Abstract
Purpose
Research has produced inconsistent results with respect to whether the association between psychotic experiences and suicidal behavior is independent of co-occurring clinical and socioenvironmental factors, despite substantial evidence linking the two phenomena. This study tests whether a comprehensive set of demographic, socioenvironmental, and clinical variables account for the statistical association between psychotic experiences and suicidal behaviors.
Methods
We utilized blocked multivariable logistic regression models to analyze the association between 12-month psychotic experiences and 12-month suicide behaviors (ideation, plan, and attempt) on a subsample (N = 2307) of the National Comorbidity Survey Replication. The models adjusted for socio-demographic characteristics, environmental factors in the form of childhood adversity, mental health service utilization, and psychiatric and substance abuse disorders.
Results
Psychotic experiences were significantly associated with suicidal ideation, even after adjusting for socio-demographics, childhood adversity. However, the significant association between psychotic experiences and suicidal ideation was not robust to the inclusion of mental health service utilization and psychiatric disorders. There was no significant association between psychotic experiences and suicide plan. Psychotic experiences were associated with a significantly increased risk of reporting suicide attempts (OR 6.52; 95% CI 1.36–31.11), even after adjusting for the full set of variables.
Conclusions
Although psychotic experiences were not associated with suicidal ideation after statistical adjustments, psychotic experiences were associated with a significantly increased risk of suicide attempts after the inclusion of common risk factors and co-morbidities. Thus, psychotic experiences should be included in routine psychiatric assessments to identify the individuals most at risk for attempting suicide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is now substantial evidence linking psychotic experiences to suicidal ideation and behavior, showing that the well-established elevated risk for suicide associated with schizophrenia [7, 14] persists along the psychosis continuum [24] and applies to sub-threshold psychotic experiences [10, 12, 13, 34]. This raises the possibility that screening for psychotic experiences may improve our ability to predict risk for suicidal behavior, although translation of this epidemiological research into clinical practice would benefit from the further exploration the role of co-occurring factors.
Psychotic experiences and suicidal behavior both tend to arise in the context of significant psychological distress and amidst histories of trauma and severe stress [31], and also may be directly related. The majority of recent research on psychotic experiences and suicide suggest that psychotic experiences precede either the onset or exacerbation of suicidal behavior and therefore may serve as a marker of subsequent risk, and they have indeed been linked to incident suicidal behavior [2, 16, 17, 26, 34]. This hypothesis parallels common explanations for the elevated risk of suicide in schizophrenia, which presume that the illness itself (rather than other co-occurring factors) leads to suicidal ideation and behavior.
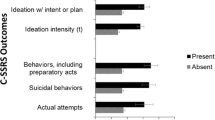
It has alternatively been proposed that psychotic experiences may be an adaptive response to the extreme distress of having significant suicidal thoughts, in that they serve to externalize thoughts or behaviors that when internalized would manifest as self-harm; this comparably less-tested “suicidal drive hypothesis” has been supported by some retrospective epidemiological evidence [27]. Either of these causal pathways could potentially be directly translated into interventions that could contribute to the alleviation of risk for psychosis or suicide as illustrated (Fig. 1), based on common underlying constructs identified in a previous review [11].
Conceptual model of the potential associations between psychotic experiences, suicidal outcomes, and their shared risk factors. The direct links between psychotic experiences and each aspect of suicidal behavior, labelled A, B, and C, are tested through progressively adjusted hierarchical models. Direct effects are considered present when the association between psychotic experiences and suicidal ideation (pathway A), suicide plans (pathway B), and suicide attempts (pathway C) remain statistically significant in the fully adjusted models
However, a third possibility is that the association between psychotic experiences and suicide is indirect and better explained by co-occurring factors In this scenario, psychotic experiences and suicide may both be transdiagnostic indicators of severe psychological distress that arise in the context of extensive trauma or other forms of psychosocial vulnerability and adversity [6]. There have been attempts to test whether shared underlying risk factors explain the co-occurrence of psychotic experiences and suicide, and a recent review concluded that factors such as comorbid psychiatric disorders and socioenvironmental exposures explained a substantial amount of the associations between psychotic experiences and suicidal behavior [10]. Many of the factors that had been included in the reviewed studies had previously been linked to suicide risk based on the interpersonal theory and three-step theory of suicide [23, 33]. The reviewed studies varied widely in terms of exposure and outcome measures, settings and demographics of participants, and adjustment factors, but the main associations between psychotic experiences and suicide-related outcomes generally remained significant although attenuated following adjustment. However, studies with the most extensive adjustments notably found either a substantial reduction in point estimates [28] or in some cases a complete statistical elimination of the main effects [3, 6].
Given the mixed results in the prior literature and methodological inconsistencies across reviewed studies, we herein attempt to test the confounding hypothesis in (1) a representative probability sample (2) using contemporaneous (12-month) measurement of psychotic experiences and suicide-related outcomes, (3) with adjustments and considerations for all categories of potential confounders and mediators previously identified [10]. The association between psychotic experiences and suicidal ideation and behavior has previously been described in these data [5]. Therefore, the aims of this study were to further explore the associations between psychotic experiences and suicidal ideation, suicide plans, and suicide attempts, with and without a full set of adjustments, to determine whether these associations are better conceptualized as direct independent relationship, or if they are better explained by co-occurring psychological, social, clinical, and demographic factors.
Methods
Sample
We analyzed data from the National Comorbidity Survey Replication (NCS-R; [21]). The face-to-face survey was conducted between 2001 and 2002, and used multi-stage probability sampling strategies to achieve US nationally representative samples of adults in the general population of the 48 contiguous states. The NCS-R contains 9090 adults (over the age of 17) who completed ‘Part 1’ of the survey, which included measures of DSM-IV psychiatric disorders. All respondents who screened positive for psychiatric disorders were administered ‘Part 2’ of the survey, as did an additional probability subsample of other Part 1 respondents. A total subsample of 5554 respondents completed Part 2, and a random subsample (n = 2313) of these individuals completed the psychosis screen. Individuals who self-reported having received a diagnosis of schizophrenia from a medical professional (n = 5) were excluded from the analyses. Recruitment and consent procedures were approved by the institutional review boards of both Harvard University and the University of Michigan.
Measures
Suicidal ideation and behavior (dependent variables)
In 81.4% of the sample, suicidality was assessed through a written self-report module for respondents literate in English, which helps mitigate the influence of social desirability bias. Another 17.4% of the sample was asked the suicidality questions in face-to-face interviews in the respondents’ primary language. These responses were collapsed into the suicidality variables. In this paper, suicidality refers to three separate variables: suicidal ideation, suicide plans, and suicide attempts. Respondents reported (yes/no) whether they had ever seriously thought about suicide over the past 12 months; if yes, respondents were then asked (yes/no) if they had made a plan, and (yes/no) if they had made an attempt in the past 12 months.
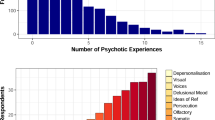
Psychotic experiences (independent variable)
Psychotic experiences were assessed using the WHO World Mental Health-Composite International Diagnostic Interview (WMH-CIDI) 3.0 Psychosis Screen [22], which is a validated diagnostic instrument for mental disorders. It has been used in World Mental Health Surveys for assessment of psychotic experiences (see Kaymaz et al. 2012; McGrath et al., 2015). Respondents were asked to report the lifetime occurrence of six psychotic experiences, including: (1) visual hallucinations, (2) auditory hallucinations, (3) thought insertion, (4) thought control, (5) telepathy, and (6) delusions of persecution. Endorsing at least one of these experiences constituted a positive endorsement of lifetime psychotic experiences. Responses were not considered a psychotic experience when occurring in the context of falling asleep, dreaming, or substance use. Individuals who responded ‘yes’ to any of the aforementioned experiences were asked if the experiences occurred over the past 12 months. The binary indicator of 12-month psychotic experiences was used as the primary exposure variable of the study.
Potential confounder and mediator variables
Potential confounders and mediators were identified and grouped based on the seven categories recently identified in a systematic review of prior research on the association between psychosis and suicide [10]. Confounders included factors such as demographics, environmental factors of neglect and abuse, and family history of mental illness, which likely predate the 12-month assessment period of the primary exposure and outcome variables. Potential mediators (which in some cases may be better conceptualized as confounders, although this cannot be distinguished in our cross-sectional data) included concurrent psychiatric disorders, concurrent alcohol and substance use, service utilization, and psychological factors. Mediators and confounders are detailed by sub-category, below.
Socio-demographic characteristics
All models were adjusted for age (continuous), sex (male, female), race (white, black, Latino, Asian, other), income (poor, near poor, non-poor according to the federal poverty line), education (less than high school, high school graduate, some college, college graduate and beyond), and immigration status (foreign born vs. native born).
Psychiatric disorders
Twelve-month psychiatric disorders were based on the WMH-CIDI [11], which is a fully structured lay interview to screen for diagnoses according to DSM-IV criteria. Respondents were coded as ‘yes’ if they had at least one of the following psychiatric disorders at some point in the 12 months prior to the survey’s administration: mood disorder (dysthymia, depressive episode, major depressive disorder, bipolar I, bipolar II), anxiety disorder (agoraphobia with and without panic disorder, generalized anxiety disorder, panic attacks, panic disorder, post-traumatic stress disorder, social phobia), and eating disorders (anorexia, bulimia, binge eating).
Alcohol and substance use
Twelve-month substance use disorders were diagnosed in accordance with the WMH-CIDI. Respondents were coded as ‘yes’ if reporting 12-month alcohol and/or substance use (DSM-IV drug abuse and dependence) disorder(s).
Environmental factors
Environmental factors were measured in four different ways: (1) five variables measuring frequency of childhood neglect; (2) one variable measuring frequency of physical abuse; (3) one measure indicating childhood poverty; (4) and one measure indicating household instability. All of these measures were included as indicators of childhood adversity in previous studies using NCS-R data (see [19]). The neglect variables were measured using five items, all of which were recorded on a four-point ordinal scale that included the following responses: never, rarely, sometimes, and often. Respondents rated the frequency they went hungry (“How often did your parents or your caregivers make you go hungry or not prepare regular meals?”),went without things (“How often did you go without things you needed like clothes, shoes, or school supplies because your parents or caregivers spent money on themselves?”); went unsupervised (“How often were you left alone or unsupervised when you were too young to be alone?”); went without proper medical care (“How often did your parents fail to get you treatment when you were sick or hurt?”); and were overburdened with chores (“How often were you made to do chores that were too difficult or dangerous for someone your age?”). Physical abuse was measured using an ordinal item capturing frequency of abuse (often, sometimes, rarely, and never), (“When you were growing up, how often did someone in your household do any of the following things to you [“pushed, grabbed or shoved”, “threw something”, and “slapped or hit”]?”). For childhood poverty, respondents were asked (yes/no) whether their families received government assistance (e.g., “welfare, Aid to Families with Dependent Children, General Assistance, or Temporary Assistance for Needy Families”) for six or more months during their childhood and adolescence, serving as the proxy for childhood poverty. For housing instability, respondents were asked (yes/no), “Up until you were sixteen, were you ever away from home for 6 months or longer—either in foster care, with other relatives, in a boarding school, hospital, juvenile detention center, or elsewhere?” Respondents were coded as ‘no’ if they “returned home on weekends” or for other occasions during the separation period.
Psychological factors
Psychological distress was measured using the K-6, a global measure of nonspecific psychological distress that accurately and efficiently predicts the presence of serious mental illness, where serious mental illness was defined as any 12-month DSM-IV disorder, excluding substance abuse disorders [20]. Participants responded to six items of psychological distress during 1 month in the previous 12 months when they were “at [their] worst emotionally in terms of being anxious, depressed, or emotionally stressed”. The K-6 was not included in our final models as it was not administered to the entire sample (approximately, 60% of the NCS-R subsample that completed the psychosis screen responded to the K-6 items), but is included as an independent variable in our Supplemental Results (Table S2).
Service utilization
Respondents reported the number of times they used any of the following six mental health services in the “past year” or “past 12 months”: a hotline, psychologist, psychiatrist, social worker, counselor, and other professionals. Each variable was recoded into a dichotomous measure by being coded as ‘yes’ if a respondent used a service at least once and ‘no’ if a respondent reported no utilization. The six dichotomous variables were aggregated into a new binary variable that was coded as ‘yes’ if any of the six mental health services was used and ‘no’ if none of the services was used.
Family history
Parental mental health problem was measured using the dichotomous item that identified individuals who had at least one parent who experienced depression, anxiety, alcohol/substance abuse, and/or suicide attempt. Family history was not included in our final models as it was not administered to the entire sample (approximately 83% of the NCS-R subsample that completed the psychosis screen responded to the questions regarding parents’ mental health histories), and was previously shown to have limited value in explaining the association between psychosis and suicide [10, 11], but is included as an independent variable in our Supplemental Results.
Data analysis
Using blocked multivariable logistic regression, we examined the associations between psychotic experiences and suicidality (ideation, plans, attempts), using separate models for each outcome, with additional sets of predictive variables added at each block. Socio-demographic characteristics were included in the first block and all subsequent blocks, childhood adversity variables were included in the second block, mental health service utilization was included in the third block, and 12-month psychiatric and substance abuse disorders were included in the fourth block. Standard errors were estimated through design-based analyses that used the Taylor series linearization method to account for the complex multistage clustered design, with US metropolitan statistical areas or counties as the primary sampling units. Sampling weights were used for all statistical analyses to account for individual-level sampling factors (i.e., non-response and unequal probabilities of selection). Estimation of variance inflation factors (VIFs) for the childhood adversity variables assuaged concerns of multicollinearity. The highest VIF was 1.96 (childhood hunger) and the mean VIF across all childhood adversity variables was 1.46. All analyses were performed using STATA SE 15. Findings were presented as odds ratios (OR) with 95% confidence intervals (95% CI).
Results
The sample was weighted to be nationally representative of US households, using the provided NCS-R survey weights (for demographics, see Table S1, Online Supplement). The survey-weighted prevalence of 12-month suicidal ideation for the analytic sample was 2.23%, whereas the prevalences for 12-month suicide plan and suicide attempt were 0.53% and 0.49%, respectively. Approximately, 2.97% of respondents reported experiencing a 12-month psychotic experience. The prevalence for 12-month psychiatric disorders was relatively higher, with 20.96% of respondents reporting at least one psychiatric disorder and 3.17% of respondents reporting a 12-month substance use disorder. Although nearly a quarter of the sample reported a 12-month psychiatric or substance use disorder, only 7.66% of respondents reported utilizing formal mental health services in the same time period (Table 1).
Reporting psychotic experiences in the past 12 months was associated with nearly a four times greater odds of reporting suicidal ideation in the past 12 months when controlling for socio-demographic characteristics. However, the association was no longer significant after adjusting for childhood adversities, mental health service utilization, 12-month psychiatric disorders, and substance use disorders (Table 2). Psychotic experiences were not significantly associated with reporting a suicide plan in the previous 12 months in any of the specifications, including the demographically adjusted model, although this may be due to type II error given the low prevalence of plans (Table 3). Psychotic experiences were associated with approximately nine times greater odds of reporting a suicide attempt in the past 12 months when adjusting for socio-demographic characteristics. The significantly greater risk of a suicide attempt in the past 12 months for those who reported psychotic experiences remained significant after adjusting for childhood adversities, mental health utilization, and 12-month substance use disorders (Table 4).
The supplemental analyses examined the impact of the K-6 psychological distress scale and family mental health history on the association between 12-month psychotic experiences and 12-month suicide behaviors. The sample size reduction (n = 1644) when including both the K-6 and family history into the fully adjusted models was too large to produce meaningful estimates when the outcomes were 12-month suicide plan and suicide attempt. Therefore, the two variables were included simultaneously for the 12-month suicidal ideation model and separately for the 12-month suicide plan and attempt models. The association between 12-month psychotic experiences and suicidal ideation did not appreciably change in magnitude or statistical significance with the inclusion of the K-6 and family history variable (OR 2.20; 95% CI 0.45–10.72). The same was true when suicide plan was the outcome. In contrast, 12-month psychotic experiences were associated with approximately nine times the odds of reporting a 12-month suicide attempt in the fully adjusted models (OR 8.80; 95% CI 1.03–75.01; p < 0.05), even after the inclusion of the K-6, which itself was significantly associated with suicide attempts (OR 1.64; 95% CI 1.32–2.04, p < 0.01). The association between 12-month psychotic experiences and 12-month suicide attempts was no longer significant after the inclusion of family history, although the sample size fell from 2066 to 1586 and family history was independently weakly associated with suicide attempts.
Discussion
Psychotic experiences were associated with all indicators of suicidal ideation and attempts in the demographically adjusted analyses, but these associations were variably attenuated when adjusting for shared underlying factors and concurrent psychiatric disorders. The relationship between psychotic experiences and suicidal ideation was partially explained by childhood history of physical abuse (Model 2), but was primarily explained (and rendered statistically insignificant) by inclusion of concurrent psychiatric disorders and formal treatment in the model (Model 4). Alternatively, associations between psychotic experiences and suicide attempts were only minimally attenuated with adjustments, including adjustment for concurrent psychiatric treatment and substance disorders (which themselves were independently related to attempts).
Unlike ideation and attempts, suicide plans were not significantly associated with psychotic experiences in any of the models, although there were only a small number of participants who reported making a plan (n = 19, demographically adjusted OR 3.41), suggestive of a type II error. The association between psychotic experiences and plans seemed to instead be better explained by childhood poverty, neglect, and concurrent psychiatric conditions. Notably, however, confidence intervals were wide due to the relatively low prevalence of suicidal behaviors, and include the possibility of very large or very small effects, despite this lack of statistical significance based on traditional p values (see [1]). For example, the 95% confidence interval for suicide plans includes the possibility of plans being anywhere from tenfold less likely to tenfold more likely among respondents reporting psychotic experiences.
Psychotic experiences and suicide attempts
Psychotic experiences were associated with more than sixfold greater odds of making at least one suicide attempt during the concurrent 12-month period in these data, even after adjusting for an extensive and conservative set of potential confounding and mediating variables (see Table 4). This finding is consistent with prior evidence that psychotic experiences may be particularly indicative of those at increased risk of suicide attempts, based on evidence that (1) they can significantly differentiate individuals with ideation alone from those who act on that ideation with a suicide attempt, and that (2) psychotic experiences may not be associated with suicidal ideation when people who make attempts are excluded [5, 6, 18]. It is not clear why psychotic experiences are associated with suicide attempts but not suicidal ideation, although this has notably been shown in multiple prior general population and clinical samples [5, 6, 17, 18], suggesting that psychotic experiences may be particularly predictive of more severe suicidal behavior, with ideation better explained by co-occurring depressive or anxiety symptoms. A prior study of Australian adolescents likewise found that the association between 12-month psychotic experiences and suicide attempts remained significant following adjustment with a similarly extensive set of potential confounders [11]. Meta-analysis has further confirmed that the magnitude of association between psychotic experiences and suicide attempts tends to be greater than that of suicidal ideation [34]. Together, this supports the role of screening for psychotic experiences to identify those at increased risk of suicide attempts. Similarly, schizophrenia-spectrum psychotic disorders have been linked to greater severity of suicide attempts and greater associated intent to die [15, 29].
The role of mediators and confounders
This study built upon the recent systematic review of factors linking sub-clinical psychosis to self-injurious thoughts and behavior [10], incorporating indicators of each potential confounder and mediator identified in that review into our statistical models (or in the case of family history and psychological distress, in the Supplemental Analysis Materials). The most important factors appear to be concurrent psychiatric diagnoses and service utilization, which is perhaps unsurprising given that psychotic experiences and suicidal behavior both seem to be transdiagnostic indicators of the severity of underlying psychopathology. This in itself may be a primary reason for their common co-occurrence at both the clinical and sub-clinical range. A study of Australian adolescents using a similar approach of hierarchical adjustments likewise found comorbidities (specifically depression) and service utilization to be the variables with the greater explanatory power [11]. Notably, suicide risk has been shown to persist or reemerge among people with schizophrenia, even when psychotic symptoms are adequately managed, suggesting that it may be factors other than psychotic symptoms themselves that are driving this risk [32].
Interestingly, the impact of the socioenvironmental exposures (which were tested without inclusion of co-morbidities and service utilization in Model 2 for each outcome) was comparably marginal. Individual neglect indicators were associated with suicide plans and attempts, and physical abuse exposure was associated with suicide ideation, but these factors did not substantially reduce the odds ratios of the main independent-dependent association for any of the three suicidal outcomes.
Taken together, the pattern of significant confounder and mediator variables suggests that both psychotic experiences and suicide-related outcomes are indicators of significant underlying mental health difficulties, but we cannot conclusively determine the role of the social environment in driving this expression, as had been previously suggested in a high-functioning college student sample [5, 6]. We also cannot conclusively say whether the relationship between PE and suicide attempts is directly casual or partially (or fully) mediated by relevant variables, although the strength of the association in the current study (OR > 6 after adjustment) is indicative of a strong and independent relationship for suicide attempts.
Limitations
The findings from this study should be interpreted bearing in mind a number of potential limitations. First, the data were cross-sectional and thus did not allow us to assess temporal order of exposures, outcomes, and covariates. Many of the childhood adversities temporally preceded the current manifestations of symptoms, though we cannot be entirely certain that the age at which these childhood adversities first occurred preceded the onset of symptoms. Longitudinal studies (with path analyses) are needed to better understand the risk and protective factors of people with psychotic experiences who go on to attempt suicide. Eliciting information from adult respondents about their experiences in childhood also makes their responses subject to recall bias. The use of 12-month (rather than lifetime) psychotic experiences likely reduced the threat of recall bias for the primary exposure, although this also precluded us from studying specific psychotic experience sub-types, which were only measured as lifetime variables. We also cannot rule out whether some of the respondents who reported psychotic experiences actually had a diagnosable psychotic disorder. Given that this study was a secondary analysis, we were unable to use ideal variables for each construct we tested. In a prior study, we had the freedom to choose the measures and found these factors to fully explain the associations between psychotic experiences and suicidal behaviors [6]; however, that study was a non-probability convenience sample of college students.
Implications
The rationale for explicating the relationship between psychotic experiences and suicide, independent of commonly co-occurring risk factors and co-morbidities, is twofold. First, independent associations between psychotic experiences and suicide-related outcomes would suggest that psychosis screens may be used clinically to improve the predictive validity of suicide prevention efforts. The independent association between psychotic experiences and suicide attempts in the current study has already been confirmed in a cross-sectional clinical sample [18], and we are currently testing whether a brief psychotic screen can be used in conjunction with a brief suicide screen to improve the prediction of subsequent suicidal behavior in a longitudinal clinical sample.
The second major implication is that understanding the nature of the relationship between psychotic experiences and suicide may also inform our understanding of suicide risk associated with clinical psychosis. Efforts to address risk for suicide in psychosis have often focused on characteristics of psychosis itself, such as the presence of command hallucinations [8, 30] or the role of insight [4]. However, our finding that some of the association between psychosis and suicide may be driven by common psychiatric comorbidities implies that suicide prevention efforts in schizophrenia may likewise benefit from a focus on co-occurring symptoms, such as depression or anxiety. Subsequent work has suggested that depression may be the factor underlying the associations between insight and suicide risk in schizophrenia [25]. Further, this is consistent with prior work showing that depression, and particularly how one reacts to depression, is a major distinguishing factor separating people with schizophrenia who do and do not attempt suicide [9].
Conclusion
In adjusting for a wide range of previously identified confounders and mediators, the association between psychotic experiences and suicidal ideation was no longer significant. However, even after extensive adjustment, psychotic experiences remained significantly associated with suicide attempts. Previous longitudinal studies have shown that psychotic experiences precede suicide attempts [17, 26]. Together, this suggests that psychotic experiences should routinely be included in mental health assessments to improve the identification of those individuals most at risk of attempting suicide, as the predictive value associated with psychotic experiences appears to be independent of other common risk factors and co-morbidities.
References
Amrhein V, Greenland S, McShane B (2019) Scientists rise up against statistical significance. Nature 567:305–307
Bromet EJ, Nock MK, Saha S, Lim CC, Aguilar-Gaxiola S, Al-Hamzawi A, de Girolamo G (2017) Association between psychotic experiences and subsequent suicidal thoughts and behavior: a cross-national analysis from the World Health Organization World Mental Health Surveys. JAMA Psychiatry 74(11):1136–1144
Calkins ME, Moore TM, Satterthwaite TD, Wolf DH, Turetsky BI, Roalf DR, Merikangas KR, Ruparel K, Kohler CG, Gur RC, Gur RE (2017) Persistence of psychosis spectrum symptoms in the Philadelphia Neurodevelopmental Cohort: a prospective 2-year follow-up. World Psychiatry 16:62–76
Crumlish N, Whitty P, Kamali M, Clarke M, Browne S, McTigue O, O'callaghan E (2005) Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr Scand 112(6):449–455
DeVylder JE, Lukens EP, Link BG, Lieberman JA (2015) Suicidal ideation and suicide attempts among adults with psychotic experiences: data from the collaborative psychiatric epidemiology surveys. JAMA Psychiatry 72(3):219–225
DeVylder JE, Jahn DR, Doherty T, Wilson CS, Wilcox HC, Schiffman J, Hilimire MR (2015) Social and psychological contributions to the co-occurrence of sub-threshold psychotic experiences and suicidal behavior. Soc Psychiatry Psychiatr Epidemiol 50(12):1819–1830
Fazel S, Wolf A, Palm C, Lichtenstein P (2014) Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: a 38-year total population study in Sweden. Lancet Psychiatry 1(1):44–54
Harkavy-Friedman JM, Kimhy D, Nelson EA, Venarde DF, Malaspina D, Mann JJ (2003) Suicide attempts in schizophrenia: the role of command auditory hallucinations for suicide. J Clin Psychiatry 64(8):871–874
Harkavy-Friedman JM, Restifo K, Malaspina D, Kaufmann CA, Amador XF, Yale SA, Gorman JM (1999) Suicidal behavior in schizophrenia: characteristics of individuals who had and had not attempted suicide. Am J Psychiatry 156(8):1276–1278
Hielscher E, Connell M, Lawrence D, Zubrick SR, Hafekost J, Scott JG (2018) Association between psychotic experiences and non-accidental self-injury: results from a nationally representative survey of adolescents. Soc Psychiatry Psychiatr Epidemiol 54:1–10
Hielscher E, DeVylder JE, Saha S, Connell M, Scott JG (2018) Why are psychotic experiences associated with self-injurious thoughts and behaviours? A systematic review and critical appraisal of potential confounding and mediating factors. Psychol Med 48(9):1410–1426
Honings S, Drukker M, van Nierop M, van Winkel R, Wittchen HU, Lieb R, van Os J (2016) Psychotic experiences and incident suicidal ideation and behaviour: disentangling the longitudinal associations from connected psychopathology. Psychiatry Res 245:267–275
Honings S, Drukker M, Groen R, van Os J (2016) Psychotic experiences and risk of self-injurious behaviour in the general population: a systematic review and meta-analysis. Psychol Med 46(2):237–251
Hor K, Taylor M (2010) Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol 24(4_suppl):81–90
Ishii T, Hashimoto E, Ukai W, Kakutani Y, Sasaki R, Saito T (2014) Characteristics of attempted suicide by patients with schizophrenia compared with those with mood disorders: a case-controlled study in northern Japan. PLoS ONE 9(5):e96272
Kelleher I, Cederlöf M, Lichtenstein P (2014) Psychotic experiences as a predictor of the natural course of suicidal ideation: a Swedish cohort study. World Psychiatry 13(2):184–188
Kelleher I, Corcoran P, Keeley H, Wigman JT, Devlin RH, Wasserman D (2013) Psychotic symptoms and population risk for suicide attempt: a prospective cohort study. JAMA Psychiatry 70(9):940–948
Kelleher I, Devlin N, Wigman JT, Kehoe A, Murtagh A, Fitzpatrick C, Cannon M (2014) Psychotic experiences in a mental health clinic sample: implications for suicidality, multimorbidity and functioning. Psychol Med 44(8):1615–1624
Kessler RC, Adler LA, Barkley R, Biederman J, Conners CK, Faraone SV, Zaslavsky AM (2005) Patterns and predictors of ADHD persistence into adulthood: results from the National Comorbidity Survey Replication. Biol Psychiatry 5(11):1442–1451
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Ggroerer JC, Hiripi E, Zaslavsky AM (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60:184–189
Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Zheng H (2004) The US national comorbidity survey replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res 13(2):69–92
Kessler RC, Üstün TB (2004) The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) composite international diagnostic interview (CIDI). Int J Methods Psychiatr Res 13(2):93–121
Klonsky ED, May AM (2015) The three-step theory (3ST): a new theory of suicide rooted in the “ideation-to-action” framework. Int J Cognit Ther 8(2):114–129
Linscott RJ, Van Os J (2013) An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med 43(6):1133–1149
López-Moríñigo JD, Ramos-Ríos R, David AS, Dutta R (2012) Insight in schizophrenia and risk of suicide: a systematic update. Compr Psychiatry 53(4):313–322
Martin G, Thomas H, Andrews T, Hasking P, Scott JG (2015) Psychotic experiences and psychological distress predict contemporaneous and future non-suicidal self-injury and suicide attempts in a sample of Australian school-based adolescents. Psychol Med 45(2):429–437
Murphy J, Shevlin M, Hyland P, Christoffersen M, Elklit A, Bentall R (2018) Reconsidering the association between psychosis and suicide: a suicidal drive hypothesis. Psychosis 10(4):286–297
Nishida A, Tanii H, Nishimura Y, Kajiki N, Inoue K, Okada M, Sasaki T, Okazaki Y (2008) Associations between psychotic-like experiences and mental health status and other psychopathologies among Japanese early teens. Schizophr Res 99:125–133
Nock MK, Kessler RC (2006) Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol 115(3):616
Rogers P, Watt A, Gray NS, MacCulloch M, Gournay K (2002) Content of command hallucinations predicts self-harm but not violence in a medium secure unit. J Forensic Psychiatry 13(2):251–262
Selten JP, van der Ven E, Rutten BP, Cantor-Graae E (2013) The social defeat hypothesis of schizophrenia: an update. Schizophr Bull 39(6):1180–1186
Shrivastava A, Johnston ME, Shah N, Innamorati M, Stitt L, Thakar M, Pompili M (2010) Persistent suicide risk in clinically improved schizophrenia patients: challenge of the suicidal dimension. Neuropsychiatr Dis Treat 6:633
Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr (2010) The interpersonal theory of suicide. Psychol Rev 117(2):575
Yates K, Lång U, Cederlöf M, Boland F, Taylor P, Cannon M, Kelleher I (2019) Association of psychotic experiences with subsequent risk of suicidal ideation, suicide attempts, and suicide deaths: a systematic review and meta-analysis of longitudinal population studies. JAMA Psychiatry 76(2):180–189
Acknowledgements
This research was supported by a young investigator Grant from the American Foundation for Suicide Prevention (Grant YIG-1-042-16 to Dr. DeVylder). Emily Hielscher is supported by the Dr. F and Mrs. ME Zaccari Scholarship, Australia. James Scott is supported by a National Health and Medical Research Council Practitioner Fellowship Grant APP1105807 and is employed by the Queensland Centre for Mental Health Research which receives core funding from Queensland Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
DeVylder, J., Waldman, K., Hielscher, E. et al. Psychotic experiences and suicidal behavior: testing the influence of psycho-socioenvironmental factors. Soc Psychiatry Psychiatr Epidemiol 55, 1167–1177 (2020). https://doi.org/10.1007/s00127-020-01841-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01841-9