macrophage activity (Huber et al. 1984, Murr et al. 2002). In our study, we have also examined the plasma neopterin levels, a marker of activation of the monocyte/macrophage system, in patients with endemic fluorosis to show the possible role of inflammatory processes (monocyte/macrophage activity) in the underlying pathophysiology of fluoride toxicity at clinical setting. We have found an increased neopterin levels in patients with endemic fluorosis for the first time. In humans, increased neopterin concentrations have been reported in bacterial, viral and parasitic infections, autoimmune diseases, malignant tumors, during rejection episodes in allograft recipients and chronic inflammatory processes (Murr et al. 2002; Fuchs et al. 1992; Ariyarajah 2008). Increased serum neopterin levels have also been observed in various cardiovascular diseases in which inflammation play an integral role (Schumacher et al. 1997; Varol et al. 2011; Sahin et al. 2008). To the best of our knowledge, there is no study about role of neopterin, a novel marker of activation of the monocyte/macrophage system in fluoride toxicity.
The mechanism of increase in neopterin levels is not clear and also complex process. Gutowska et al. (2010) examined the effect of fluoride, at concentrations determined in blood of persons environmentally exposed to fluorides, on the intracellular production of reactive oxygen species (ROS), apoptosis process and synthesis of ATP in macrophages. The incubation of macrophages in fluoride solutions significantly decreased the amount of synthesized cellular ATP and increased formation of ROS and apoptosis in a dose-dependent manner and they speculated that fluoride probably promotes oxidative stress in macrophages, which is manifested by a strong increase in ROS synthesis and a decrease in ATP. Fluoride can induce oxidative stress in macrophages and this in turn can stimulate macrophages to secrete more neopterin. Several lines of evidence confirm that pro-inflammatory cascades and oxidative stress are strongly involved in fluoride toxicity (Barbier et al. 2010). In another study, Gutowska et al. (2011) demonstrated that fluoride increased the concentration of prostaglandin E2 and thromboxane B2 (stable derivative of thromboxane A2) in peripheral blood mononuclear macrophages in a dosage dependent manner. They suggested that fluoride, even in small concentrations, might induce an inflammatory process and apoptotic effect in peripheral blood mononuclear macrophages through the stimulation of prostanoids metabolism and increased synthesis of prostaglandin E2 and thromboxane A2. In one study, fluoride exposure induced the expression of apoptosis and inflammatory genes in peripheral blood mononuclear cells (Salgado-Bustamante et al. 2010). Recently, Ma et al. (2012) reported that fluoride and arsenic alone or combined increased the expression of vascular cell adhesion molecule-1, P-selectin monocyte chemotactic protein-1, interleukin-8 and interleukin-6 at the RNA and protein levels in rabbit aorta. They suggested that fluoride exposure induce inflammatory reactions in rabbit aorta. These molecules play an important role on the adhesion of monocytes and subsequent migration to activated arterial endothelium, which is an initial event in the pathogenesis of atherosclerosis (Libby 2002). As a result, increased expression of inflammatory genes might cause an increase in plasma inflammatory markers in endemic fluorosis patients. It must be emphasized that fluoride has a special effect on macrophages and macrophages have ability to uptake and accumulate fluoride, which may stimulate processes leading to the conversion of macrophages into foam cells forming the atherosclerotic plaque (Gutowska et al. 2010). Interestingly, in our previous study, we have found that elastic properties of ascending aorta are impaired in patients with endemic chronic fluorosis (Varol et al. 2010b). In other words aortic stiffness which is associated with atherosclerosis was found to be increased in patients with endemic chronic fluorosis in this study. In our second study, we have shown that chronic fluorosis patients have left ventricular diastolic and global dysfunctions (Varol et al. 2010a). We have presumed that these results are due to inflammation and oxidative stress induced by fluoride toxicity. As we know, inflammatory reactions underlie the pathogenesis of the atherosclerotic process (Libby 2002).
Inflammation is the first response of the immune system to infection or tissue damage to protect the human body against these insults. However, chronic inflammation is harmful and has an important role in the development of several chronic diseases such as atherosclerosis and diabetes mellitus (Libby 2002). Inflammation can be triggered by a chronic excess of neurotransmitters and/or metabolic factors, such as cytokines, lipids, and glucose. Also environmental factors like air pollution, drinking water pollution can trigger inflammation (Barbier et al. 2010). As we mentioned above, long term consumption of drinking water with high fluoride concent can trigger inflammation in patients with endemic fluorosis. This in turn, can cause chronic cardiovascular and metabolic disorders.
It has also been shown that, fluoride toxicity can cause impaired glucose tolerance (García-Montalvo et al. 2009). Impaired glucose tolerance is also associated with inflammation (Wolf et al. 2004). As a result fluoride toxicity can cause inflammatory response in endemic fluorosis patients and this in turn can cause cardiovascular and metabolic disorders in long term.
There are some limitations of this study that should be noted. Firstly, our sample size was small. Another limitation of this study is that analysis was based on a simple baseline determination that may not reflect the patient status over long periods.
The results of our study demonstrate that serum neopterin and hs-CRP levels are significantly elevated in patients with endemic fluorosis when compared with control subjects. This study shows that low-grade, chronic inflammation exists in endemic fluorosis patients. This low-grade inflammation can cause many chronic diseases like cardiovascular and metabolic diseases in long term period. Consequently, our data contribute to the concept that induction of inflammatory responses may play an important role in the mechanism of the cardiovascular and metabolic toxicity of fluoride.
References
Ariyarajah V (2008) Neopterin: ıts role in ınflammation and coronary heart disease. South Med J 101(5):461–463
Barbier O, Arreola-Mendoza L, Del Razo LM (2010) Molecular mechanisms of fluoride toxicity. Chem Biol Interact 188:319–333
Cenesiz S, Yarim GF, Nisbet C, Ciftci G (2008) Effects of fluoride on C-reactive protein, adenosine deaminase, and ceruloplasmin in rabbit sera. Fluoride 41:52–56
Fuchs D, Weiss G, Reibnegger G, Wachter H (1992) The role of neopterin as a monitor of cellular immune activation in transplantation; inflammatory; infectious and malignant diseases. Crit Rev Clin Lab Sci 29:307–341
García-Montalvo EA, Reyes-Pérez H, Del Razo LM (2009) Fluoride exposure impairs glucose tolerance via decreased insulin expression and oxidative stress. Toxicology 263(2–3):75–83
Gutowska I, Baranowska-Bosiacka I, Baskiewicz M, Milo B, Siennicka A, Marchlewicz M, Wiszniewska B, Machaliński B, Stachowska E (2010) Fluoride as a pro-inflammatory factor and inhibitor of ATP bioavailability in differentiated human THP1 monocytic cells. Toxicol Lett 196:74–79
Gutowska I, Baranowska-Bosiacka I, Siennicka A, Baśkiewicz M, Machaliński B, Stachowska E, Chlubek D (2011) Fluoride and generation of pro-inflammatory factors in human macrophages. Fluoride 44:125–134
Huber C, Batchelor JR, Fuchs D, Hausen A, Lang A, Niederwieser D, Reibnegger G, Swetly P, Troppmair J, Wachter H (1984) Immune response-associated production of neopterin. Release from macrophages primarily under control of interferon-gamma. J Exp Med 160:310–316
Libby P (2002) Inflammation in atherosclerosis. Nature 420:868–874
Lund K, Refsnes M, Sandstrom T, Sostrand P, Schwarze P, Boe J, Kongerud J (1999) Increased CD3 positive cells in bronchoalveolar lavage fluid after hydrogen fluoride inhalation. Scand J Work Environ Health 25:326–334
Lund K, Refsnes M, Ramis I, Dunster C, Boe J, Schwarze PE, Skovlund E, Kelly FJ, Kongerud J (2002) Human exposure to hydrogen fluoride induces acute neutrophilic, eicosanoid, and antioxidant changes in nasal lavage fluid. Inhal Toxicol 14:119–132
Ma Y, Niu R, Sun Z, Wang J, Luo G, Zhang J (2012) Inflammatory responses induced by fluoride and arsenic at toxic concentration in rabbit aorta. Arch Toxicol Mar 16. [Epub ahead of print]
Murr C, Widner B, Wirleitner B, Fuchs D (2002) Neopterin as a marker for immune system activation. Curr Drug Metab 3:175–187
Oruc N (2008) Occurrence and problems of high fluoride waters in Turkey: an overview. Environ Geochem Health 30:315–323
Ozsvath DL (2009) Fluoride and environmental health: a review. Rev Environ Sci Biotechnol 8:59–79
Sahin M, Varol E, Ozaydin M, Altinbas A, Aydin O, Aslan SM, Dogan A, Kaya S (2008) Comparison of neopterin levels in patients with coronary artery ectasia versus patients with obstructive coronary artery disease. South Med J 101:476–479
Salgado-Bustamante M, Ortiz-Perez MD, Calderon-Aranda E, Estrada-Capetillo L, Nino-Moreno P, Gonzalez-Amaro R, Portales-Pérez D (2010) Pattern of expression of apoptosis and inflammatory genes in humans exposed to arsenic and/or fluoride. Sci Total Environ 408:760–767
Schumacher M, Halwachs G, Tatzber F, Fruhwald FM, Zweiker R, Watzinger N, Eber B, Wilders-Truschnig M, Esterbauer H, Klein W (1997) Increased neopterin in patients with chronic and acute coronary syndromes. JAmColl Cardiol 30:703–707
Schwarze PE, Lag M, Becher R, Thrane EV, Samuelsen JT, Hetland RB, Refsnes M (2000) Role of signal transduction pathways in lung inflammatory responses. Toxicol Lett 112–113:165–170
Susheela AK, Jethanandani P (1994) Serum haptoglobin and C-reactive protein in human skeletal fluorosis. Clin Biochem 27:463–468
Susheela AK, Sharma YD (1981) Chemical profile of blood in fluoride toxicity. III. Plasma fibrinogen levels in rabbit. Toxicol Eur Res 3:105–107
Varol E, Akcay S, Ersoy IH, Koroglu BK, Varol S (2010a) Impact of chronic fluorosis on left ventricular diastolic and global functions. Sci Total Environ 408:2295–2298
Varol E, Akcay S, Ersoy IH, Ozaydin M, Koroglu BK, Varol S (2010b) Aortic elasticity is impaired in patients with endemic fluorosis. Biol Trace Elem Res 133:121–127
Varol E, Gulcan M, Aylak F, Ozaydın M, Sütçü R, Erdoğan D, Doğan A (2011) Increased neopterin levels and its association with angiographic variables in patients with slow coronary flow: an observational study. Anadolu Kardiyol Derg 11:692–697
Wang Y, Yin Y, Gilula LA, Wilson AJ (1994) Endemic fluorosis of the skeleton: radiographic features in 127 patients. AJR Am J Roentgenol 162:93–98
Wolf M, Sauk J, Shah A, Vossen Smirnakis K, Jimenez-Kimble R, Ecker JL, Thadhani R (2004) Inflammation and glucose intolerance: a prospective study of gestational diabetes mellitus. Diabetes Care 27(1):21–27
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varol, E., Aksoy, F., Icli, A. et al. Increased Plasma Neopterin and hs-CRP Levels in Patients with Endemic Fluorosis. Bull Environ Contam Toxicol 89, 931–936 (2012). https://doi.org/10.1007/s00128-012-0801-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00128-012-0801-x